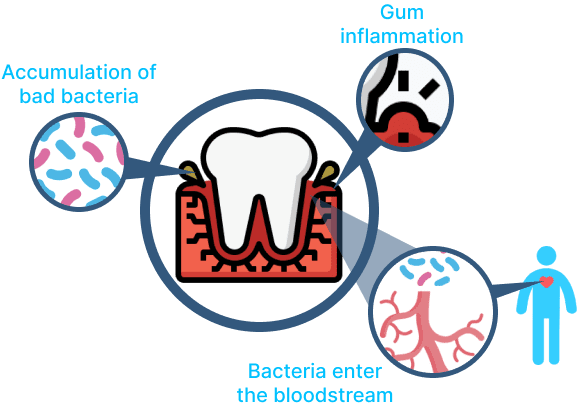
Many studies have shown the close relationship between dental health (teeth and gums) and our general well-being.
Our teeth are connected to our body through the bloodstream. Bacteria present in dental conditions such as cavities and gum disease can enter the bloodstream and affect other organs in your body, such as the heart.
Therefore, good oral health care is not only important for maintaining healthy teeth and gums, but it also contributes to your overall well-being.
Tooth problems encompass conditions like tooth decay, fractures, and tooth wear, which can cause pain, discomfort, and shorten the tooth's life if left untreated.
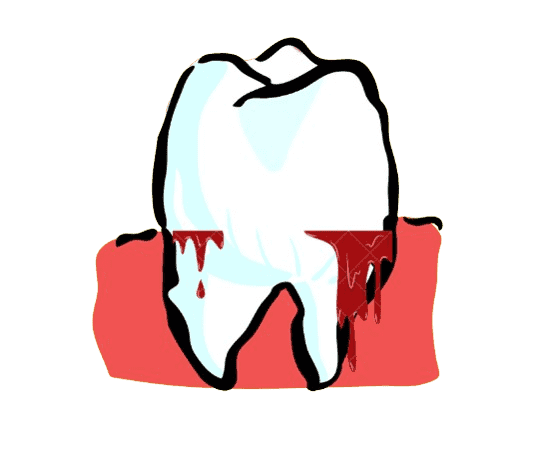
Gum disease, or periodontal disease, involves inflammation and infection of the tissues around the teeth. It begins with gingivitis, causing swollen, bleeding gums, and can progress to periodontitis, leading to gum recession, bone loss, and potential tooth loss.
Dental treatment and procedures cover a variety of services that aim to address oral health issues, restore dental health, and enhance aesthetics, ranging from routine cleanings and fillings to more complex interventions like implants and orthodontics.

Mouth conditions encompass a range of issues that can affect oral health, including canker sores, oral thrush, dry mouth, and bad breath. These conditions can cause discomfort, pain, and impact overall well-being.
Restorative dentistry focuses on repairing and restoring the function and appearance of damaged or missing teeth. It includes procedures such as fillings, crowns, bridges, and veneers.

Prevention plays a vital role in maintaining good oral health and avoiding dental issues. By practicing regular and thorough oral hygiene, you can reduce the risk of tooth decay, gum disease, and other oral problems.
Hello, I am Ayoub, a graduate of a dental internship with 4 years of practice. I am currently pursuing my PhD and enjoy sharing my knowledge and ideas about dentistry and oral health.
I am passionate about web development, writing and medical research. All of this has inspired me to launch Tooth Life in 2019, with the main goal of helping and educating others about the importance of oral health.
I've learned and improved a lot at what I do. My goal now is to offer the greatest possible value to my readers.