I Have a Hole in My Tooth with No Pain. Am I Safe?
A hole in your tooth, even if it isn’t causing pain, doesn’t mean it should be ignored or that you’re safe.
It could be a sign that an infection is quietly developing, progressing slowly without noticeable symptoms. Often, you might not realize it until it suddenly flares up and becomes much more serious.
Painful or not, a tooth cavity should never be ignored. The longer you wait, the more complex the situation can become.
If you have a hole in your tooth without pain, don’t worry—we’ll break down the possible causes, how it can progress if untreated, and the right steps to take.
It could be a sign that an infection is quietly developing, progressing slowly without noticeable symptoms. Often, you might not realize it until it suddenly flares up and becomes much more serious.
Painful or not, a tooth cavity should never be ignored. The longer you wait, the more complex the situation can become.
If you have a hole in your tooth without pain, don’t worry—we’ll break down the possible causes, how it can progress if untreated, and the right steps to take.
In this article:
1. Does Tooth Cavity Always Mean Pain?
2. A Painless Hole in My Tooth: What's the Possible Causes
3. A Hole in a Tooth Isn't Always a Cavity
4. How Can an Untreated Hole Due to a Cavity Progress?
5. Treating a Painless Hole in a Tooth: What's the Options?
Does Tooth Cavity Always Mean Pain?
When cavities advance, they form holes in the teeth, often bringing that sharp, short pain triggered by cold, hot, or sweet foods and drinks. However, that's not always the case.A cavity can sometimes be sneaky and symptom-free, without the usual discomfort.
And no pain isn’t necessarily a good thing. Why? Because it’s like the tooth’s alarm system is turned off. This allows the cavity to progress silently, without you noticing.
You might only discover it during a routine dental checkup—or worse, when it has already advanced and caused an infection or abscess.
A Painless Hole in My Tooth: What's the Possible Causes
A painless hole in a tooth usually points to one of two situations:- The damage is only at the surface, limited to the enamel (the outer layer of the tooth), which doesn’t have nerves.
- The damage has reached the nerves and caused so much damage that the tooth is no longer alive. When the pulp—the soft tissue inside the tooth that contains nerves and blood vessels—is completely destroyed, it leads to a condition called necrosis, leaving the tooth completely insensitive.
Here’s a breakdown of these two situations:
1. The Damage is Limited to the Enamel Layer
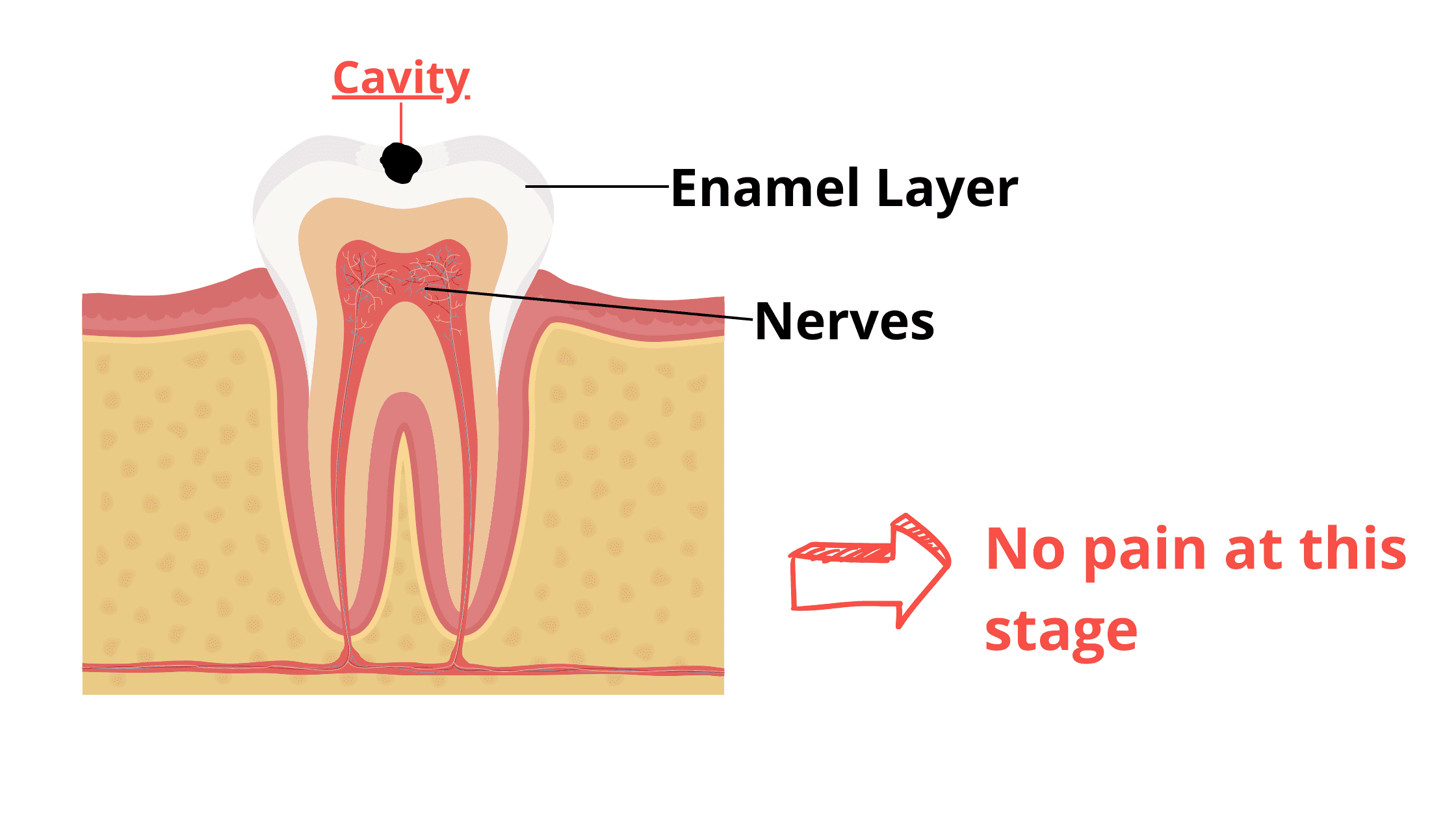
Enamel is the hardest tissue in your body. Its main job is to protect your teeth from outside stressors like bacteria and chewing pressure.
When decay sets in, it starts to affect the outer enamel layer. Early signs are often mild and very shallow, appearing as white or brown chalky spots on the tooth.
As decay progresses, the tooth loses more minerals, and the early spots can develop into deeper holes or cavities. But cavities limited to the enamel are still superficial, usually less than 1 mm deep.
You won’t feel any pain at this stage, as enamel has no nerves.
The good news? Damage at this stage is completely reversible by simply improving your oral hygiene, balancing your diet, and using remineralizing treatments.
The bad news is that enamel cavities are easy to miss. If left untreated, decay will reach the next layer—dentin—where cavities become more extensive and require professional dental treatment.
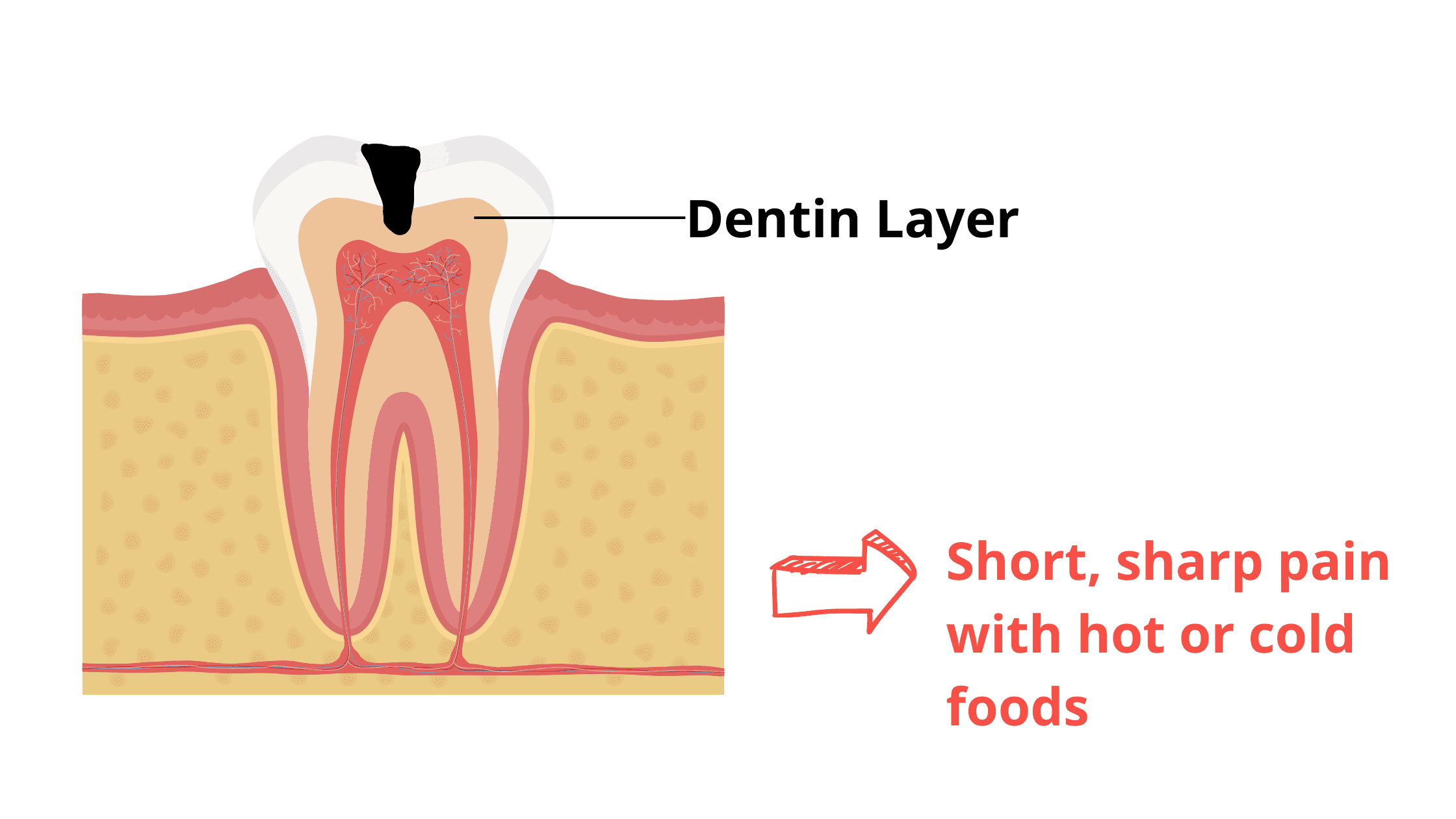
Once the cavity reaches the dentin layer, your tooth may become more sensitive and painful, especially when exposed to hot, cold, sweet, or acidic foods and drinks.
2. The Pulp Necrosis Scenario
While a painless hole can indicate mild, superficial damage, it may also signal a more serious situation where the nerves are severely affected, causing the tooth to die.
When decay or a cavity reaches the pulp, it triggers intense inflammation to fight off the invading bacteria. This increases pressure inside the tooth, compressing the nerves and causing a throbbing toothache.
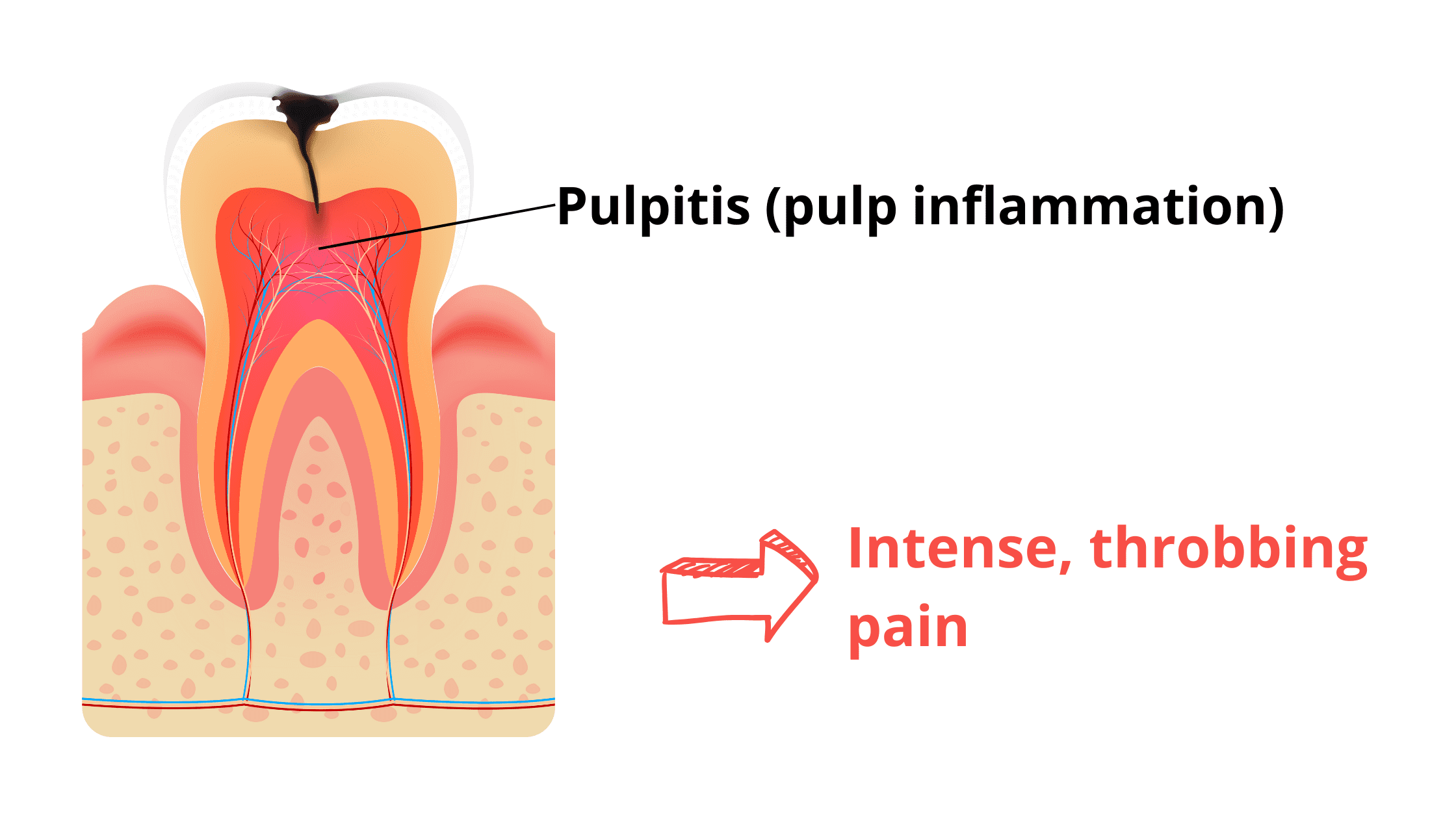
This pain is often temporary because the pressure can also compress the tiny blood vessels, cutting off the tooth’s blood supply. Without oxygen and nutrients, the pulp dies, and the tooth becomes completely insensitive.
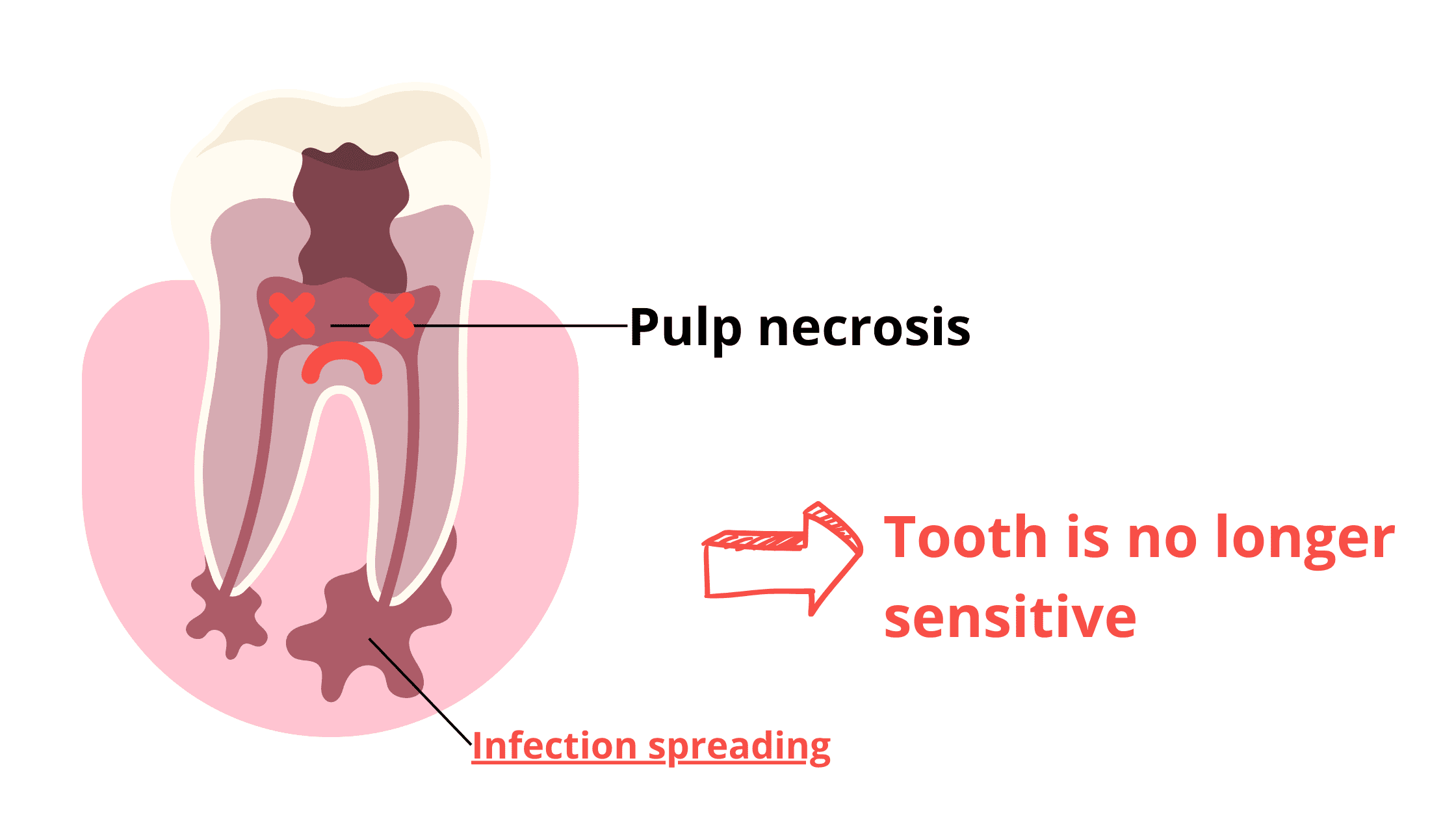
A common sign of this is the tooth gradually darkening, turning grayish or bluish as the blood vessels inside break down.
But no pain doesn’t mean the tooth is healed. It's actually a more serious problem: without the pulp to contain the infection, bacteria can spread deeper into surrounding tissues, like the gums, bone, and even the face. If left untreated, the bacteria will continue to spread further, potentially leading to severe infections.
A Hole in a Tooth Isn't Always a Cavity
Not all holes in teeth are caused by cavities. While cavities are the most common culprit, other dental issues can also lead to tooth damage:- Dental fractures: These occur when a crack develops on the tooth surface or a piece of the tooth breaks off. The most common causes are trauma from accidents, a hard blow, or biting down on something too hard.
- Dental wear: This happens when the outer hard layers of the teeth gradually break down and thin out. Common causes include teeth grinding or clenching (bruxism), excessive friction from a hard object (like a stiff toothbrush), or repeated acid exposure from vomiting, acid reflux, or consuming acidic foods and drinks.
Left untreated, all of these dental conditions can have serious consequences for your teeth and overall oral health.
How Can an Untreated Hole Due to a Cavity Progress?
A hole or any damage to a tooth should never be ignored or postponed.Once tooth structure is lost, it cannot heal on its own—it can only get worse.
Even more concerning, the damage creates a perfect entry point for bacteria to reach deep inside the tooth and surrounding tissues.
Healthy teeth are perfectly protected from harmful bacteria by strong enamel and dentin layers. That's no longer the case when a cavity or hole breaks this shield.
If left untreated, bacteria can invade the tooth nerves and spread to the underlying bone and gums, forming an abscess.
From there, the infection can reach soft facial tissues, causing severe pain and swelling. In extreme cases, it may even reach vital areas like the upper airways, leading to difficulty breathing. Some situations can even be life-threatening.
This isn’t meant to scare you—it’s to show why treating dental issues early is so important. Early treatment is safer, easier, more effective, and less costly.
Treating a Painless Hole in a Tooth: What are the options?
When treating a hole or cavity in a tooth, the first thing we look at is the depth of the damage and the condition of the nerves.If the damage is superficial, limited to the enamel surface (appearing as a white or brown spot), it may be reversible with some simple measures, including:
- Thorough daily oral hygiene
- Limiting sugars and snacking between meals
- Using remineralizing products to complement your daily oral care
- Managing dry mouth by staying hydrated and chewing sugar-free gum between meals
When the damage has progressed into the dentin and formed a deep cavity, it is no longer reversible and requires professional treatment. Your dentist will remove the decayed tissue and restore the tooth with options like a dental filling or crown.
If the pulp or nerves are reached and badly damaged, a root canal is necessary before restoring the tooth. A root canal involves removing the damaged nerve, thoroughly cleaning the inside of the tooth, and sealing it to prevent future infections.
Once that's done, the next step is to restore the tooth with a crown or filling to regain its function and appearance.
As you can see, the more severe the damage, the more complex the treatment becomes. The best approach is to address any dental issue early to avoid the need for a root canal, which, although generally successful, can weaken the tooth further and shorten its overall lifespan.