6 Common Reasons to Remove Your Wisdom Tooth
 There’s a common myth that all wisdom teeth should be removed no matter what. They’re often seen as useless leftovers that only take up space. So, why keep them?
There’s a common myth that all wisdom teeth should be removed no matter what. They’re often seen as useless leftovers that only take up space. So, why keep them?
Just like any other tooth, wisdom teeth don’t always need to be removed. If they’re healthy, not causing problems, and unlikely to cause issues in the future, wisdom teeth can help you chew your food just like your other molars.
The reason these teeth often get blamed is because they’re the last to come in—usually in your late teens or early twenties. By then, there’s often not enough space left in your mouth, which can lead to problems like pain, infection, gum disease, and cavities.
In this article, we’ll break down 6 common reasons why your wisdom tooth might need to be removed.
In this article...
1. Prevent Bone Loss and Gum Disease
2. Pericoronitis (Infection of the Gum Over a Wisdom Tooth)
3. Prevent Tooth Decay
4. Prevent Damage to the Roots of Nearby Teeth
5. Ulceration and Cheek Damage
6. Prevent or Treat a Cyst or Tumor Around the Wisdom Tooth
How to Know If a Wisdom Tooth Needs to Be Removed
Is There a Better Time to Extract a Wisdom Tooth?
1. To Prevent Bone Loss and Gum Disease
Wisdom teeth grow in a very tight area—right behind your second molars, the last teeth at the back of your mouth.
As they try to push their way in, they can press against the bone that supports your second molars, making it thinner and weaker. This increases the risk of gum disease, receding gums, and bone loss in that area.
As they try to push their way in, they can press against the bone that supports your second molars, making it thinner and weaker. This increases the risk of gum disease, receding gums, and bone loss in that area.
What makes things worse is that these back teeth are the hardest to keep clean. Plaque, food particles, and bacteria can easily build up there, creating the perfect conditions for gum inflammation.
Even mild inflammation behind your molars can open the door for bacteria to travel deep down into the gums and bone. This can lead to unnaturally wide spaces between your teeth and gums, called periodontal pockets, which form when the surrounding ligaments and bone start to break down.
Even mild inflammation behind your molars can open the door for bacteria to travel deep down into the gums and bone. This can lead to unnaturally wide spaces between your teeth and gums, called periodontal pockets, which form when the surrounding ligaments and bone start to break down.
If this continues, you could end up losing not just the wisdom tooth, but also the healthy tooth right in front of it.
Removing wisdom teeth early can help prevent all of this. It gives your gums and bone a chance to heal before the damage becomes irreversible and harder to treat.
Removing wisdom teeth early can help prevent all of this. It gives your gums and bone a chance to heal before the damage becomes irreversible and harder to treat.
2. Pericoronitis (Infection of the Gum Over a Wisdom Tooth)
When a wisdom tooth doesn’t fully erupt, it often ends up partially covered by gum tissue. Part of the tooth is visible, while the rest remains trapped beneath the gums.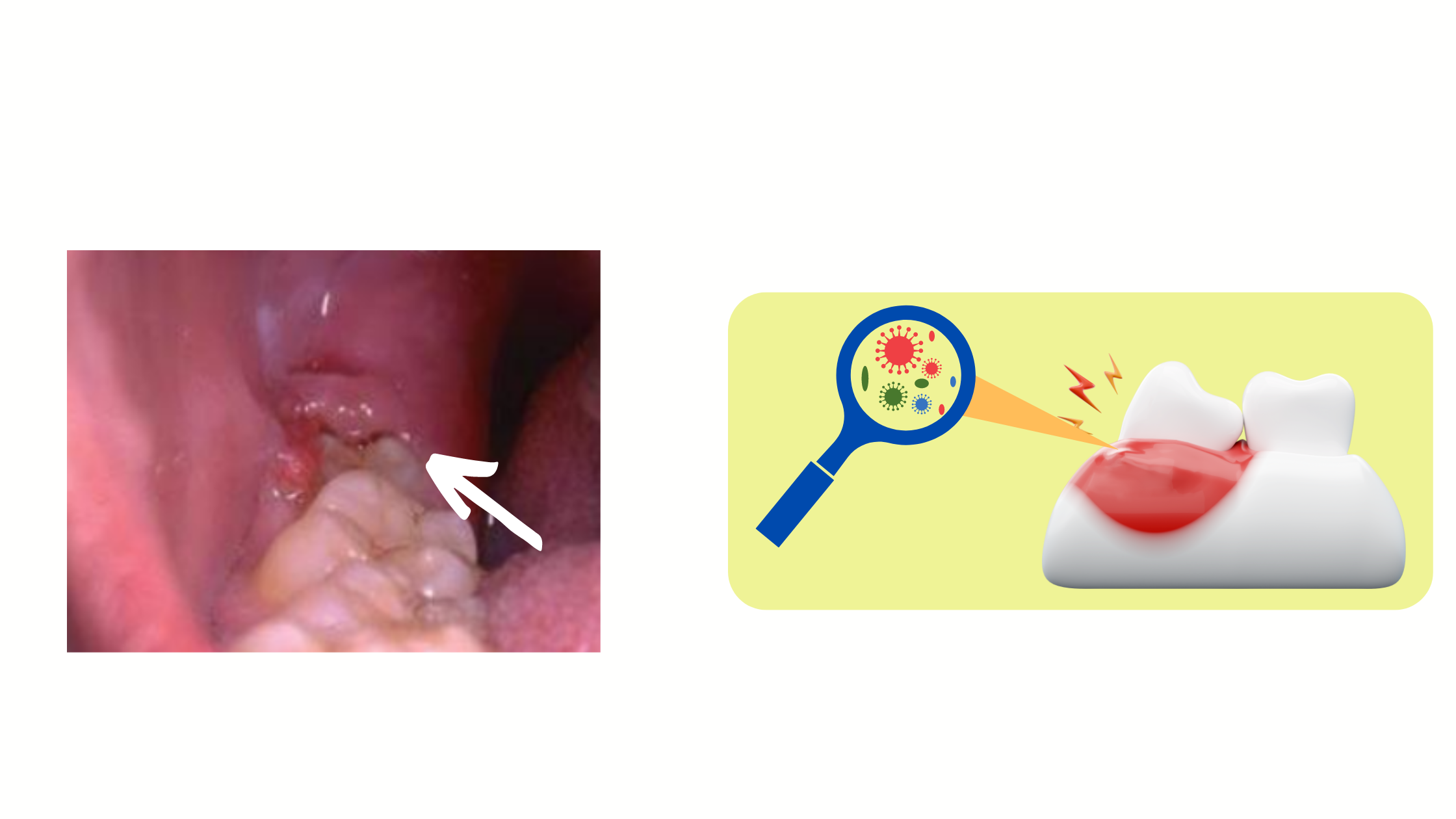
This abnormal position makes it easy for food and plaque to get stuck, making this area a breeding ground for bacteria. When the gum covering the tooth swells and becomes inflamed or infected, it leads to a condition called pericoronitis.
The telltale signs are red, swollen, and painful gums around the tooth, along with bad breath and sometimes difficulty opening the mouth. In more severe cases, you might also experience fever, facial swelling, and a general feeling of being unwell.
If the symptoms keep coming back or don’t go away with treatment, removing the wisdom tooth is often the best solution.
Often, the swollen gum becomes irritated by the opposing wisdom tooth from the other jaw constantly biting down on it. When this happens, the opposing tooth may also need to be removed.
3. To Prevent Tooth Decay
When a wisdom tooth is tilted or not properly aligned with the rest of your teeth, it’s much more likely to develop cavities. That’s because misaligned teeth tend to trap more plaque and are harder to brush and clean effectively.
Since wisdom teeth sit right next to your second molars, they often end up affecting them too.
If a wisdom tooth has not come in straight, it's often best to remove it as early as possible to prevent cavities that could damage both the wisdom tooth and the healthy molar next to it.
If a wisdom tooth has not come in straight, it's often best to remove it as early as possible to prevent cavities that could damage both the wisdom tooth and the healthy molar next to it.
4. To Prevent Damage to the Roots of Nearby Teeth
Wisdom teeth can grow at an angle toward the roots of the second molars. As they advance, they can put a lot of pressure on the roots and eat away at them.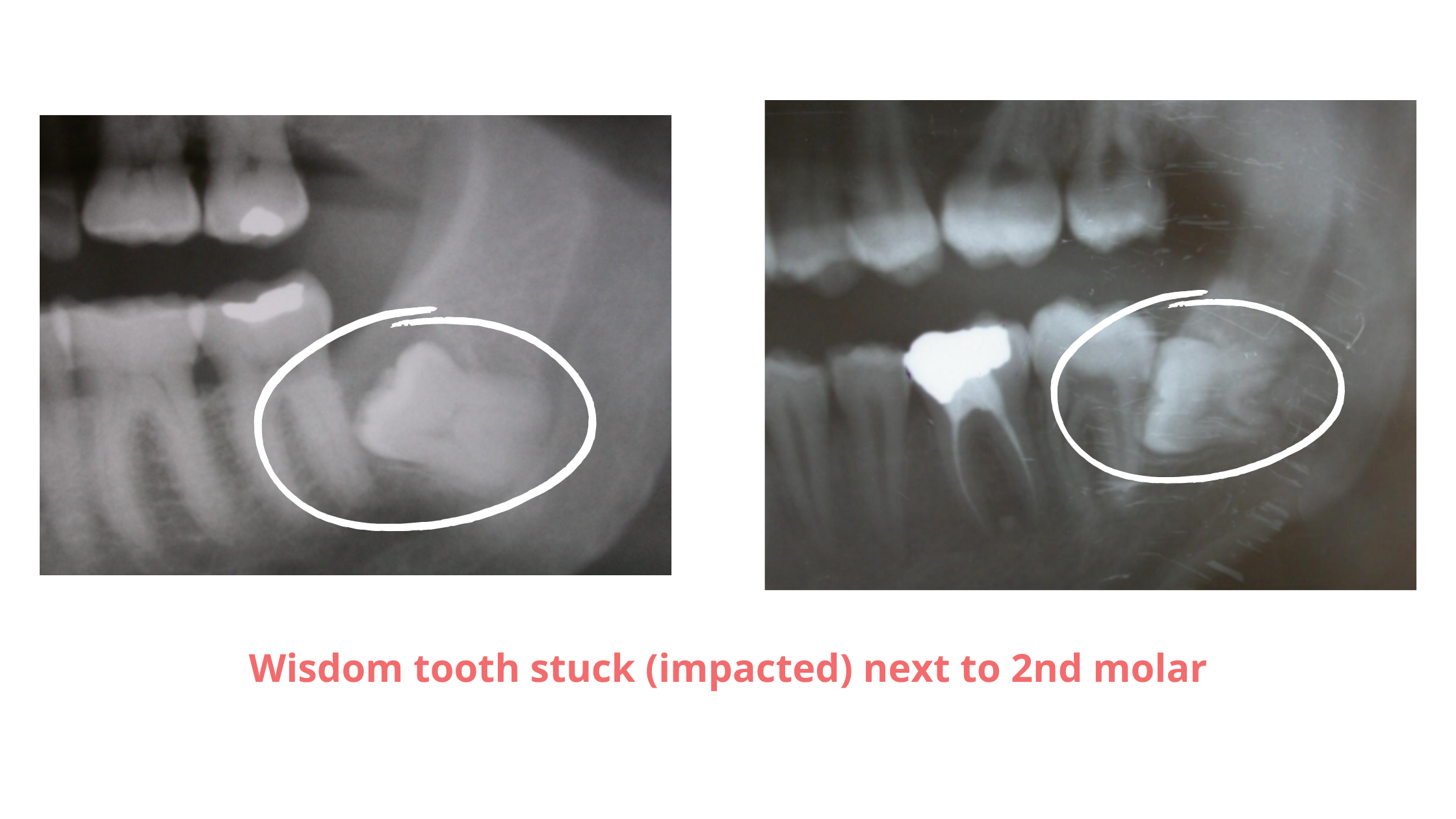
This is one of the most unfortunate situations where the roots of your second molars can become too short, causing the tooth to loosen and eventually fall out. This means you could lose both your wisdom tooth and the healthy tooth in front of it.
The best way to avoid such serious damage is to extract the wisdom tooth at an early stage, before it even touches the adjacent tooth.
5. Ulceration and Cheek Damage
When a wisdom tooth is tilted so that its sharp chewing surface constantly rubs or presses against the inside of your cheek, it can lead to irritation, injuries, and even painful ulcers.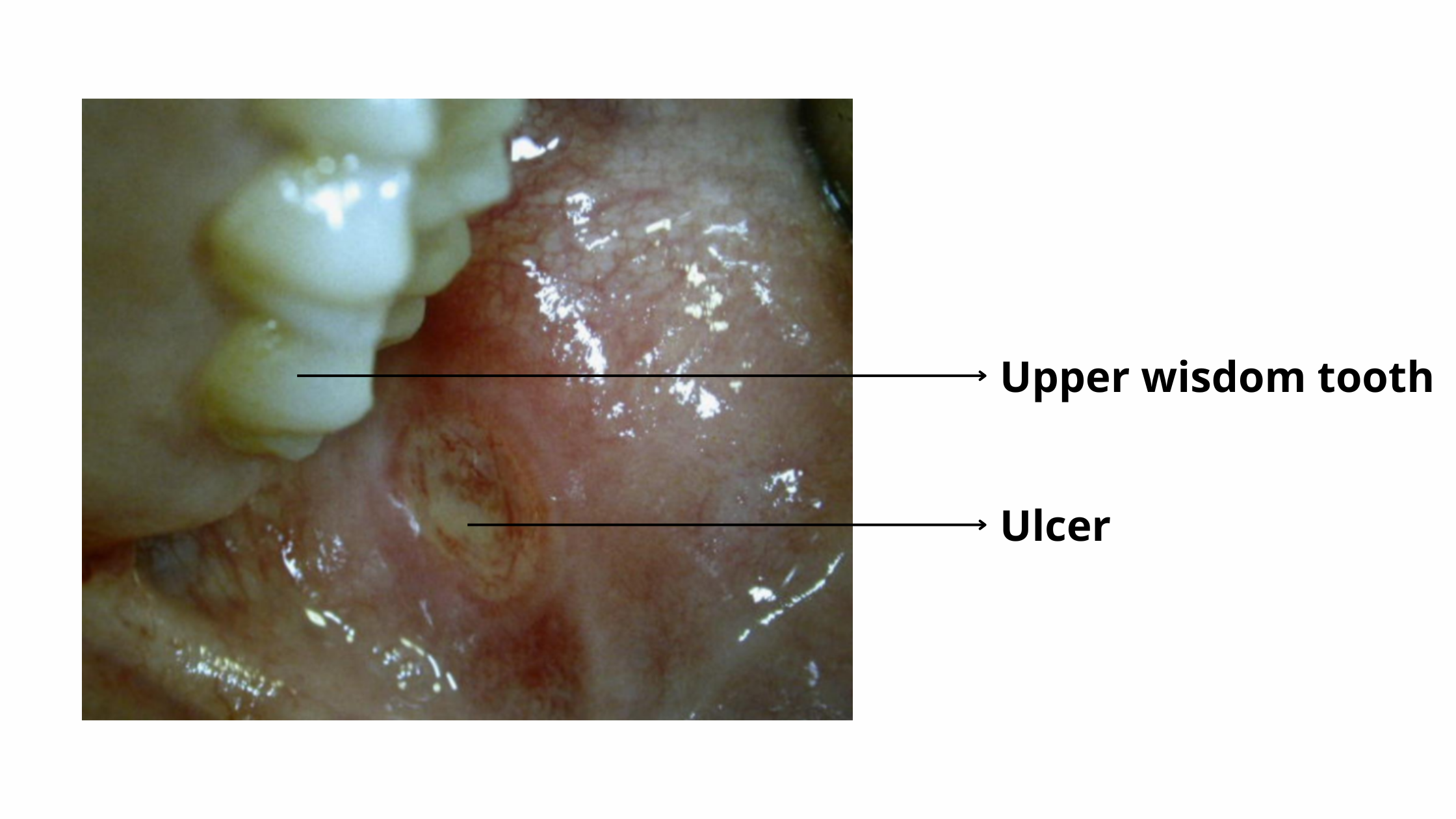
This can be so uncomfortable that it can affect your ability to eat, speak, or enjoy your meals.
If the tooth can’t be reshaped or its sharp edges smoothed out, removing it is often the best way to stop the irritation.
6. To Prevent or Treat a Cyst or Tumor Around the Wisdom Tooth
Although rare, abnormal growths like cysts or tumors can sometimes form around a wisdom tooth—especially if the tooth is impacted (stuck within the jawbone).Impacted wisdom teeth are the teeth most commonly associated with jaw tumors and cysts.
These growths often develop slowly and silently, with no noticeable symptoms at first. But as they grow, they can cause swelling, distort the jawbone, and even press on nearby nerves—leading to pain and discomfort.
Most of these lesions are benign (non-cancerous) and can be successfully treated by surgically removing both the wisdom tooth and the growth around it.
How to Know If a Wisdom Tooth Needs to Be Removed
The key rule to remember is simple: if the wisdom tooth is properly aligned, symptom-free, and unlikely to cause problems in the future, there’s no benefit to removing it. Extraction would only leave you with one less tooth.
The decision to remove a wisdom tooth first depends on whether it's fully emerged or impacted.
The decision to remove a wisdom tooth first depends on whether it's fully emerged or impacted.
Fully Emerged Wisdom Tooth
For teeth that have fully erupted above the gum line, there are two main things we look at: position and angulation.
If the tooth is straight and has enough space to fit, it should be left in place.
If the tooth is straight and has enough space to fit, it should be left in place.
A common scenario is when the wisdom tooth is partially covered by gum and tilted toward the adjacent molar. This position often traps bacteria and food, making the gum inflamed and prone to recurring infections. If the infection is severe or keeps coming back despite treatment, removal is usually the best option.
Another common situation is when the tooth is misaligned with your bite and constantly injures your cheek or tongue. If reshaping the tooth doesn’t help, extraction might be the most comfortable solution.
Another common situation is when the tooth is misaligned with your bite and constantly injures your cheek or tongue. If reshaping the tooth doesn’t help, extraction might be the most comfortable solution.
Impacted Wisdom Tooth
If the wisdom tooth is trapped inside the jawbone, there's no way you can tell whether it needs to be removed just by looking at it. Your dentist will need to take a dental X-ray to check:
- The position and angle of the tooth
- Its proximity to nearby nerves
- Whether it's affecting or threatening nearby teeth
- An infection or cyst
If the impacted tooth isn’t causing any symptoms and is positioned away from other structures, there may be no need to remove it.
However, if the X-ray reveals a bad position that could lead to serious problems later—like root damage, cyst formation, or gum disease—then early removal might be the wiser choice.
Before deciding on surgery, your dentist will always weigh the benefits and risks of the procedure, as sometimes it can be complex and carry certain risks.
Is There a Better Time to Extract a Wisdom Tooth?
In general, removing wisdom teeth that are impacted in the bone is much more difficult than extracting those that are fully visible. This is because the procedure often requires drilling into the surrounding bone to access the tooth.
The best time to remove impacted wisdom teeth is typically between 18 and 25 years old. At this time, the procedure is usually easier and the risk of complications is much lower.
The best time to remove impacted wisdom teeth is typically between 18 and 25 years old. At this time, the procedure is usually easier and the risk of complications is much lower.
At a younger age, the roots of the wisdom teeth are still short, and the surrounding bone is softer and more flexible. This makes the procedure more straightforward, and the healing process is usually quicker and smoother.
After the age of 30, things become a bit more complicated. The bone becomes stiffer and denser, and the roots are fully developed. This can make the extraction more challenging and raise the risk of complications and post-operative discomfort.
After the age of 30, things become a bit more complicated. The bone becomes stiffer and denser, and the roots are fully developed. This can make the extraction more challenging and raise the risk of complications and post-operative discomfort.
That’s why, if your dentist believes the tooth will eventually need to be removed, it’s often best to do it sooner rather than later. Delaying extraction until later in life can only make the procedure more complex and result in a longer and more uncomfortable recovery period.