The stages of a gum abscess and its healing process
So you have recently noticed a small swelling in your gums, which makes you think you have a gum abscess.
A gum abscess occurs when an infection in the tooth or surrounding tissue becomes difficult for the body to handle.
It is important to know that there are no hard and fast rules regarding the stages an abscess can go through. This is because our bodies and immune systems are different, and what happens to others may not apply to you.
In this article, we will look at the two most common types of gum abscesses, the different stages they can go through, and their potential complications.
In this article:
1. How does a gum abscess occur?
2. Periapical abscess: the different stages
3. Periodontal abscess: the different stages
4. Gum abscess treatment
5. The healing stages and recovery
6. Other types of gum abscesses
7. The potential complications of a gum abscess
8. Symptoms to look out for
9. Takeaway
How does a gum abscess occur?
 A gum abscess happens when your body reacts to harmful bacteria with a strong inflammatory response. This creates a pocket of pus made up of bacteria, dead cells, and other by-products of inflammation.
A gum abscess happens when your body reacts to harmful bacteria with a strong inflammatory response. This creates a pocket of pus made up of bacteria, dead cells, and other by-products of inflammation.
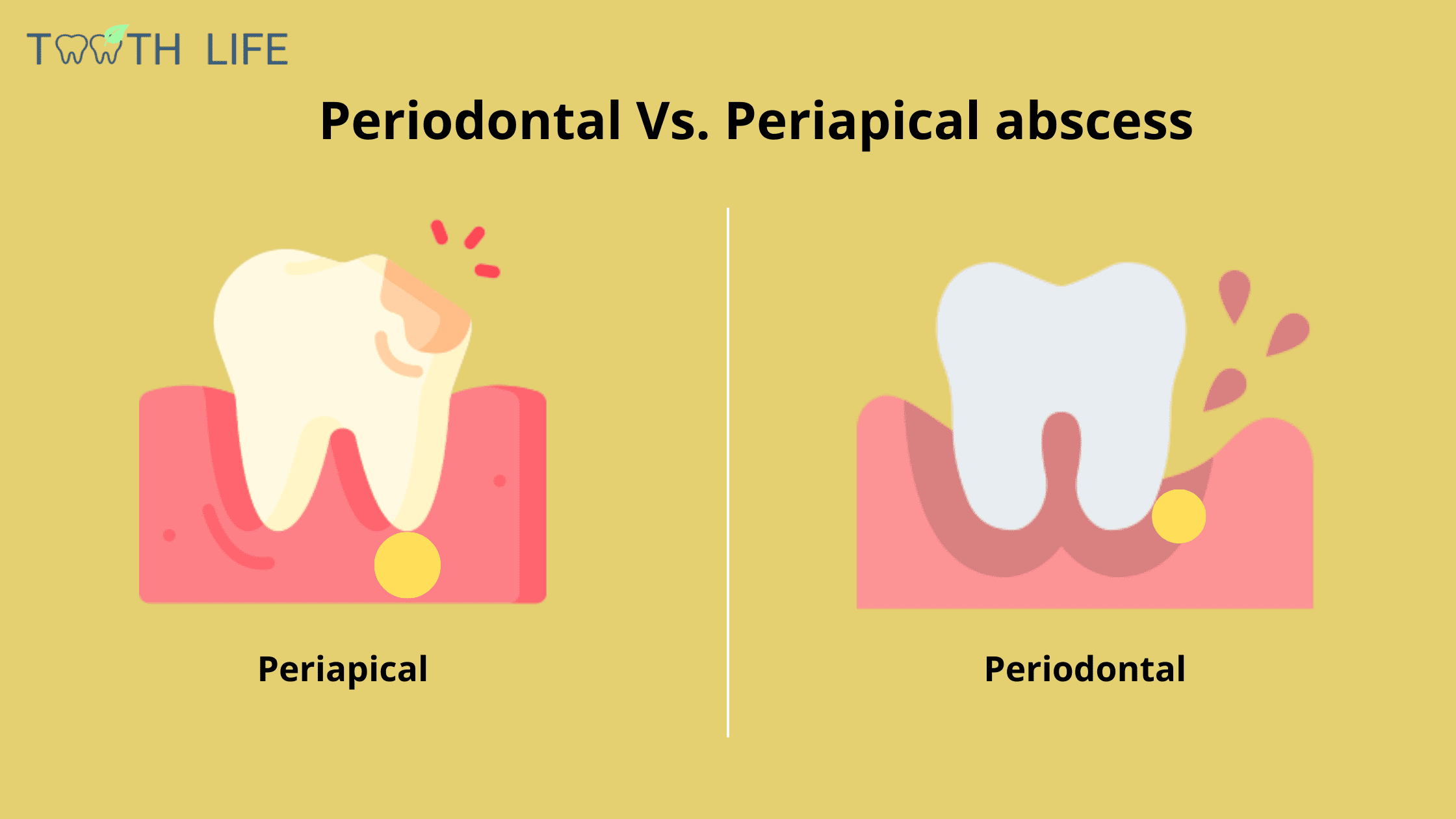
There are two main dental problems that can lead to this kind of infection: a periapical abscess and a periodontal abscess.
Both develop in a similar way—the main difference is simply where the infection starts.
1. Periapical abscess
A periapical abscess is an infection that starts inside the tooth. It typically develops when a cavity or a crack lets bacteria reach the tooth’s nerve (pulp), allowing the infection to spread to the tip of the root (see picture below).
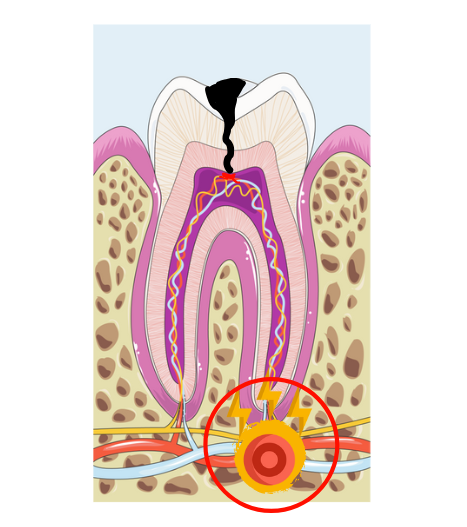
The area around the root tip is called the periapex, which is where the term “periapical abscess” comes from. That's the most common form of dental abscess.
2. Periodontal abscess
A periodontal abscess doesn’t come from an infection in the tooth’s nerves and doesn’t involve the inside of the tooth. Instead, it’s caused by an infection in the tissues that surround and support the tooth—known as the periodontal tissues (see image below).
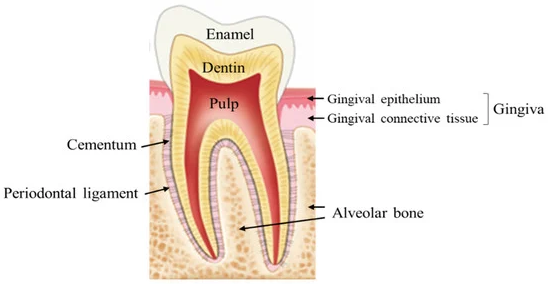
These tissues include the bone, ligaments, gums, and cementum. In gum disease, harmful bacteria can invade deep into these areas, triggering severe inflammation. This may lead to a build-up of pus and a visible swelling in the gum, called a periodontal abscess. It's the second most common form of dental abscess.
Both periapical and periodontal abscesses can cause visible swelling, commonly known as a gum boil.
In a periodontal abscess, the swelling usually appears near the gum line, while in a periapical abscess, it’s often further away, closer to the tip of the root.
Below is a breakdown of the stages of both periapical and periodontal abscesses.
Below is a breakdown of the stages of both periapical and periodontal abscesses.
Periapical abscess: the different stages
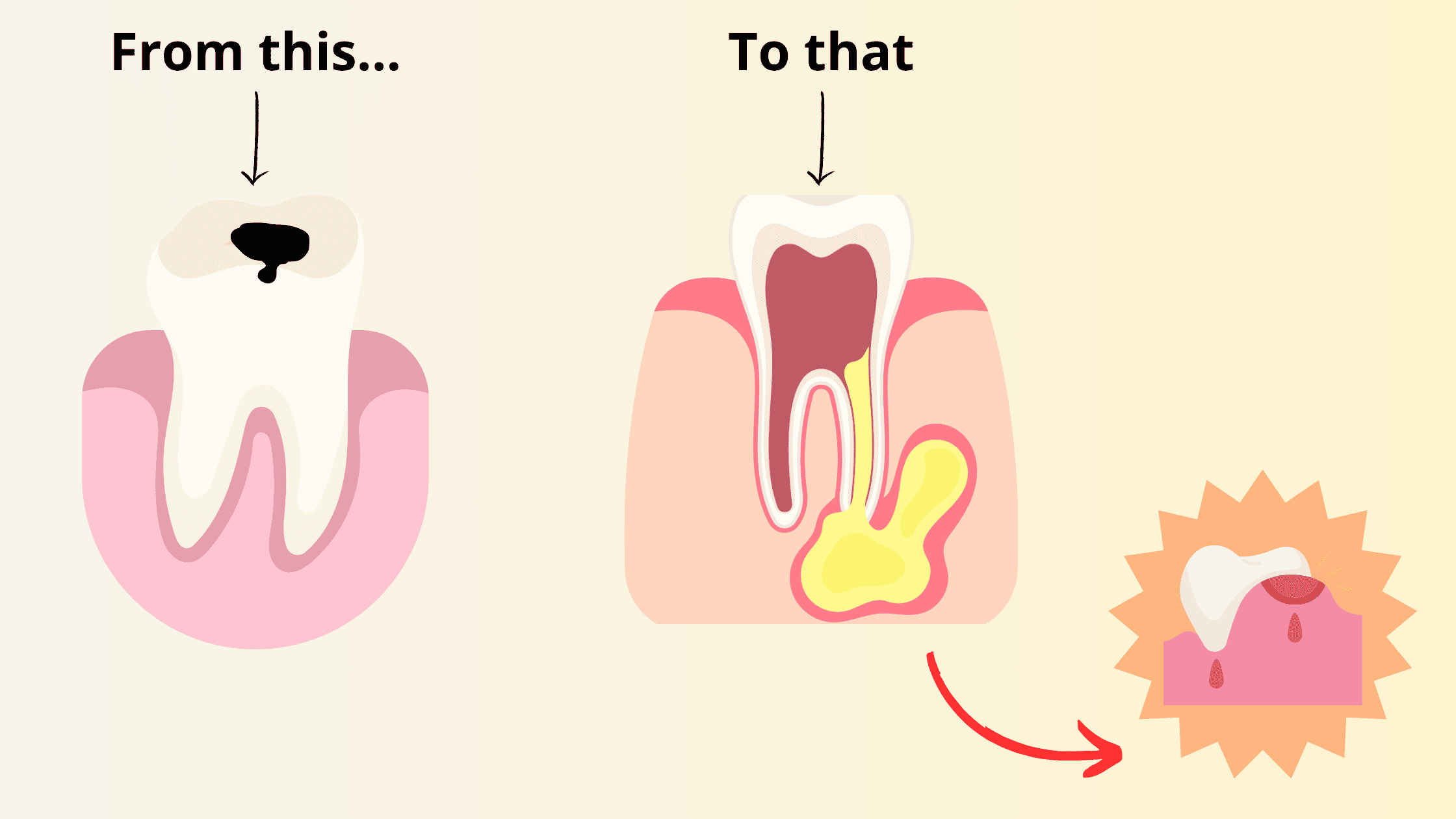
A periapical, or tooth abscess, develops when an abnormal opening allows bacteria from the mouth to reach the pulp inside the tooth. The most common cause is cavity or tooth decay.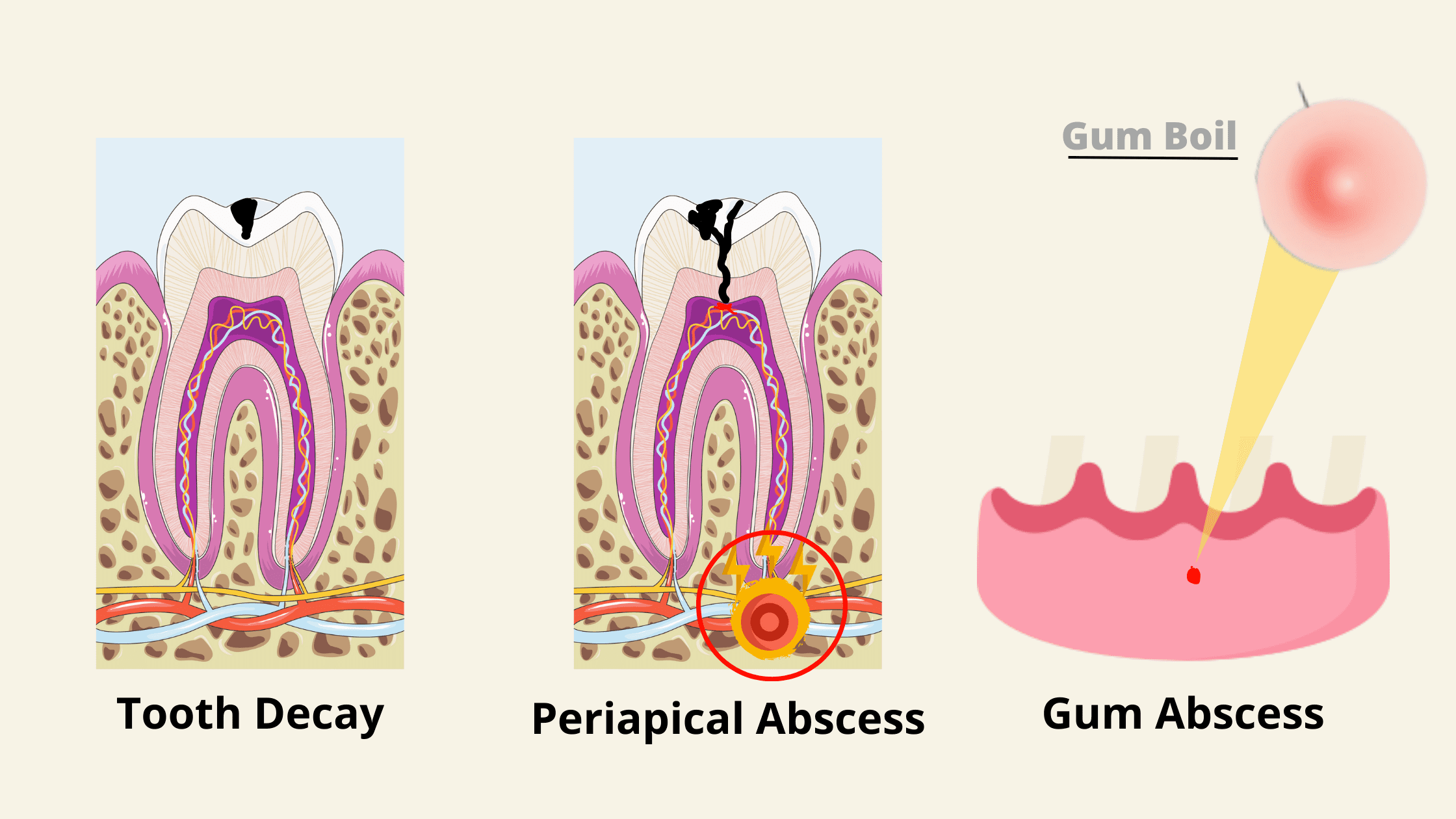 The typical stages of a periapical abscess are:
The typical stages of a periapical abscess are:
1. Tooth decay:
Tooth decay is one of the most common diseases worldwide. It doesn’t happen overnight but develops slowly, gradually eroding and destroying the tooth’s hard outer layers—the enamel and dentin. Here’s how tooth decay can progress if it’s left untreated:
1. Enamel decay:
Enamel is the outermost layer of the tooth and the hardest tissue in the body. Initially, it appears as white or brown spots on the tooth surface, which can still be stopped or even reversed with the right treatments.If left untreated, it can progress further to the underlying dentin layer, forming a hole or cavity.
2. Dentin decay:
When the decay reaches the dentin layer, it progresses faster, as dentin is softer and less resistant than enamel. The tooth may become very sensitive to cold, hot, or sweet foods.Dentin decay shows up as larger brown or black holes in the tooth. These damaged areas are permanent and must be treated by a dentist.
3. Pulp decay:
When decay progresses through the dentin layer and reaches the pulp, the nerve becomes inflamed and infected. The result is intense, throbbing pain.If left untreated, the infection can worsen and progress to the next stages.
2. Pulp death and early abscess:
When bacteria reach the pulp, your body responds by triggering inflammation to fight them off. But if this inflammation becomes too intense or lasts too long, it can actually cause more harm than good.
The increased pressure inside the pulp reduces blood flow and leads to pulp death (or necrosis).
Once the tooth is no longer alive, nothing can stop the bacteria from spreading further. They then move to the area around the root tip (periapical area) and cause a local infection called periapical periodontitis. This sets the stage for gum abscess.
Some people may not feel much pain at this point, while others might experience significant pain and swelling. It all depends on how quickly the infection settles and how your body reacts.
3. Periapical abscess and gum boil:
If periapical periodontitis is left untreated, the infection can form a pocket of pus at the root tip and transition into a full-blown abscess. At this stage, the pain can become so intense and unbearable that it may even keep you from sleeping.
The infection can damage the bone around the tooth, as well as the nearby gums. As it works its way out through the bone and gum, you may notice a small bump or pimple, commonly known as a gum boil.
Sometimes, the infection breaks through the gum and creates a small hole or channel called a fistula. This lets the pus drain out, which can reduce pressure and provide relief. But this doesn’t mean the infection is gone.
The bacteria involved in dental infections are tough and countless. As long as the source of the infection isn’t treated, the abscess will keep coming back.
Periodontal abscess: the different stages
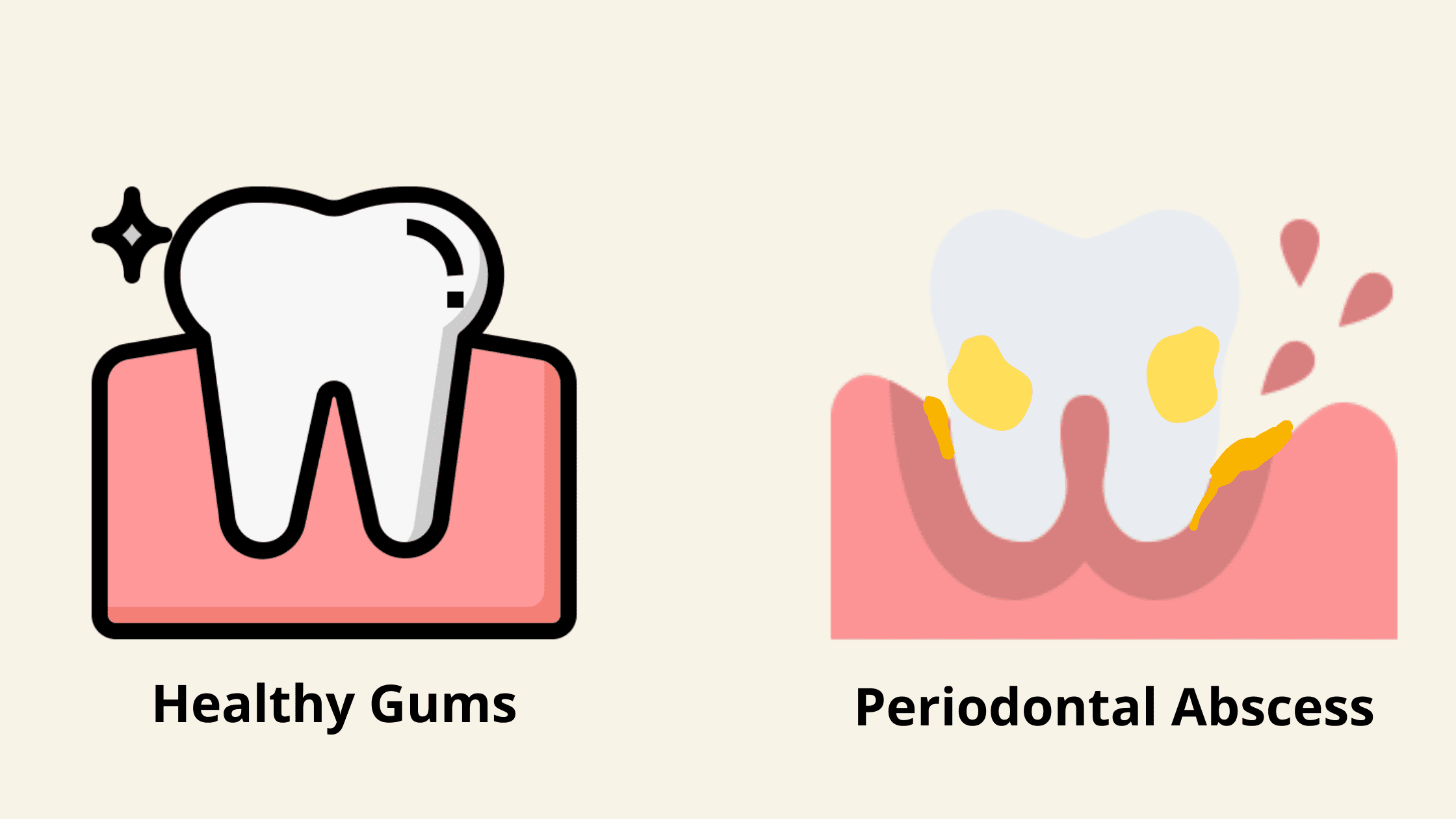 What makes a periodontal abscess different is that it can develop even if the tooth looks healthy and has no decay.
What makes a periodontal abscess different is that it can develop even if the tooth looks healthy and has no decay.
As we said, in periodontal abscess, the infection doesn’t affect the tooth’s nerves or pulp at all. It’s usually caused by aggressive gum disease, where the deeper tissues that support the tooth become infected.
The stages of a periodontal abscess include:
1. Gum inflammation (gingivitis):
Gum inflammation can develop after just a few days of skipping brushing and flossing.This allows bacteria to build up and form plaque, which can then penetrate the gum line, causing the classic signs of inflammation: redness, swelling, tenderness, and bleeding.
As long as the inflammation is limited to the gums, the damage is completely reversible. Treatment mainly involves improving oral hygiene at home and removing plaque and tartar.
2. Periodontitis:
If left untreated, inflammation can progress to the deeper tissues, including the bone. This stage is known as periodontitis.Many factors can cause gingivitis to develop into periodontitis, including genetics, poor oral hygiene, smoking, and some medical conditions.
The bacteria that cause periodontitis are more aggressive. They invade the space between the teeth and gums, making it larger and forming what we call periodontal pockets.
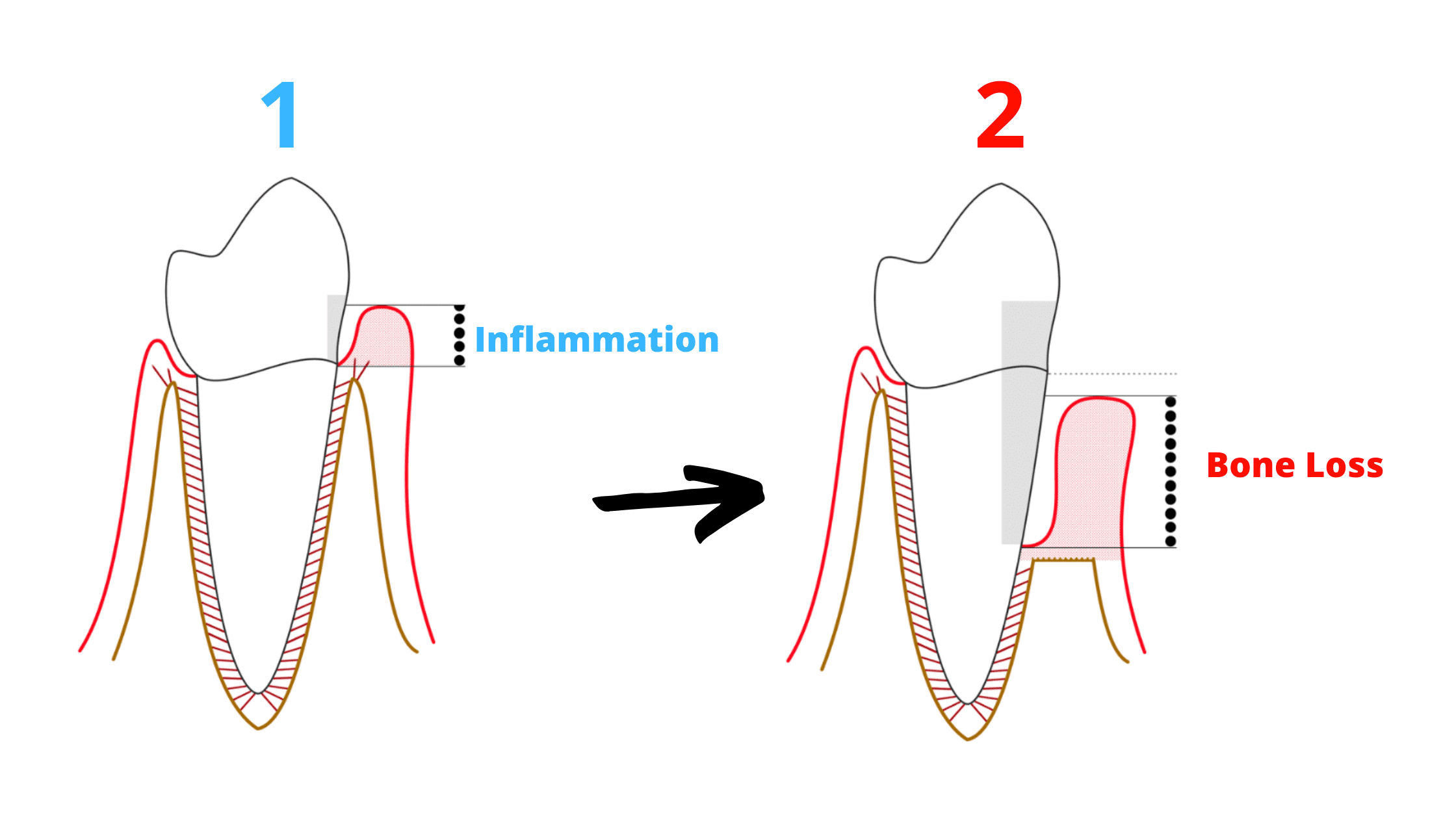
Unlike gingivitis, periodontitis is not reversible. The bone loss it causes is permanent and cannot fully grow back. If it’s allowed to progress further, periodontitis can cause your teeth to become loose or even fall out.
Treating periodontitis usually involves a deep dental cleaning procedure called scaling and root planing. The goal is to remove plaque and tartar from the teeth—and clean the roots too.
Antibacterial mouthwash and antibiotics are often necessary to fully eliminate bacteria hidden deep within the pockets.
3. Periodontal abscess:
Not all cases of periodontitis cause abscesses.Most of the time, periodontitis is chronic and progresses slowly without noticeable symptoms.
However, sometimes it can become aggressive and rapidly destroy the tissues that support your teeth. This happens when harmful bacteria overwhelm and completely take over your immune system.
When the infection is severe, pus can build up in the pockets, causing a localized swelling, often near the gum line.
Factors that can disrupt the balance between bacteria and your immune system, leading to a periodontal abscess, include:
- A weakened immune system
- Improper use of antibiotics
- Tartar build-up
- Trauma to the gums or teeth
- Medical conditions such as diabetes
Gum abscess treatment
The main goal is to eliminate the cause of the infection and drain the pus.To do this, your dentist needs to find the source, because as long as it’s there, the infection won’t heal.
Here are the different treatment approaches:
1. Root canal:
Your dentist will drill into the tooth to create a pathway for the pus to drain. Once the drainage happens, you’ll feel immediate relief. After about a week, your dentist will clean and fill the root canals and restore the tooth with a filling or crown.2. Surgical drainage:
If the abscess doesn’t drain with the root canal, your dentist may create a small incision in the gum to help the pus drain out directly.3. Deep dental cleaning:
If you have a periodontal abscess, your dentist will drain it through the pockets—the spaces between the gum and the root. The area will then be cleaned and smoothed to help the gum reattach during healing.4. Tooth extraction:
Sometimes the damage is too severe and the tooth cannot be saved. In this case, the tooth may need to be extracted to get rid of the infection for good.Antibiotic use for dental infections
- Antibiotics may not always be necessary to treat a gum abscess if drainage is sufficient.
- Antibiotics may be needed in specific situations, such as when the infection has started to spread.
- People with weakened immune systems may also need antibiotics.
- Antibiotics are not a standalone treatment for dental abscesses. While they may ease symptoms temporarily, they don’t fix the underlying cause.
The healing stages and recovery
Once the infection clears and the pus drains, the relieved pressure helps restore healthy blood flow to the area, promoting healing.How quickly your gums and bone heal depends on several factors, including the severity of the infection, your body’s healing ability, oral hygiene, smoking habits, and the treatment method used.
Your gums usually return to their normal appearance in about ten days. However, bone healing takes much longer—often several months to years.
Here’s what you can expect during the healing process:
1. Mild discomfort and swelling
Immediately after treatment, you may feel some mild discomfort. This is normal as your body needs to set up an inflammatory response in the affected area to bring in the cells and nutrients needed for healing.The pain should gradually subside over the next week. However, if the pain worsens or suddenly reappears, you should see your dentist immediately, as it may be a post-operative complication.
2. Gum healing
After about a week, the inflammation decreases, and the gums start to return to normal. The swelling and redness should fade, and most of the discomfort should improve.2. Bone healing
Bone healing is a slow process that can take several months. It can’t be assessed just by looking at your mouth—it requires dental X-rays.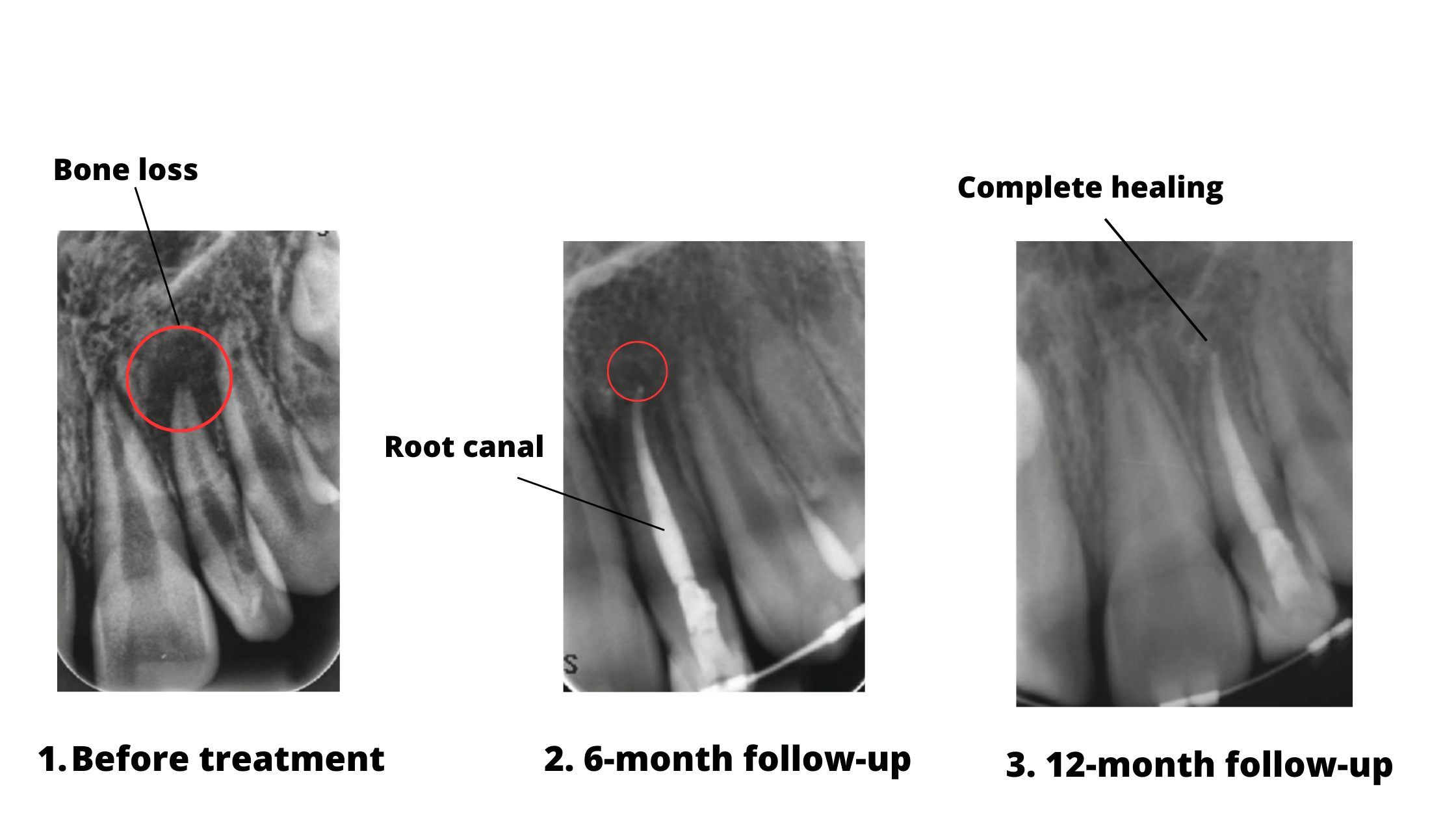
In the X-rays above, the dark areas around the root tips (marked with red circles) show bone loss caused by the abscess.
After treatment, these dark areas gradually shrink as the bone regenerates. 12 months later, the area appears denser and whiter, showing that the bone has fully healed successfully.
Your dentist will schedule follow-up appointments during this time to monitor your healing and make sure the infection is completely gone.
Other types of gum abscesses
Gingival abscess:
Gingival abscesses usually occur in the back teeth (molars). The pus accumulates in the gum part closer to the gum line, causing local swelling.
The most common cause is a piece of tartar or food stuck between the tooth and gum, causing irritation and inflammation.
Symptoms of a gingival abscess include pain, heat, bleeding, and discomfort when eating.
Pericoronary abscess:
Pericoronal abscesses occur mainly on emerging wisdom teeth. When the wisdom tooth is not properly positioned in the gum, it can cause food and bacteria to accumulate in the area, resulting in infection.
The potential complications of a gum abscess
If left untreated, an abscessed tooth can lead to serious complications.The first complication is tooth loss. As the pus eats away at the bone, the tooth becomes loose and may eventually fall out.
The infection can spread to facial soft tissues such as the cheek, lips, and skin. This is called cellulitis. When this happens, you may notice swelling, redness, and pain in the affected area.
If the infection involves a lower molar, it can easily spread to the spaces beneath the lower jaw. Because these areas are close to your airway, you might have trouble swallowing or breathing.
In more severe cases, the infection can spread extensively and completely block your airway. This life-threatening complication, called Ludwig’s angina, requires immediate hospital treatment.
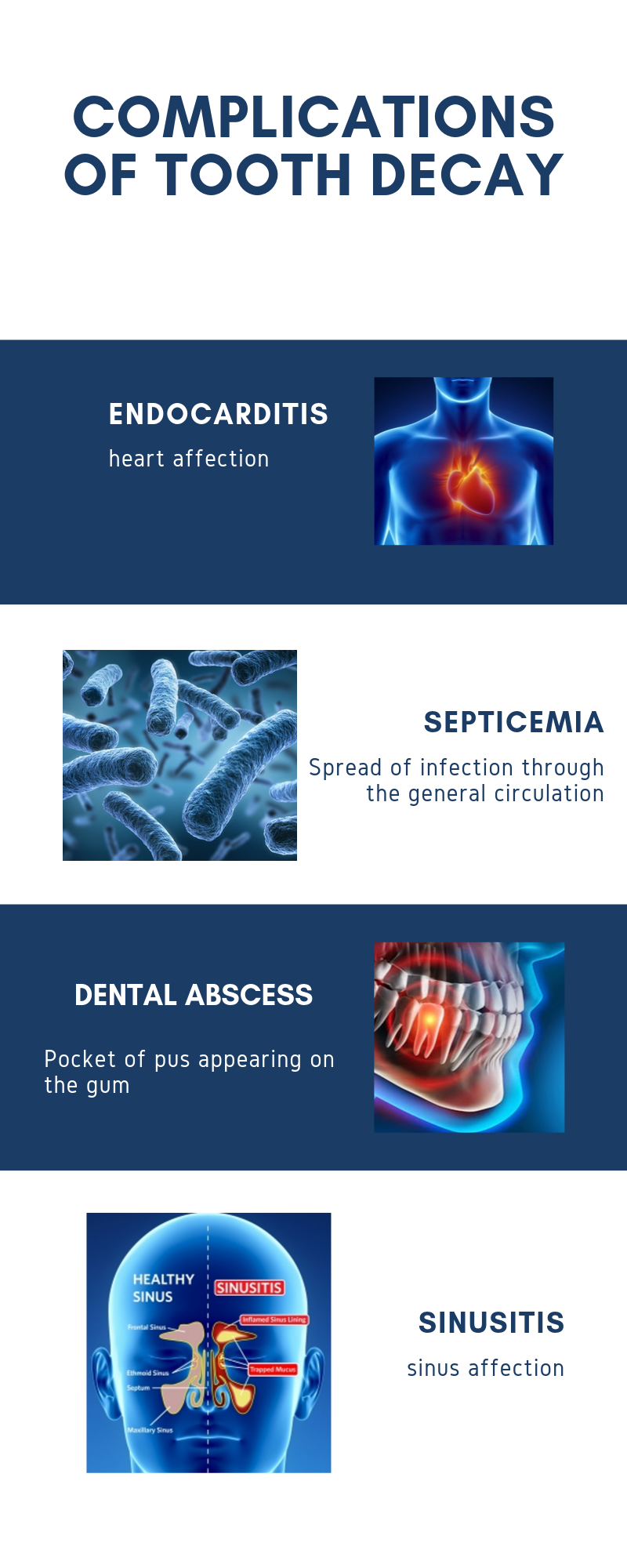
Other complications may include:
- Sinusitis: The sinuses are bony cavities located just above your upper molars. If the infection spreads beyond the roots, it can reach these areas and cause sinusitis.
- Endocarditis: This happens when the infection travels through the bloodstream to the heart. It can lead to heart failure if not treated promptly.
- Brain abscess: The infection can travel through the veins to the brain and cause a brain abscess.
Symptoms to look out for
Gum abscesses can never heal on their own. It’s not something you can postpone, because the earlier the treatment, the simpler and more effective it will be.Delaying treatment will not resolve the infection—it can only make it worse.
So, the best thing to do as soon as you notice a cavity or early infection is to see your dentist before it turns into something more serious.
In the meantime, there are some things to do and avoid at home to help ease your pain.
Symptoms to watch for that may indicate the infection is spreading include:
- Extreme swelling.
- Fever.
- Chills.
- Feeling unwell and tired.
- Increased heart and breathing rate.
- Dehydration and stomach pain.
Takeaway
While severe complications from dental infections are less common—especially in healthy people with strong immune systems—it’s not a reason to delay treatment!Treating a gum abscess in its early stages is straightforward, simpler, and less costly.
Waiting until the pain becomes unbearable or the swelling is extensive is never a good idea. At these advanced stages, treatment tends to be more complex and recovery takes longer.
People with weakened immune systems are at higher risk of serious, even life-threatening complications.
So never delay treatment for a tooth abscess. The sooner you act, the better the outcome.
- Periodontal Abscess https://www.ncbi.nlm.nih.gov/books/NBK560625/
- Periodontal Abscess https://www.ncbi.nlm.nih.gov/books/NBK560625/
- Textbook of General and Oral Surgery
- Ludwig Angina https://www.ncbi.nlm.nih.gov/books/NBK482354/