Yes, You Can Reverse Gingivitis at Home: Here's How
 Gingivitis is just a fancy way of saying “inflammation of the gums”. It's the earliest and mildest stage of gum disease.
Gingivitis is just a fancy way of saying “inflammation of the gums”. It's the earliest and mildest stage of gum disease.
It’s actually more common than you might think. Some studies suggest that chronic gingivitis affects over 90% of the global population to some extent. This might surprise you, as gingivitis is often so mild that it’s barely noticeable.
The tricky part is that if left untreated, gingivitis can advance to a more serious form of gum disease called periodontitis. At this stage, the inflammation starts affecting the underlying bone and ligaments.
The result? Loose teeth that might eventually fall out.
Not everyone with gingivitis will develop periodontitis. Some people are more immune than others. But is it a reason to leave gingivitis unchecked?
If you’ve noticed any signs of gingivitis, it’s time to take action now. Keep reading to find out the right steps to take to reverse this common issue.
In this article:
1. You Can Reverse Gingivitis (If You Catch It Early Enough)
2. The Right Actions to Reverse Gingivitis
3. Common Concerns When Reversing Gingivitis
4. How Do I Know If My Gums Have Healed?
5. The Main Culprit Behind Gingivitis
6. The Symptoms to Look Out For
7. From Gingivitis to Periodontitis: The Risk Factors
You Can Reverse Gingivitis (If You Catch It Early Enough)
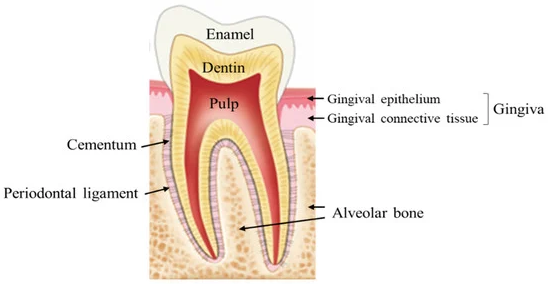
The tooth is supported and held in place by the gums, the bone, ligaments, and cementum.
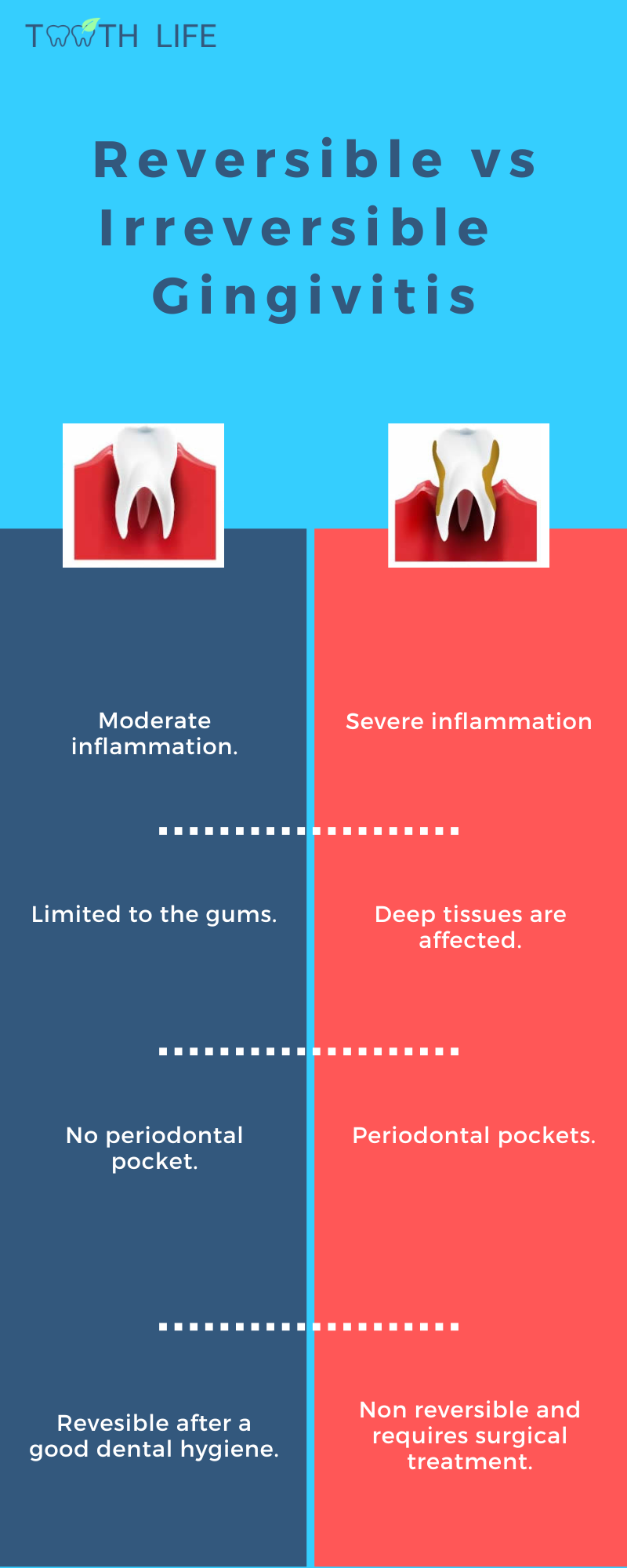
Gingivitis is a stage where only the outer gum tissue is affected, meaning the bone, ligaments, and cementum have not yet been damaged by inflammation.
The good news is that, unlike bone, the gum tissue can repair and heal itself. The damage caused by inflammation can be completely reversed with proper oral hygiene measures.
However, if gingivitis is left untreated, the inflammation can spread to the deeper tissues that support the teeth, causing irreversible damage. Unlike the gums, these deeper tissues cannot repair themselves, which is why periodontitis is considered irreversible.
So catching and treating gingivitis early is crucial to prevent it from progressing further. Early treatment is simpler, painless and less costly.
The Right Actions to Reverse Gingivitis
So, what should you do when you start noticing the early signs of gingivitis—like sensitivity, swelling, redness, or bleeding?While you can reverse gingivitis at home, it’s still best to visit your dentist. They can check for tartar buildup—which is sticky and hard to remove—and assess whether your bone has been affected.
At the gingivitis stage, all we need to do is remove the root cause of the problem. No surgery or invasive treatment is needed.
But keep in mind that treating gingivitis isn’t a one-time fix—it takes consistent, thorough oral care to keep your gums healthy and strong in the long run.
Here are a few tips to reverse gingivitis at home:
Brush Your Teeth Properly with the Right Technique
It's not enough to just brush your teeth—you need to do it properly. The best brushing technique to clean both your teeth and gums is the Modified BASS Technique. Here's how to use it:
- Hold the toothbrush parallel to your teeth.
- Tilt the brush to a 45-degree angle.
- Position the brush so the bristles are slightly under the gumline.
- With firm but gentle pressure, use a circular motion 15 to 20 times before moving to the next area.
- Brush all the front surfaces of your teeth, then clean the backs using the same motions.
- Hold the toothbrush vertically behind your front teeth and brush up and down.
- Brush the chewing surfaces of your back teeth.
Make sure to brush for a full 2 minutes, twice a day. Once you start brushing properly, you've already done most of the work to fight off most dental issues.
Change Your Toothbrush When It Shows Signs of Wear
Replace your toothbrush every three to four months, or sooner if the bristles become frayed or worn. A worn toothbrush is less effective at removing plaque and can host "BAD" bacteria that may harm your gums and teeth.
I also recommend using an electric toothbrush over a manual one. Electric toothbrushes are better at removing plaque. They are also easy to use. You simply need to slide the brush over your teeth and let it do the work for you.
Floss Once a Day
If you skip flossing or cleaning between your teeth, you're missing out on 40% of your teeth and gums surfaces. This means that after brushing alone, 40% of your dental surfaces can still retain plaque and food residues.
Clean between your teeth once a day, preferably at night before bed. You can use whichever tool you find most comfortable, whether it's dental floss, interdental brushes, or a water flosser. Studies have shown that water flossers are actually more effective at reducing gum inflammation.
Scrape Your Tongue Once a Day
Your tongue can also collect harmful bacteria that contribute to bad breath. Clean it once a day using your regular toothbrush or, ideally, a tongue scraper.
By cleaning your tongue, you not only reduce the bacterial load in your mouth, but also improve your breath.
Balance Your Diet
What you eat affects not only your overall health but also the health of your gums. Healthy gums need essential nutrients, including vitamins C, D, E, and B-complex vitamins. Studies have shown that a deficiency in these nutrients can lead to increased inflammation, more bleeding, and a higher risk of severe gum disease.
Replace pro-inflammatory foods with anti-inflammatory ones.
It’s no surprise that foods known to trigger inflammation—like sodas, refined carbs, and processed snacks—are also harmful to your overall health.
Instead, focus on anti-inflammatory foods, especially those rich in omega-3 fatty acids and vitamins D and E.
Stop or Cut Back on Risk Factors
Certain factors and habits can increase your risk of gum disease. These include:
- Smoking: Smoking is a major risk factor for gum disease. Tobacco and its by-products weaken the body’s defense mechanisms, reduce blood flow to the gums, and impair their ability to heal.
- Bruxism: Grinding or clenching your teeth (a condition known as bruxism) can make gum problems worse.
It puts excessive pressure on the tissues around your teeth and can accelerate their breakdown over time. - Mouth Breathing: Breathing through your mouth can dry out your gums and reduce the natural cleaning effect of saliva.
- Aggressive Tooth Brushing: Brushing too hard can damage your gums and contribute to gum recession.
Stay Hydrated
Staying hydrated throughout the day helps prevent your mouth from drying out. This also prevents the bacteria from gathering and forming plaque, which is the primary cause of gingivitis.
Try Oil Pulling
Oil pulling is an ancient practice that is proven today to reduce harmful bacteria in the mouth and improve gum health.
It’s definitely worth giving a try—and once you feel the difference, you won’t want to go without it. Here’s how to do it:
- Choose Your Oil: Use 1 tablespoon of coconut oil, sesame oil, or sunflower oil.
- Swish the Oil: Swish the oil around your mouth for 15 to 20 minutes. Make sure to push and pull the oil through your teeth and around your gums.
- Spit It Out: After swishing, spit the oil out.
- Brush Your Teeth: Rinse your mouth and brush your teeth as usual to remove any remaining oil and bacteria.
Common Concerns When Reversing Gingivitis
One of the most common concerns I hear from patients is: “I can’t brush or floss because my gums bleed so much!”Even if your gums are bleeding, it’s important to keep brushing and flossing.
Think of the bleeding as a sign that your gums are in their way toward healing.
That said, if your symptoms aren’t getting better—or are getting worse—despite your best efforts, don’t wait to see your dentist.
You could be dealing with a more serious form of gum disease (periodontitis), which can’t be treated with brushing alone.
In these cases, your dentist may recommend a deep cleaning (scaling and root planing) to remove plaque and tartar from below the gum line.
How Do I Know If My Gums Have Healed?
With consistent care, you can expect your gums to return to their healthy state within a few days to weeks. But how can you tell if your gums have healed?Most patients notice some improvement as soon as they improve their oral hygiene. You’ll notice your gums gradually changing to a light pink color. The gum line will become more defined and firmly attached to your teeth.
Any swelling will subside, and your gums should no longer bleed when you brush or floss.
The Main Culprit Behind Gingivitis
Plaque is the primary cause of gingivitis. This whitish, thin, bacteria-laden film constantly forms on your teeth and gums. When you neglect your oral hygiene and don't brush regularly, plaque builds up and thickens, especially along the gum line.Pathogenic bacteria can then infiltrate the space between your teeth and gums, leading to inflammation—this is gingivitis. Over time, plaque can absorb minerals from your food and saliva, becoming calcified, stickier, and even more difficult to remove. At this stage, it's known as tartar.
In addition to plaque, other factors can indirectly worsen gingivitis. These include anything that promotes more plaque buildup, such as dental crowding, cavities, or poorly fitting dental crowns and fillings.
People who breathe through their mouths are more prone to severe forms of gingivitis. Mouth breathing dries out the mouth, preventing saliva from doing its natural cleaning function.
There are also less common forms of gingivitis that aren’t caused by plaque but by other factors, such as viral infections (like herpes), fungal infections (like oral thrush), autoimmune diseases (like pemphigus), or allergies to certain ingredients in oral care products or foods.
How Does Gingivitis Progress?
Without treatment, gingivitis can progress into a more severe form of gum disease known as periodontitis. Before reaching this stage, gingivitis typically advances through the following phases:- Healthy Gums: This is the starting point. Healthy gums are pink, firm to the touch, not swollen, and don't bleed when you brush, floss, or eat. They also have a stippling texture, resembling an orange peel.
- Early Gingivitis: After 8 to 14 days of plaque buildup, certain bacteria trigger inflammation, which shows up as redness, swelling, and bleeding in your gums.
- Advanced Gingivitis: When plaque keeps building up or other risk factors come into play—like irritations, hormonal changes, or systemic diseases—the inflammation gets worse. At this stage, your gums may even start bleeding on their own, without any contact.
The Symptoms to Look Out For
When checking the health of your gums, there are several signs to watch out for. These include:- Your Gums Color: Healthy gums are usually pink, though this can vary depending on ethnic and genetic factors. Unhealthy gums appear red or darker due to inflammation, which is a clear sign of gingivitis.
- Your Gums Texture and Consistency: Healthy gums are firm to the touch and have a stippling texture, similar to an orange peel. In contrast, unhealthy gums may feel soft, shiny, swollen, or spongy, lacking that firmness.
- Gum Bleeding: Healthy gums do not bleed when you brush, floss, or eat. When they bleed during these activities, it's a sign of inflammation.
- Check Your Gum Line: A healthy gum line fits snugly around your teeth and has a regular shape. In gingivitis, the gum line may become uneven due to swelling. If your gum line has receded or your teeth appear longer than before, it could indicate periodontitis.
- Bad Breath: Bad breath or halitosis is not always associated with gingivitis. However, it almost always indicates that your oral hygiene needs improvement, and that you probably have a build-up of plaque and tartar that you must get rid of.
- Loose or Shifting Teeth: These are major red flags for advanced periodontitis. If you notice your teeth are no longer stable or have started to shift, see your dentist immediately. This usually means the bone supporting your teeth is being destroyed.
From Gingivitis to Periodontitis: The Risk Factors

If plaque is not removed through proper oral hygiene, it can build up and harden into tartar. Tartar, a calcified mass of bacteria, cannot be removed at home and can cause gingivitis to progress to periodontitis.
Here are some risk factors for periodontitis:
- Smoking: Besides weakening the immune system and affecting blood flow, tobacco and its by-products can actually mask early signs of gum inflammation. As a result, you might not notice the problem until it reaches an advanced stage.
- Stress: Stress releases hormones that affect the immune response. Plus, it can lead to bruxism or involuntary teeth grinding, which can exacerbate gum disease.
- Medications: Certain medications, such as antidepressants, antihypertensives, and immunosuppressants, can negatively impact gum tissue by affecting saliva production and immune response.
- Diabetes: People with diabetes are more susceptible to gum disease, and gum disease can make it harder to control blood sugar levels, worsening diabetes symptoms.
- Genetics: Genetics plays a significant role in periodontitis. Some people may never develop the condition, even with poor oral hygiene, while others may be more prone to it despite good practices.
Periodontitis represents an imbalance between the immune response and pathogenic bacteria. When bacteria dominate or the immune response is insufficient, the disease can progress severely and rapidly.