The 4 Stages of Gum Recession You Need to Know
 Gum recession is a real issue—and it’s more common than you might think, especially as we age. In fact, over 50% of people have at least one tooth affected by it!
Gum recession is a real issue—and it’s more common than you might think, especially as we age. In fact, over 50% of people have at least one tooth affected by it!
The thing is, gum recession doesn’t happen overnight. It’s usually a slow and gradual process that can go unnoticed for years.
In this post, we’ll break down the key stages of gum recession and how to recognize each one—so you can better understand what’s happening and where you stand.
In this article:
1. Stage 1: Gingivitis (Gum Inflammation)
2. Stage 2: The Onset of Gum Recession
3. Stage 3: Moderate Gum Recession
4. Stage 4: Severe Gum Recession and Extensive Bone Loss
5. Do All Forms of Gum Recession Follow the Same Pattern?
6. Overcoming Receding Gums
Stage 1: Gingivitis (Gum Inflammation)
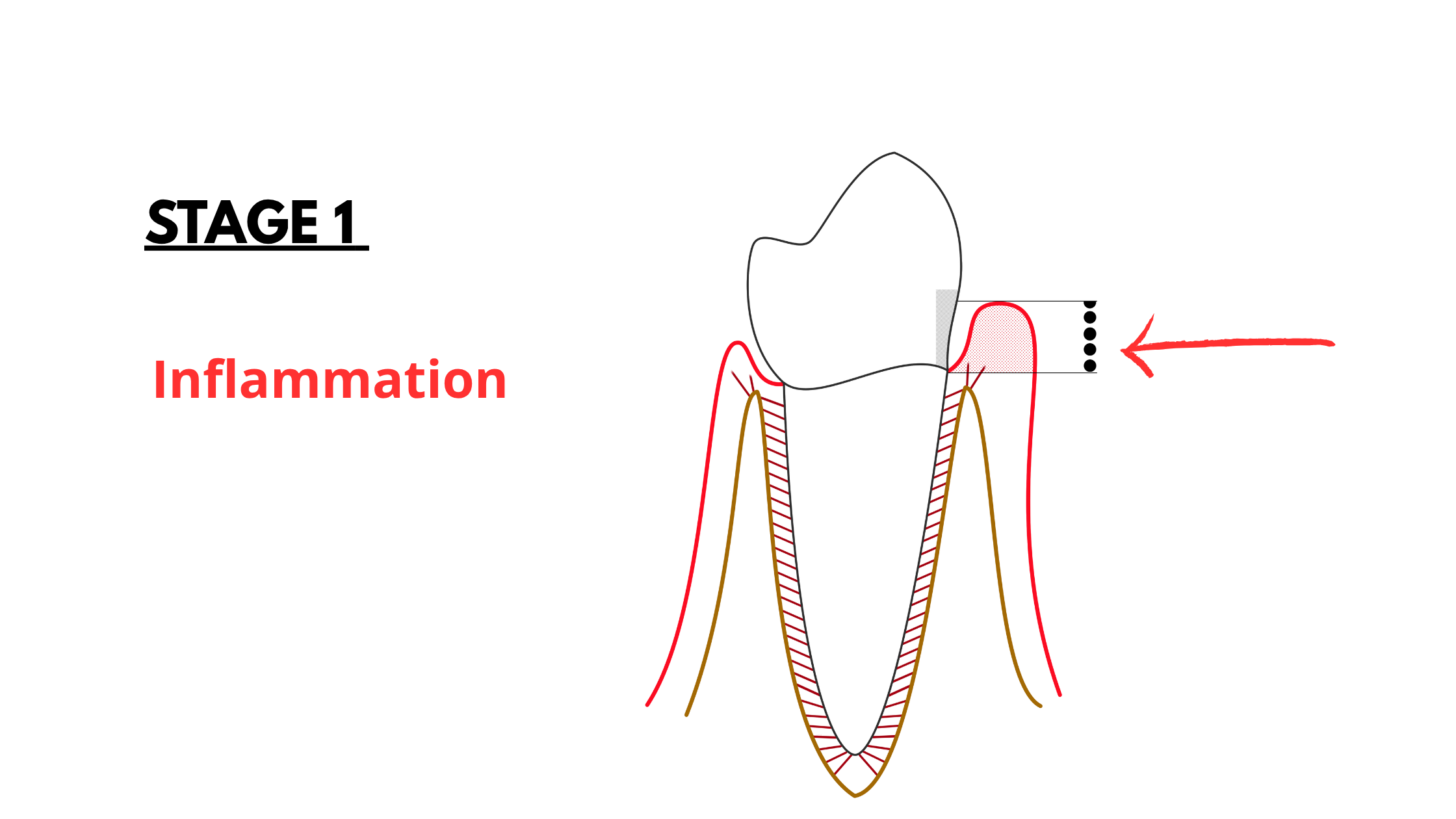
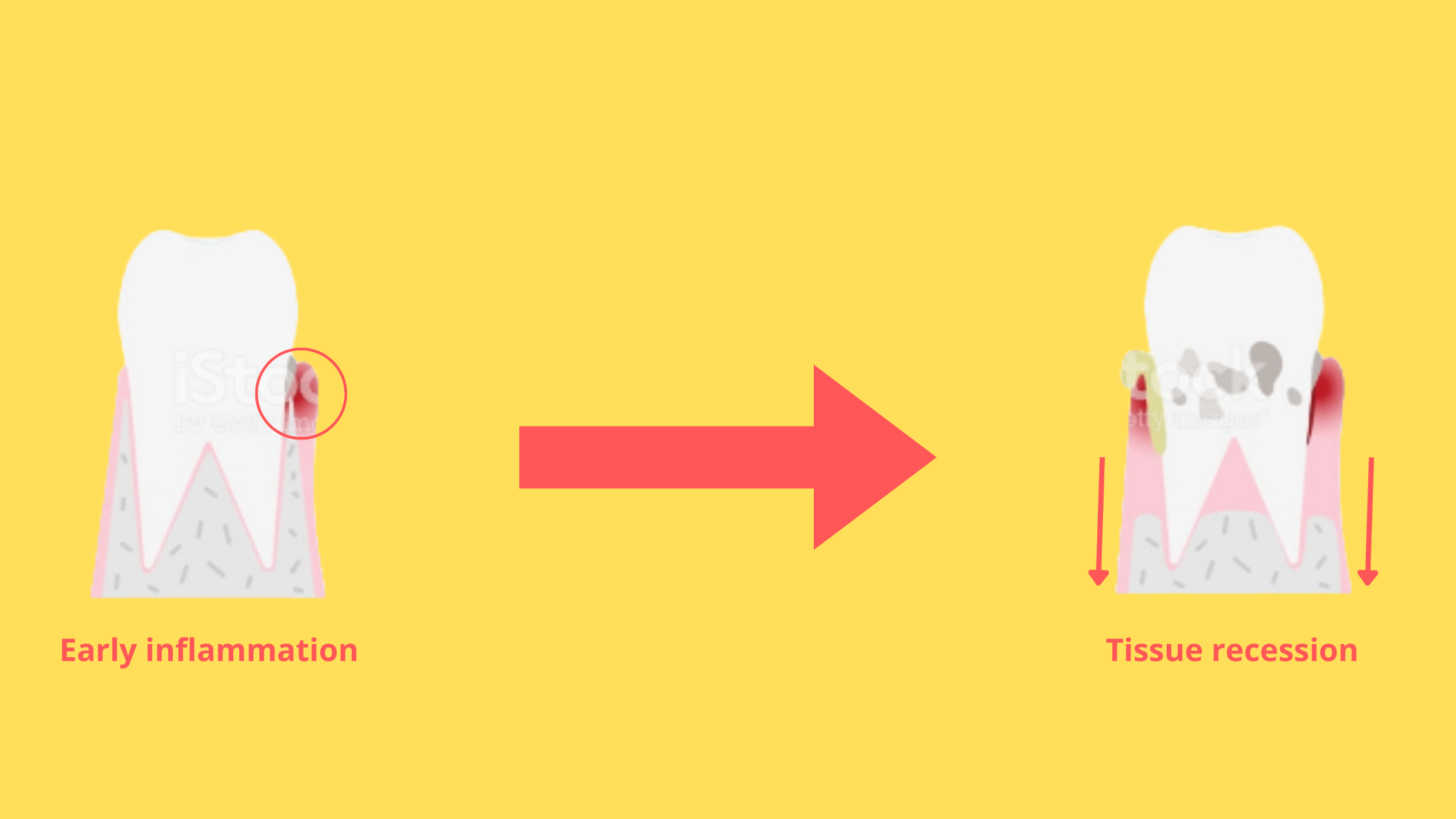
Gingivitis is just a fancy term for gum inflammation. It’s actually the starting point of most gum problems, including gum recession.
Inflammation is the body’s natural defense mechanism—it helps fight off harmful bacteria. But when it becomes too intense or lasts too long, it can do more harm than good. Over time, chronic inflammation can damage your gum tissue and even start to erode the bone underneath.
Gingivitis usually begins when plaque builds up on your teeth and along the gum line. If you don’t brush and floss well, bacteria in the plaque multiply and irritate your gums. This leads to redness, swelling, sensitivity, and bleeding—especially when brushing or eating.
The tricky part? Gingivitis can be so mild in the beginning that you might not notice anything wrong. That’s why many people don’t realize they have gum disease until the damage becomes more obvious, and more serious.
The good news is that gingivitis is completely reversible at this stage. With proper care, you can stop it before it turns into something more serious.
Stage 2: The Onset of Gum Recession
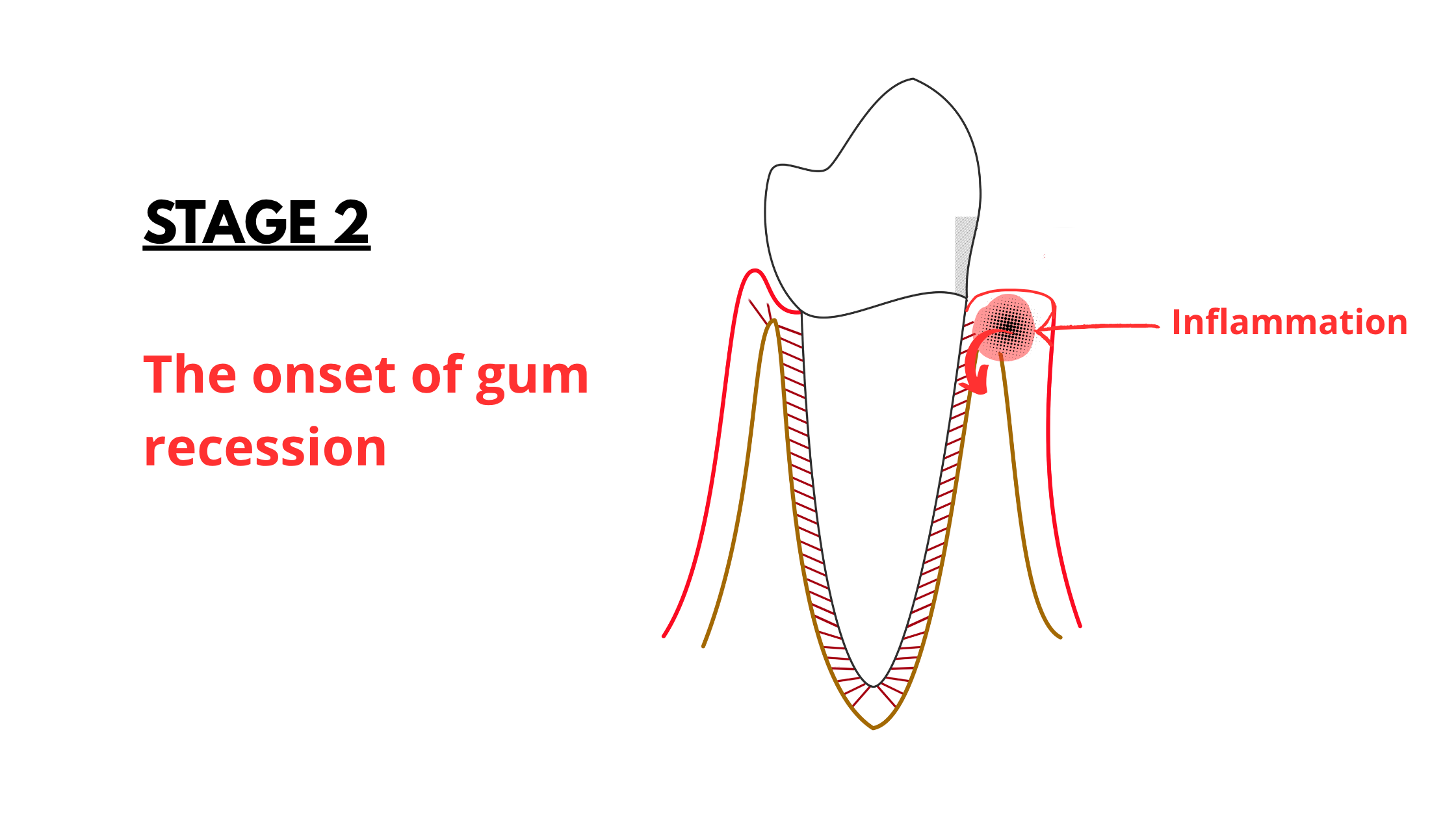
When inflammation persists longer than it should, it becomes chronic. And chronic inflammation doesn’t just affect the gums—it’s also behind many age-related diseases like arthritis, heart disease, diabetes, and even some neurological conditions.
Once gingivitis progresses, the damage becomes irreversible. That means the gum tissue and bone loss can’t fully grow back.
At first, your immune system tries to contain the harmful bacteria in the outer layers of the gums and bone. But slowly, the bone supporting your teeth starts to break down, and the gums begin to shrink and pull back.
The problem? This early damage is still too shallow to be easily noticed.
To make things trickier, this stage usually doesn’t cause any pain. Most people don’t realize something’s wrong until their teeth start feeling sensitive or they notice changes in how their smile looks.
Sometimes, gum recession starts as a small groove or notch along the gum line. This minor form is often not caused by bacteria, but rather by constant irritation—like brushing too hard or friction from a lip or tongue piercing.
If you spot something like this, it’s a warning sign to stop the source of the irritation immediately to prevent further damage.
Stage 3: Moderate Gum Recession
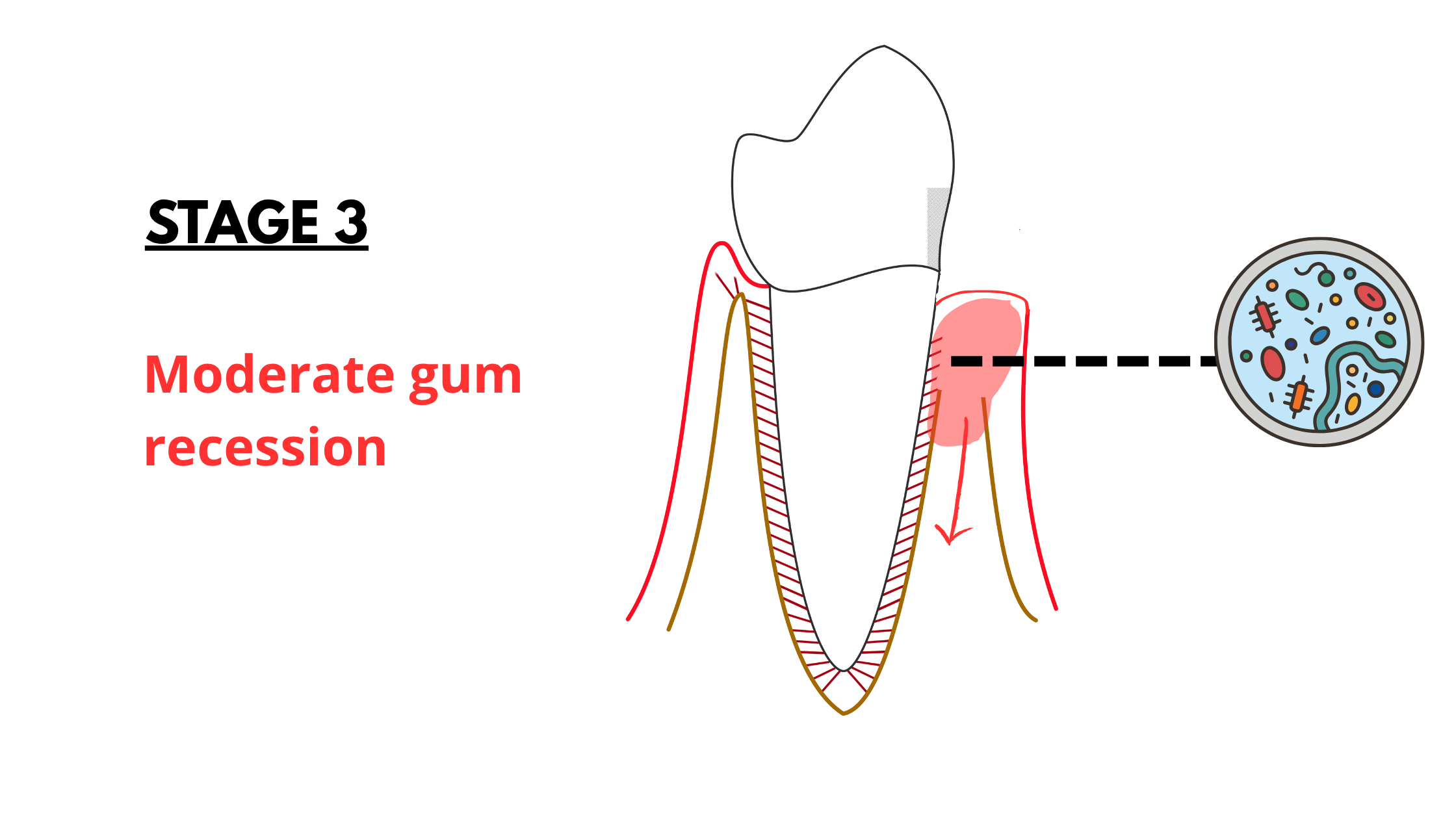
At this more advanced stage, bacteria have penetrated deeper into the gums and bone around the tooth.
This can lead to significant damage—sometimes resulting in the loss of nearly half of the bone supporting the tooth.
As the bone recedes, so do the gums, exposing the tooth roots and making your teeth look longer than before. The more bone that’s lost, the more severe the gum recession becomes.
Typically, gum recession at this stage affects all sides of the tooth: the front, back, and in between the teeth.
As the gums shrink between teeth, gaps called “black triangles” begin to form. These dark spaces are quite noticeable and can be a major reason why people seek treatment.

Stage 4: Severe Gum Recession and Extensive Bone Loss
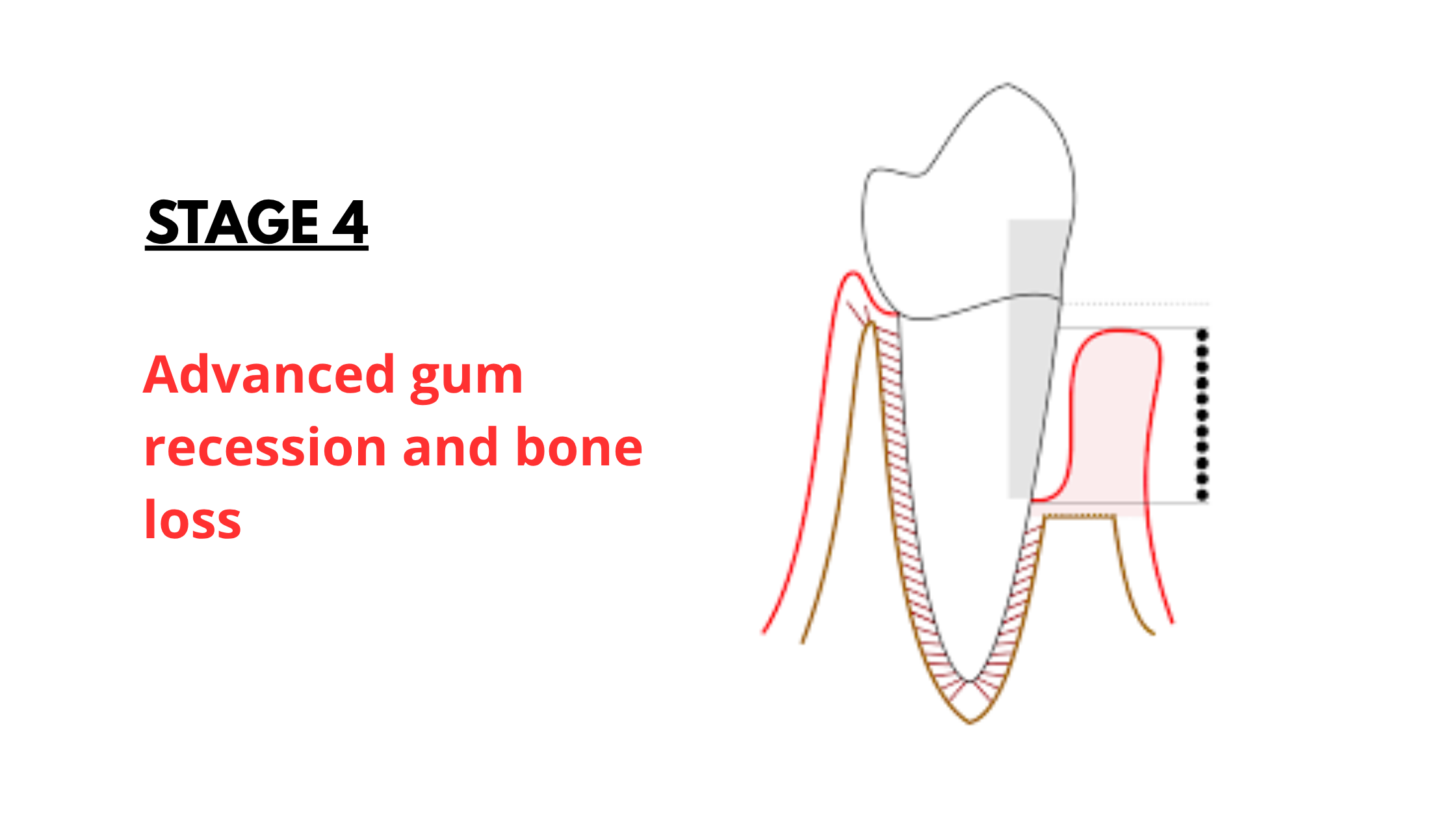
This is often called the terminal stage—right before tooth loss.
At this point, more than half of the supporting bone is gone. Gum recession is much more noticeable, with large areas of the tooth roots exposed, making your teeth look even longer than before.
Teeth may start to feel loose and can even shift out of place. This can make everyday activities like eating and speaking uncomfortable.
Is it too late to save your teeth at this stage? It depends on several factors, but one thing is clear: the more severe the damage, the harder it is to treat—and the less predictable the results.
That’s why early treatment is so crucial to save your natural teeth and keep them healthy for as long as possible.
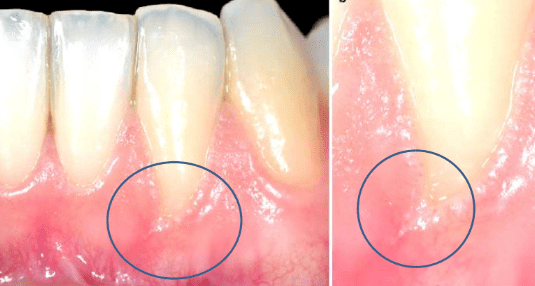
Do All Forms of Gum Recession Follow the Same Pattern?
Not all gum recession follows the same path. How far it progresses mostly depends on the root cause.The stages we described earlier apply to gum recession caused by bacterial inflammation—the most common type. This form usually develops slowly over many years. It tends to affect multiple teeth and involves all surfaces. So, the damage tends to be more widespread.
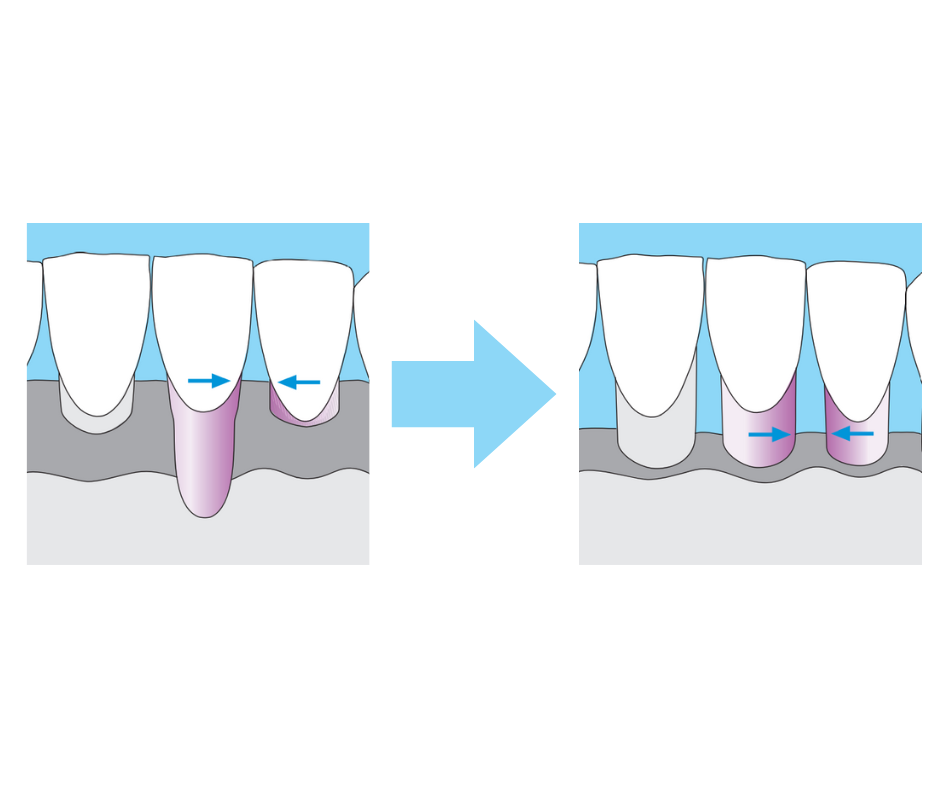 There’s also another common type of gum recession caused by trauma or repeated mechanical irritation. The most frequent culprits are aggressive brushing or using a hard-bristled toothbrush.
There’s also another common type of gum recession caused by trauma or repeated mechanical irritation. The most frequent culprits are aggressive brushing or using a hard-bristled toothbrush.
While trauma-related recession involves the same process, there are some differences. Here, only the front (visible) surface of the tooth is affected—the gums between the teeth typically remain healthy.
Another difference is that trauma-related recession usually affects just one or a few teeth, unlike the widespread pattern seen in bacterial gum disease.
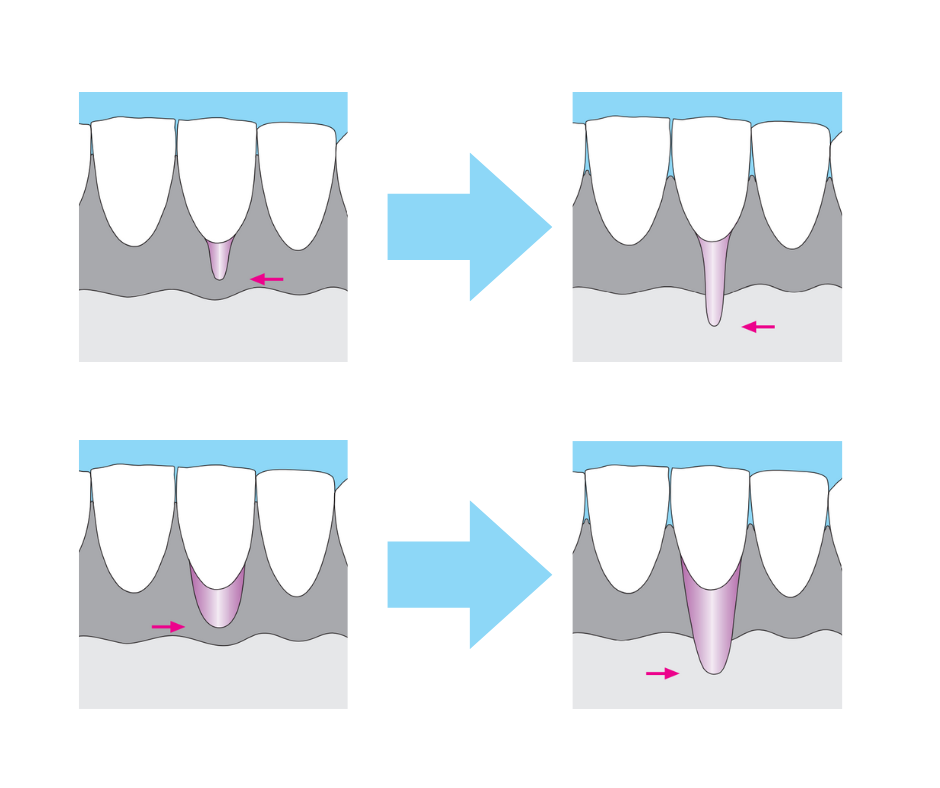 Since inflammation isn’t involved in this type, your gums may still look pink and healthy even as they recede.
Since inflammation isn’t involved in this type, your gums may still look pink and healthy even as they recede.
Overcoming Receding Gums
No matter the cause or form of gum recession, the most important step is to identify and stop the source of the problem. Simply removing the underlying cause will help stop the problem from getting worse.The best course of action is to see your dentist as soon as possible to check for gum disease or any trauma that may be damaging your gums.
If gum disease is the cause, a deep dental cleaning may be necessary to remove bacteria hidden below the gum line—areas that regular brushing and flossing cannot reach.
If trauma is the culprit, simply removing the source of injury is usually enough to prevent further damage.
Once that’s done, you and your dentist can discuss treatment options—whether surgical or non-surgical—to cover exposed roots and restore the natural look of your gums.