Tooth Decay Stages: From Cavity to Serious Complications
 Tooth decay is more complex than you might think. It's not just about eating too much sugar or skipping brushing — it’s actually the result of many factors working together.
Tooth decay is more complex than you might think. It's not just about eating too much sugar or skipping brushing — it’s actually the result of many factors working together.
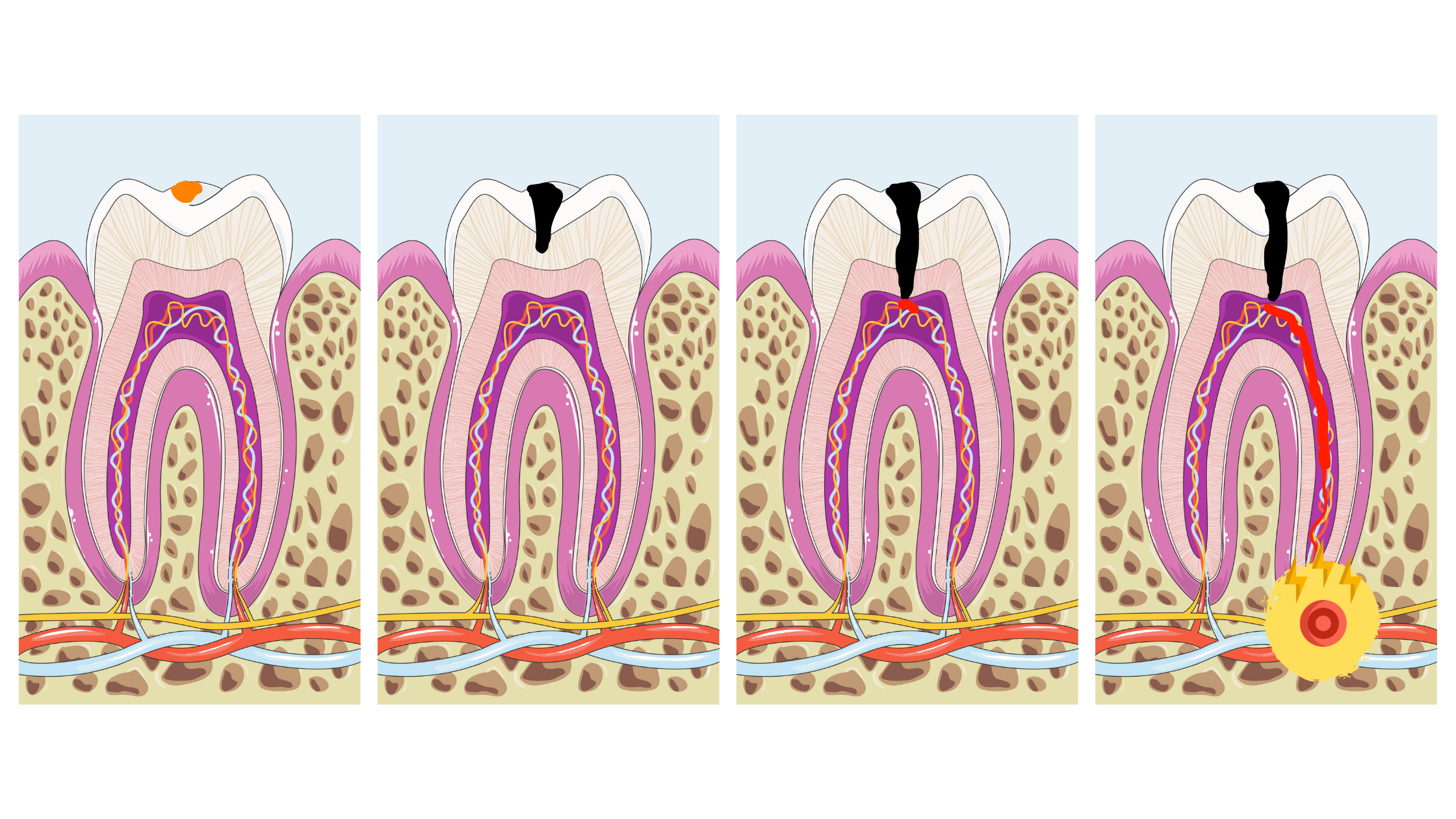
Before a visible cavity forms, tooth decay usually goes through several stages, often without you even noticing.
In this post, you’ll get a clear visual breakdown of each stage of tooth decay, along with the treatment options available at every step.
1. How Does Tooth Decay Start and Progress Over Time?
2. Tooth Decay Stages
3. What Does the Early Stage of Tooth Decay Look Like?
4. What Does the Cavity Stage Look Like?
5. Factors That Make Cavities Worse
6. Takeaway
How Does Tooth Decay Start and Progress Over Time?
Tooth decay begins when acid attacks from bacteria become too frequent or intense for your teeth to repair on their own.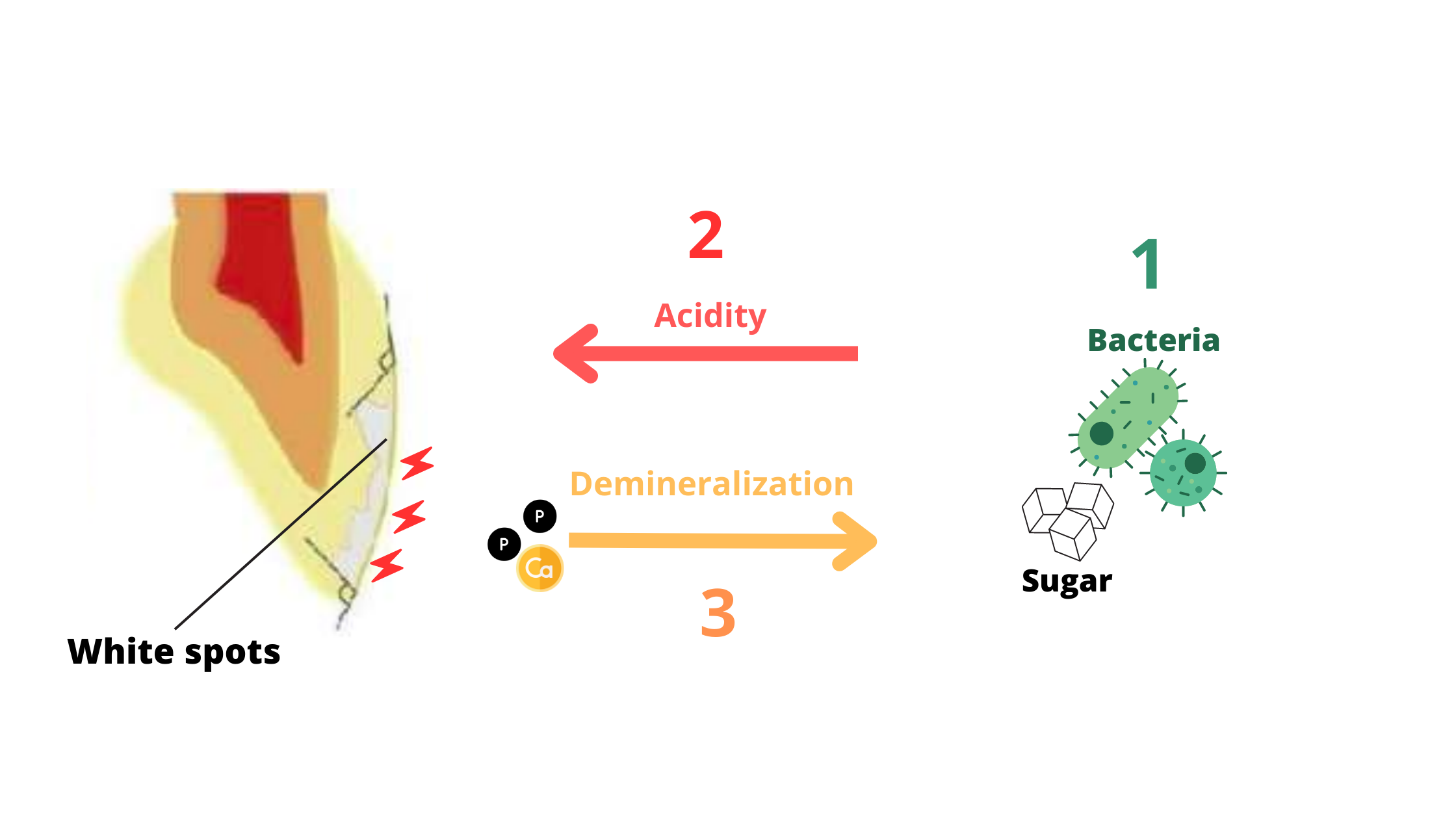
After eating something sugary, bacteria in your mouth break down those sugars and produce acids that strip minerals from your enamel. Normally, saliva — along with fluoride from toothpaste — helps rebuild those lost minerals. But when mineral loss happens more often than the tooth can recover, decay sets in.
Decay starts in the enamel, the hard outer layer of the tooth. Enamel is made of tiny, tightly packed crystals called enamel rods, which give it strength and durability.
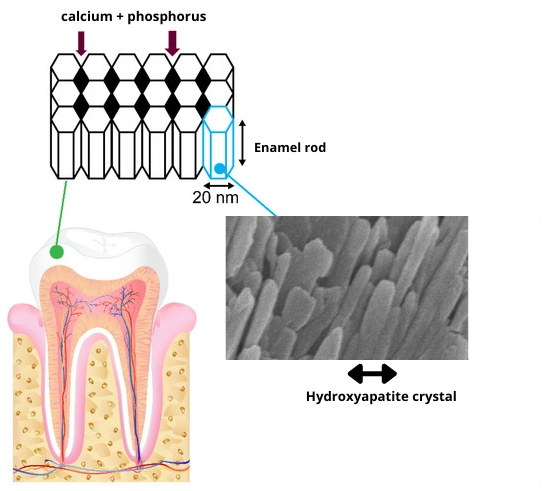
But even though enamel is the hardest tissue in the human body, it has a weakness.
When the mouth becomes too acidic, the chemical bonds holding those crystals together start to break down. This leads to early signs of decay known as surface demineralization, which appear as white or brown spots on the tooth.
At this early stage, tooth decay can still be stopped or even reversed through a healthy diet, proper oral hygiene, and remineralizing products (like fluoride or hydroxyapatite).
However, if demineralization is left untreated, it can progress further into the enamel, eventually forming a hole — this is what we call a cavity.
From there, the decay moves into the dentin, the layer beneath the enamel. Dentin is still a hard tissue, but it’s softer and less dense than enamel, so decay spreads more quickly once it gets in.
At this point, the damage is no longer reversible. Your dentist will need to remove the decayed part of the tooth and place a filling.
In more advanced stages, decay can reach the pulp, the innermost part of the tooth.
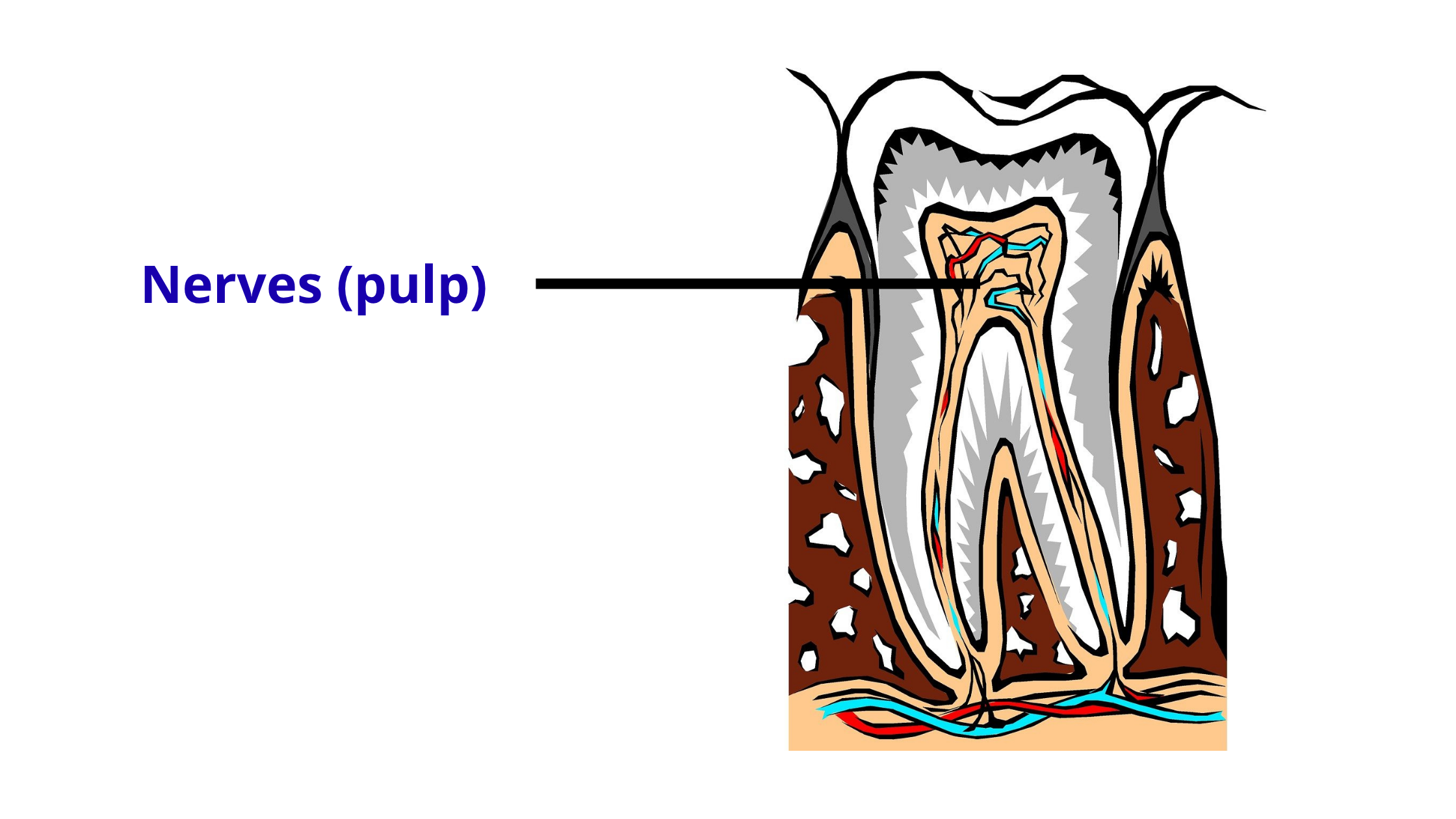
The pulp is the soft inner part of the tooth that contains nerves and blood vessels.
When decay reaches the pulp, it can lead to severe pain and irreversible inflammation. At this stage, a root canal treatment is usually necessary to save the tooth.
Tooth Decay Stages
Here’s a breakdown of the different stages that tooth decay goes through:1. Enamel Stage
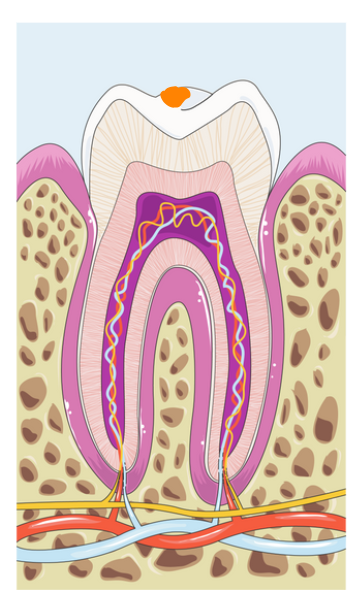
Tooth decay starts by affecting the enamel—the outermost layer of the tooth.
At this early stage, the damage is still shallow, so you won’t feel any pain or discomfort to let you know something’s wrong.
The only visible sign might be a whitish or brownish chalky spot, which means your teeth are beginning to lose minerals.
The good news? Decay at this stage can be stopped or even reversed.
With proper care and remineralization treatments, enamel has the ability to heal.
But if left untreated, this demineralization can worsen and turn into a cavity—something that's hard to fix on your own.
Treating the enamel stage:
When decay is still limited to the enamel surface, remineralization treatments can be highly effective. The goal is to strengthen and repair enamel by restoring lost minerals.
This consists of:
- Improving your oral hygiene routine
- Reducing sugar intake
- Using fluoride or calcium-phosphate-based products to rebuild the damaged areas
There are many great remineralizing products available in various forms like gels, m²outhwashes or creams. Some popular options include CariFree (gel with hydroxyapatite), MI Paste (dental cream), and ROCS Dental Gel.
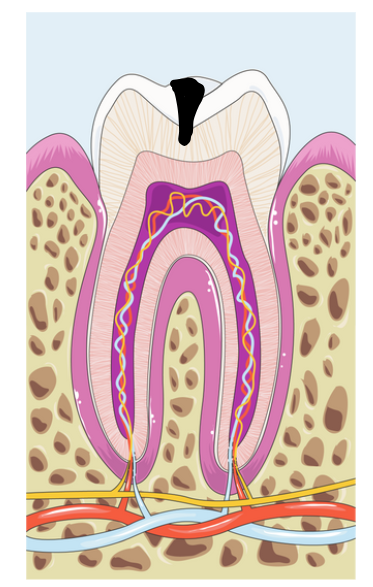
2. Dentin stage
When decay goes beyond the enamel, it reaches the dentin—the layer just above the pulp (where the nerves are).
At this stage, you might start to feel sensitivity, especially to cold or pressure.
Dentin decay is deeper and more serious than enamel decay.
It can't be reversed and won’t heal on its own, even with remineralization treatments.
Since dentin is softer than enamel, decay spreads about twice as fast once it gets in.
The only way to treat it is to remove the decayed tissue and restore the tooth with a filling to protect the pulp underneath.
Treating the dentin stage:
When tooth decay reaches the dentin, more invasive treatment is usually needed.
This typically involves drilling into the tooth to remove the decayed tissue, then restoring it with a filling.
If the cavity is large or the tooth has become structurally weak, a more advanced restoration may be recommended—often requiring two visits. These options may include an inlay, onlay, or dental crown.
That’s why it’s so important not to delay treatment. The sooner you treat a cavity, the simpler—and less costly—it will be.
3. Pulp stage
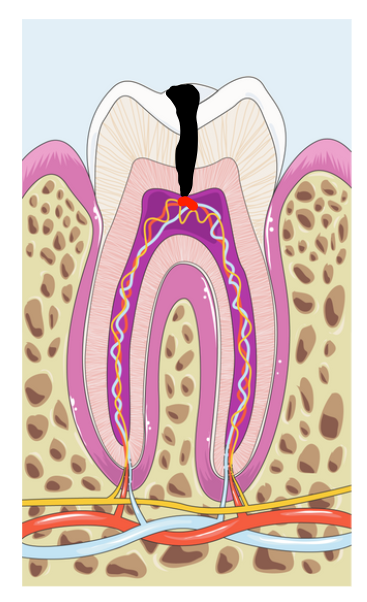
The pulp is the living tissue at the center of the tooth that feeds it throughout its life.
When decay reaches the pulp, it causes inflammation—a condition known as pulpitis. This often results in intense pain, especially when consuming hot, cold, or sour foods and drinks.
As the inflammation worsens, the pain can become constant and throbbing—sometimes severe enough to keep you awake at night.
If left untreated, the blood vessels inside the pulp shrink and break down, eventually leading to pulp death (necrosis).
At this point, the pain may go away—but that doesn’t mean the tooth has healed.
Treating the pulp stage:
Once decay reaches the pulp, root canal treatment becomes necessary.
During the procedure, the infected pulp is completely removed from the tooth. The root canals are then cleaned, disinfected, and filled with a special material to prevent further infection.
After the root canal, depending on what remains of the tooth, the treatment options may be as follows:
- Regular filling.
- Dental crown.
- Endocrown.
- Post and core crown.
4. Complications
In the final stages of tooth decay, various complications can arise.
When the pulp dies, the infection can spread beyond the tooth, leading to dental abscess or gum boil.
If left untreated, the infection can spread to the jawbone and surrounding areas, leading to severe swelling in the face.
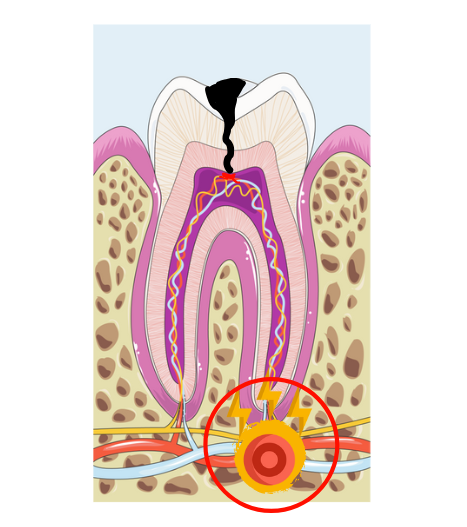
Treating a dental infection:
A tooth abscess or dental infection should never be ignored or delayed. As long as the source of the infection remains inside the tooth (in the pulp), the infection will persist or even worsen over time.
At this stage, the pulp has died, meaning there’s nothing left inside the tooth to contain or fight off the infection. As a result, the bacteria can spread beyond the tooth and into surrounding tissues.
In some cases, a dental infection can become life-threatening, especially in people with weak immune system or chronic conditions like diabetes. Serious complications can include:
- Cellulitis: When the infection spreads to the soft tissues of the face and neck, causing painful swelling, redness, and warmth. If left untreated, it can reach deeper tissues, block the airways, and become life-threatening.
- Sinusitis: The roots of the upper molars are close to the maxillary sinuses. A dental infection can extend into these sinuses, causing inflammation and sinus pain.
- Endocarditis: Bacteria from a dental abscess can enter the bloodstream and travel to the heart, potentially causing bacterial endocarditis, a serious infection of the heart lining.
- Septicemia: The bacteria can also spread through the bloodstream to other organs, including the lungs, kidneys, and liver. Individuals with pre-existing conditions affecting these organs are at higher risk of complications.
Treatment depends on the extent and severity of the infection. Typically, the first step is to drain the pus to relieve pressure and pain.
Then, the source of infection must be eliminated — either through a root canal treatment (to clean and seal the tooth) or by extracting the tooth if it cannot be saved.
Antibiotics may be needed if the infection has spread or in people with medical conditions that weaken the immune system.
What Does the Early Stage of Tooth Decay Look Like?

Early tooth decay often appears as white, rough, chalky spots—known as demineralization lesions or "white spots."
These spots can trap food pigments over time, causing them to turn yellow or brown.
On the chewing surfaces—especially in the pits and grooves—early decay can be harder to notice. Instead of white spots, it often appears as thin black lines or dark staining in those grooved areas.
What Does the Cavity Stage Look Like?

A cavity is deeper and more advanced. It often appears as a grayish or black hole that easily traps food and plaque.
If you looked at it under a microscope, you’d see that bacteria are going much deeper into the tooth than what’s visible.
That’s why cavities can’t be treated at home. Only a dentist can clean out the decay and restore your tooth properly.
Factors That Make Cavities Worse
Tooth decay is a complex process caused by many factors working together.Simply put, cavities happen when the harmful factors outweigh the protective ones.
Here are some factors that can harm your teeth and increase your risk of cavities:
- Poor oral hygiene – Not brushing and flossing regularly allows bacteria to build up and form plaque. Plaque is a sticky film that’s the main culprit behind tooth decay.
- Dry mouth – Often overlooked, dry mouth is one of the major causes of cavities. Saliva helps clean your teeth, prevent plaque buildup, and repair early damage between meals. When saliva flow decreases, your risk of decay goes up.
- Too much sugar – Sugar is the fuel for cavity-causing bacteria. A sugar-rich diet helps these bacteria overgrow and produce too much acid that damages your teeth.
- Crowded teeth – Overlapping or crowded teeth are harder to clean and more likely to trap food and plaque.
- Enamel defects – Whether caused by genetics or environmental factors, weak or defective enamel makes your teeth weaker and more vulnerable to decay.
Takeaway
Don’t wait for tooth decay to become a serious health threat. The further it progresses, the more damage it causes — and the more complex and costly the treatment becomes.While early enamel damage can be reversed, decay that reaches the dentin or beyond is irreversible and must be treated by a dentist.
Delaying treatment won’t make the problem go away — it will only make it worse.