What causes gum recession in one tooth and how to treat it?
 Gum recession is a common condition that progresses over time if left untreated. When the gums pull back, they expose the tooth roots, which can cause sensitivity and make your teeth appear longer.
Gum recession is a common condition that progresses over time if left untreated. When the gums pull back, they expose the tooth roots, which can cause sensitivity and make your teeth appear longer.
Recession can affect several or even all teeth, but sometimes it’s isolated to just one tooth.
In this article, we will discuss the causes of gum recession in one tooth and how to deal with it.
In this article...
What can trigger gum recession in one tooth?
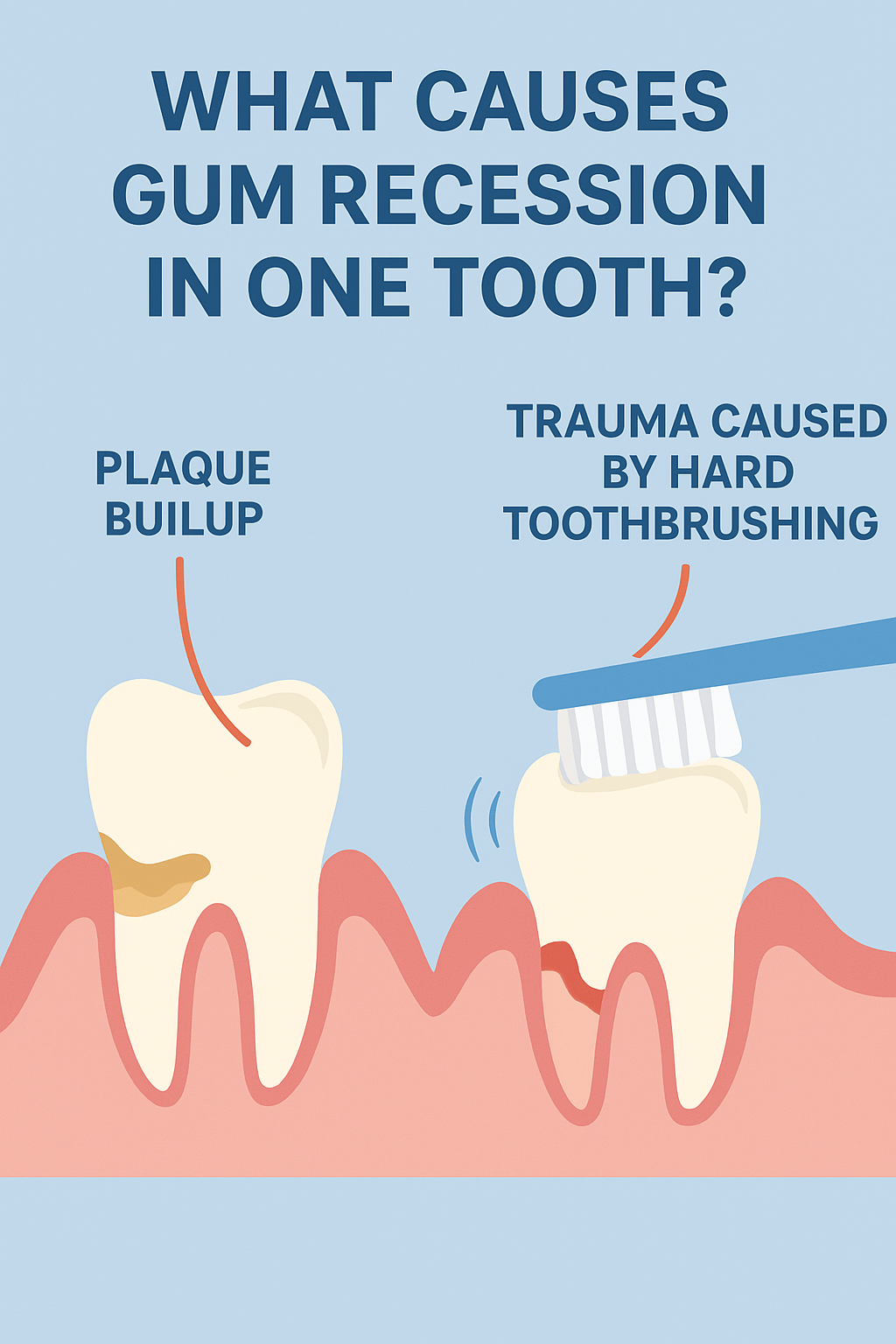
Gum recession is triggered by two main factors:
- Chronic trauma (or constant injury)
- Inflammation caused by gum disease
However, it's quite often a combination of both.
These main triggers can also work together with other secondary factors (we'll discuss later), exposing you to even greater risk.
Receding gums often progress slowly and gradually with age, which explains why they become more noticeable in older people. In some cases, they can progress rapidly and aggressively, leading to rapid and severe recession and loosening of the teeth.
Some forms of gum recession, especially those caused by ongoing irritation or trauma, can happen to anyone—even if you're young and brush regularly!
Here's how gum disease and trauma can cause your gums to pull away from your teeth:
1. Gum disease:
The main culprit here is dental plaque — a sticky, soft, whitish film that constantly forms on your teeth and along the gumline. It’s the perfect breeding ground for harmful bacteria.
To give you an idea: just 1 mg of plaque can contain over 100 million bacteria!
At first, plaque is so thin that you barely notice it. But skip brushing and flossing for just a couple of days, and it quickly thickens, showing up as a yellowish-white coating on your teeth.
From there, bacteria can seep under your gums, triggering inflammation. That's what we call the gingivitis stage. Your gums may look red, swollen, and bleed easily.
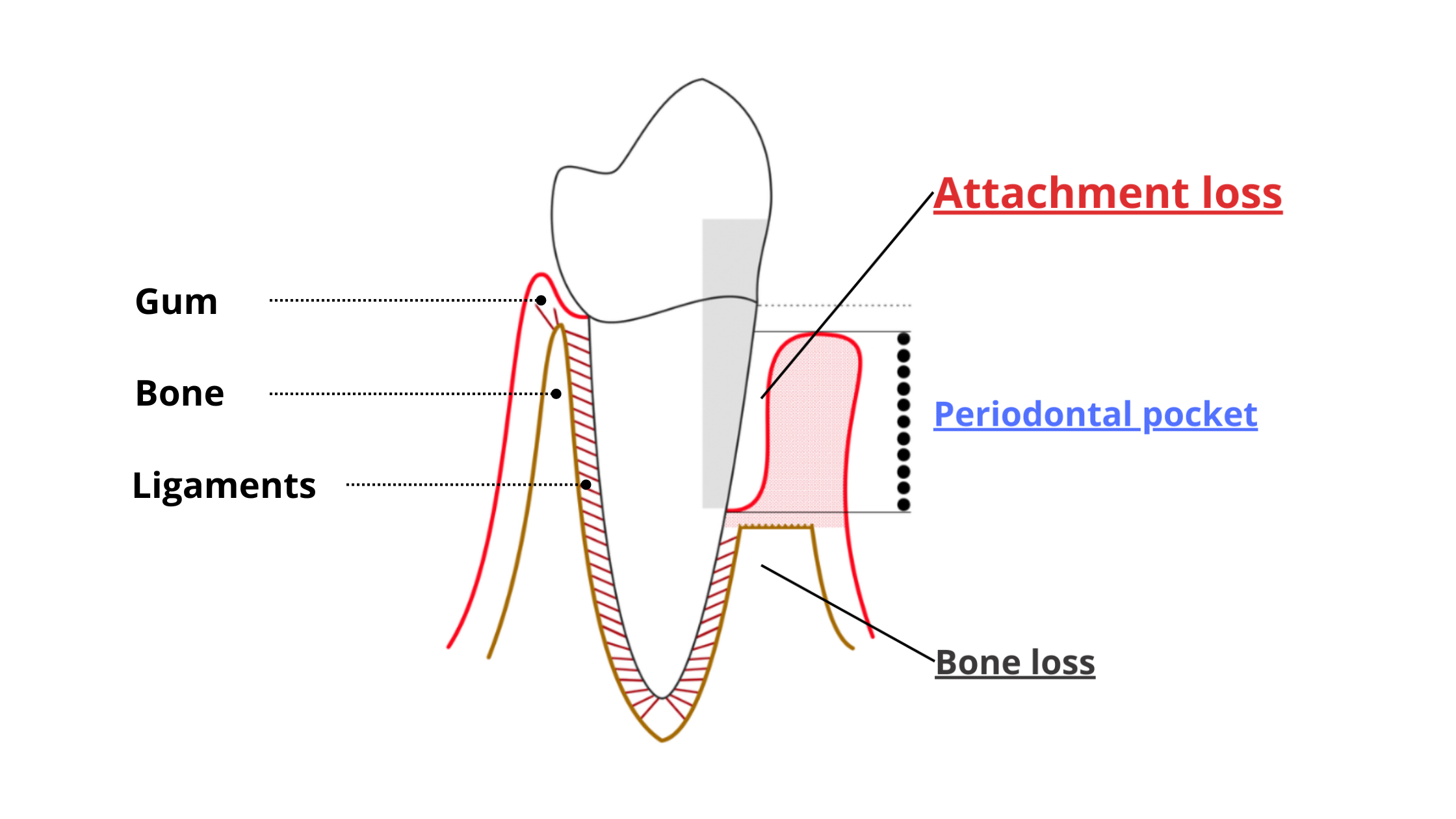
If the inflammation persists and worsens, it can start destroying the tissues that support your teeth — including the bone and ligaments that hold them in place. Gums also begin to recede. This advanced stage is called periodontitis.
Periodontitis usually affects several teeth at once and is the leading cause of tooth loss in adults. The picture below shows just how destructive it can be.
How do I know if my receding gums are due to gum disease?
If your receding gums are due to gum disease, you may also notice one or more of the following signs:
- Plaque buildup: Excessive plaque accumulation along the gumline is often a strong indicator of gum disease.
- Gum inflammation: Inflamed gums are characterized by redness, bleeding, swelling, and tenderness.
- Loose teeth: If you notice your teeth becoming increasingly loose or shifting position, it's a sign of bone loss and advanced gum disease.
- Changes in your bite: When the tissues that support your teeth are destroyed, your teeth can start to shift. You'll notice that your teeth don't line up and fit together like they used to.
2. Trauma:
Aside from gingivitis and periodontitis, gum recession can also occur without any sign of plaque buildup or inflammation. This happens in cases of trauma-induced gingival recession — and it can even affect people with excellent oral hygiene!
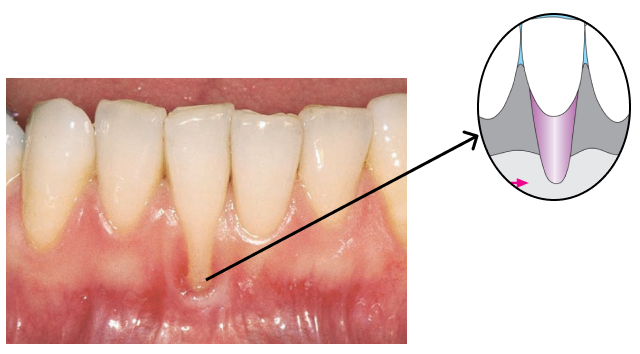
The most common cause is brushing too hard or using a hard-bristled toothbrush. If you brush this way, you are putting extra pressure on your gums, which can slowly make them pull away from your teeth and expose the roots. The picture below shows gum recession on an upper canine tooth caused by aggressive brushing.

With this type of damage, only one or a few teeth are typically affected.
When only one tooth is affected, gum recession often forms a ‘V’ or ‘U’ shape. It usually involves just the visible, front-facing part of the gum that’s exposed to trauma, while the gum between the teeth and surrounding areas stays healthy and intact.
Unlike inflammatory gum disease, the tissues that support the tooth — including the bone and ligaments — are not affected. That’s why this type of recession doesn’t lead to tooth loss.
However, if plaque builds up later, it can cause inflammation and combine with the trauma, making the problem even worse.
Gum recession on a single tooth can be caused by inflammation (periodontal disease) or trauma. Often, it’s a combination of several factors that increases the risk and makes the situation more complicated.
Other factors that increase the risk of recession in one tooth
Factors that increase the risk of gum recession in one tooth include:1. Anatomical Factor:
The shape and type of your gums by themselves do not directly cause recessions. However, when combined with other factors, they greatly increase the risk.
With triggers, such as gum disease or trauma, people with thin gums are more vulnerable to gum recession.
Sometimes, a tooth can have missing bone in certain spots around its root (called bone dehiscence and fenestration). When this happens, the gums don’t have enough support and may be more likely to recede.
Another anatomical feature that can cause recession is the labial frenulum. The labial frenulum is a piece of soft tissue that connects the lips to the gums. It is present at the top and bottom of the mouth.
When the frenulum is inserted too close to the gums, it can exert excessive tension, causing the gums to recede at that particular spot.

2. Ill-fitting restoration or dental work:
A large filling or a a poorly designed dental crown that extends beyond the gum line can also create irritation. This can cause more plaque to build up in the area and promote inflammation. As a result, the gum and bone supporting the crowned or restored tooth may break down and start to recede.
3. Orthodontic treatment:
Orthodontic treatment doesn’t directly cause gum recession, but if it’s not planned well, it can make existing risks worse.
If braces push a tooth too far from its supporting bone, the surrounding gums can become thinner. This results in weaker gums that are more likely to recede.
4. Dental crowding:
Crowded teeth can affect the shape of the bone and gums. When a tooth is tilted too far forward, it may lack bone and gum support in the front part. This can make the gums in this area less resistant and more prone to damage.
A misaligned tooth can also make brushing and flossing more difficult, promoting plaque build-up and inflammation.
Sometimes, dental crowding can interfere with the bite, resulting in an uneven distribution of chewing forces between the teeth. This is the case when only a few teeth touch when you chew, while others do not. This can lead to overloading and increased stress on the tissues supporting the teeth.
Preventing and treating gum recession in one tooth
Preventing and stopping gum recession begins with addressing any underlying causes.Having thin gums or other risk factors doesn’t mean gum recession is inevitable.
The real problem comes from triggers like plaque-induced gum disease and ongoing irritation — and those are things you can control.
Here are some tips to stop and treat gum recession:
1. Deep Dental Cleaning if Gum Disease Is the Culprit:
Advanced gum disease cannot be cured at home and will not heal on its own. When it progresses to the point of causing gum recession and bone loss, delaying treatment will only result in more damage.
A professional deep dental cleaning, also known as scaling and root planing, is the only way to prevent advanced gum disease from getting worse.
This procedure cleans deep beneath the gum line and removes hidden bacteria that regular brushing and flossing cannot reach. Left untreated, gum disease can become more destructive, potentially leading to loose teeth or even tooth loss.
1. Brushing Technique:
Brush your teeth regularly using the correct technique to control plaque buildup. Choose a soft-bristle toothbrush and gently brush your teeth in circular motions.
Avoid aggressive horizontal brushing strokes, as they can damage your gums.
Also, hold your toothbrush at a 45-degree angle, directing the bristles toward the gum line. This helps clean both your teeth and gums effectively while promoting healthy blood flow.
2. Interdental Cleaning:
The spaces between your teeth are hard to reach with a toothbrush alone. That’s why cleaning between your teeth once a day using an interdental tool should be part of your oral hygiene routine.
You can choose from dental floss, interdental brushes, or water flossers—pick the one you feel most comfortable using.
3. Regular Dental Checkups:
Make it a habit to visit your dentist regularly, at least twice a year, even if you don't experience any noticeable issues. These checkups can help catch early signs of gum disease or other dental issues so you can treat them quickly.
Remember, early treatment is easier, more effective, and less costly.
4. Enhance Your Diet for Optimal Gum Health:
A healthy, balanced diet rich in nutrients is not only essential for your overall health but also for strong, healthy gums. Studies have shown that deficiencies in certain nutrients—especially vitamin C, D, B9, and omega-3 fatty acids—are directly linked to severe forms of gum disease.
Getting enough vitamins and minerals helps your body fight oxidative stress and chronic inflammation, which are the driving forces behind the destructive effects of gum disease.
5. Address Dental Alignment:
As we’ve said, crooked or misaligned teeth can contribute to gum recession. If you think you have dental alignment issues, it’s a good idea to see an orthodontist.
Straightening your teeth can help improve bone and gum thickness, distribute chewing pressure more evenly, and reduce your overall risk of gum recession.
6. Ask Your Dentist if You Can Benefit From a Gum Graft:
Once all underlying causes and risk factors have been addressed and gum disease is stable, it may be time to consider covering exposed roots.
If gum recession is causing sensitivity or affecting your smile, talk to your dentist or periodontist to see if you can benefit from a gum graft.
There are several techniques, but the most common involves taking a small piece of tissue from another part of your mouth—usually the palate (roof of your mouth)—and placing it over the areas where the gums have receded.
Gum grafting not only reduces symptoms but also strengthens your gums and helps prevent further recession.
The benefits are not just short-term but also long-lasting.
- Color atlas of dental medicine periodontology
- Gingival recession: its causes and types, and the importance of orthodontic treatment https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4944726/
- Etiology and occurrence of gingival recession - An epidemiological study https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4753713/
- Studies of the predominant cultivable microbiota of dental plaque - ScienceDirect