How Plaque Turns into Tartar and Damages Your Teeth & Gums
 Dental plaque is the biggest culprit behind cavities, gum disease, oral infections, and even the failure of dental treatments like root canals, implants, and crowns.
Dental plaque is the biggest culprit behind cavities, gum disease, oral infections, and even the failure of dental treatments like root canals, implants, and crowns.
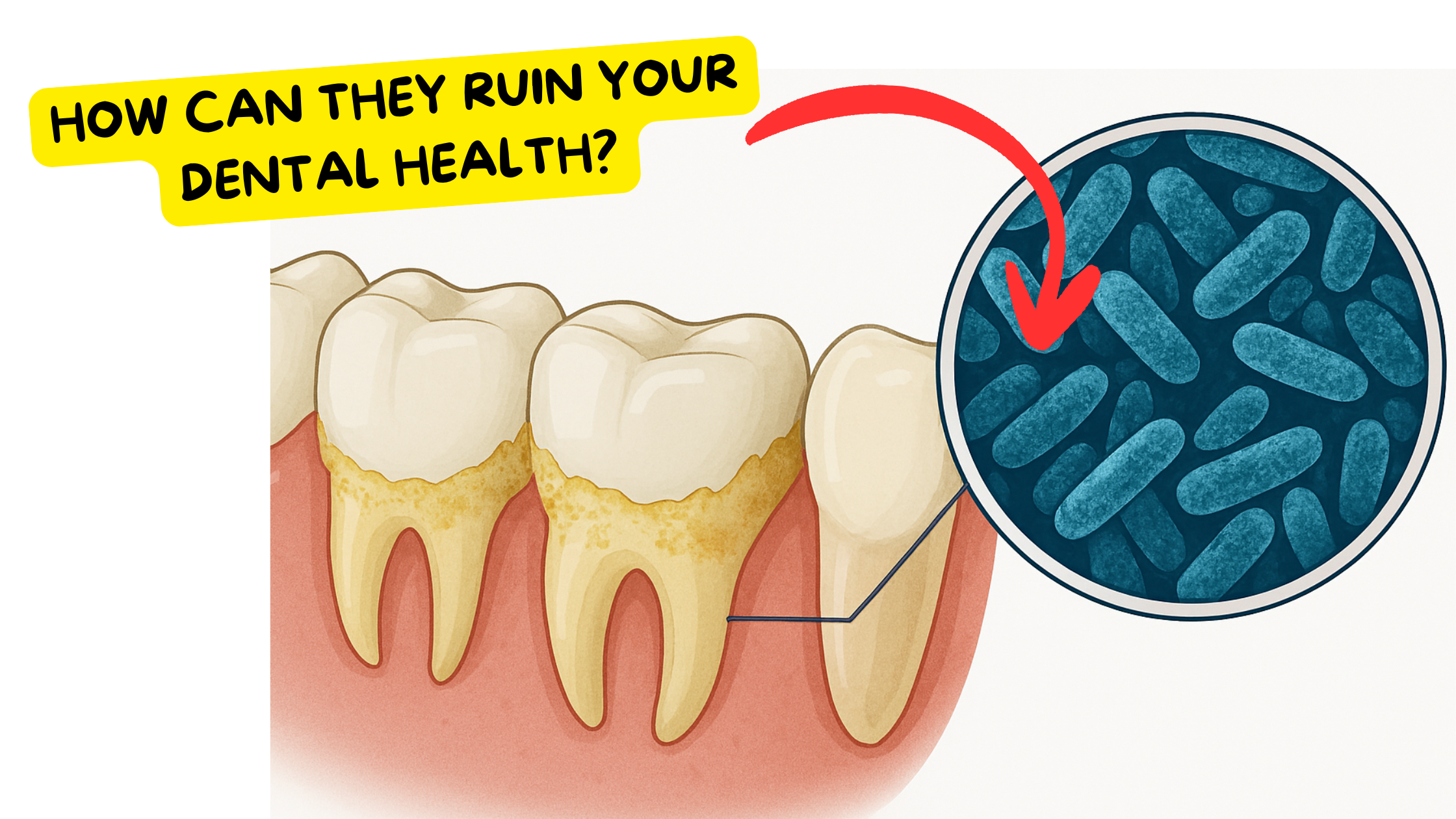
Plaque is actually a type of biofilm — a thin layer made up of billions of bacteria that sticks to your teeth and gums.
Bacteria don’t just form plaque by accident. It’s a highly organized survival strategy that allows them to work together, resist attacks, and thrive.
Bacteria living in plaque can be up to 1,000 times more resistant to antimicrobials than free-floating bacteria. This makes them more aggressive and even harder for your immune system to fight off.
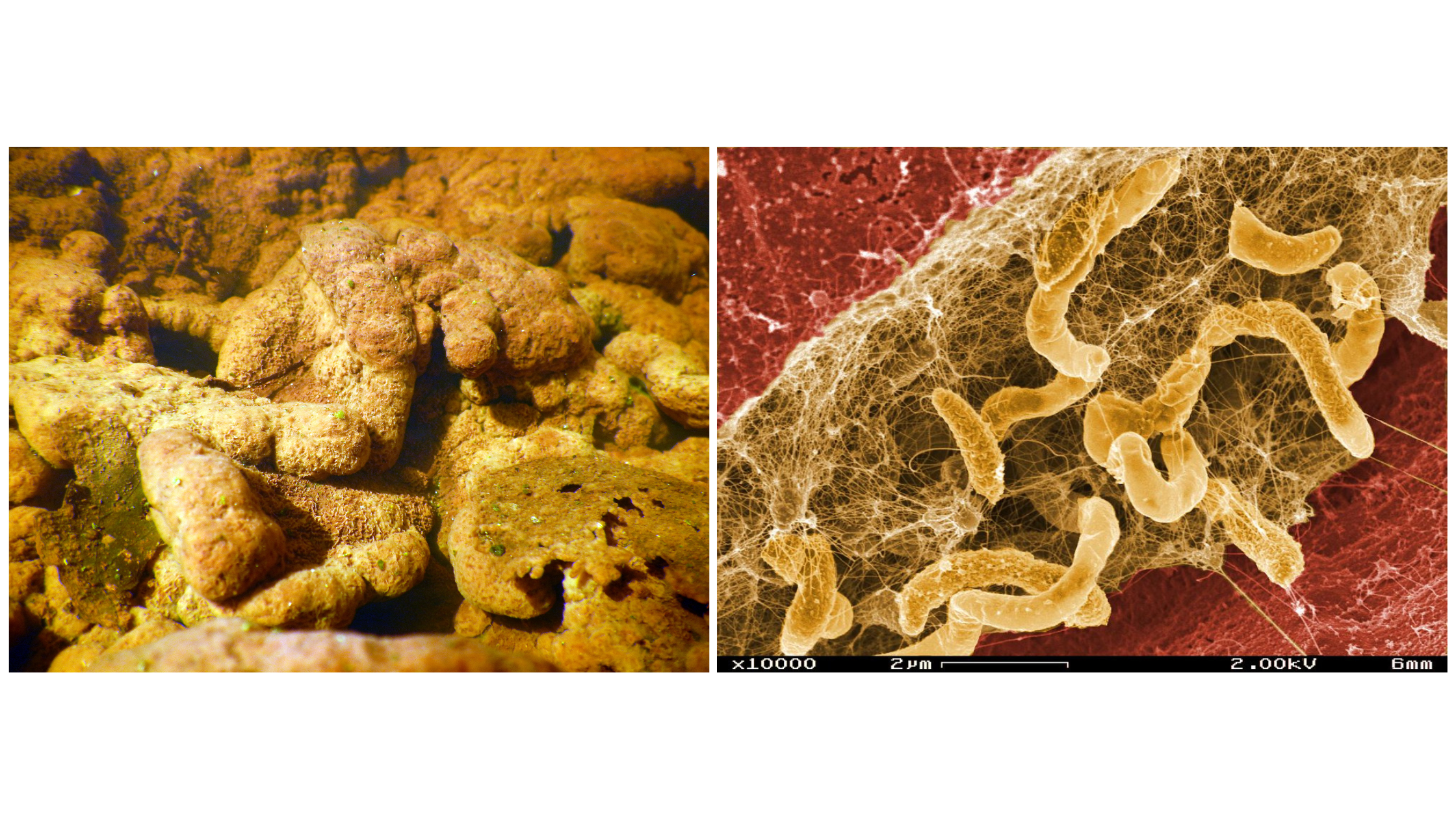
Bacteria form biofilms in many environments whenever conditions allow — not just in your mouth. You can see them in other places, such as on river rocks or inside water pipes.
When plaque isn’t removed regularly, it thickens and can harden when it absorbs minerals from your saliva and food. This hardened form is called tartar — a calcified, rough mass that’s stickier and much harder to remove.
So how does dental plaque form? How is it different from tartar? And how can it damage your oral health if not controlled regularly? We’ll break it down in detail, step by step.
In this article:
1. How Does Plaque Form on Your Teeth and Gums (and What Does It Look Like)?
2. How Plaque Harms Your Teeth and Gums
3. From Plaque to Tartar: The Key Differences
4. Why Tartar Should Be Removed
5. How to Keep Plaque and Tartar Under Control
How Does Plaque Form on Your Teeth and Gums (and What Does It Look Like)?
Bacteria can’t form plaque without saliva. It might sound surprising, but the same saliva that protects your teeth and gums also helps plaque form— the main culprit behind cavities and gum disease.Proteins and other components in your saliva constantly coat your teeth, forming a thin, invisible layer called the acquired enamel pellicle. This layer forms within minutes after you brush. While it shields our teeth, it also provides the perfect foundation for bacteria to attach to.
Minutes or hours later, bacteria begin to accumulate on this film, gradually forming a thicker layer — plaque.
At first, plaque is so thin you might not notice it. But you can make it visible by using disclosing tablets, which dye the plaque and make it stand out.

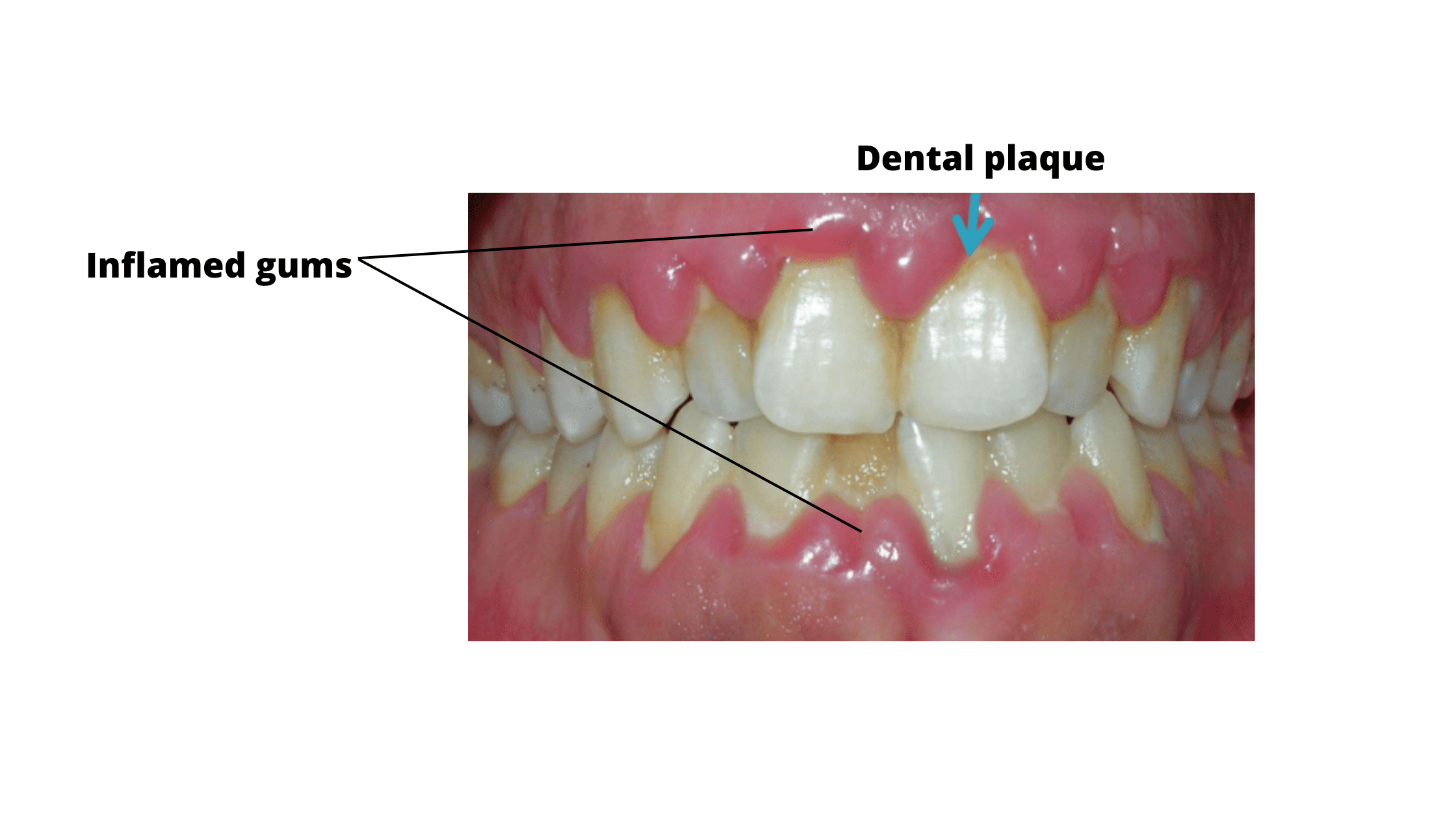
Plaque tends to build up most on the chewing surfaces of your teeth, along the gumline, and between teeth. All of these are harder to clean and offer bacteria a safe hiding place.
As more bacteria collect and the plaque thickens, it becomes more visible. It appears as a whitish or yellowish film.
Mature forms of plaque are densely packed with bacteria. Just 1 milligram of plaque can contain up to 100 million bacteria or more!
No matter how well or how often you brush and floss, plaque will always return. It’s a nonstop process that starts just minutes after a thorough cleaning.
How Plaque Harms Your Teeth and Gums
There’s no one answer—how bad plaque can be depends on the types of bacteria living in it.You’ve probably seen people who don’t brush as often as they should, but somehow never get cavities or gum disease. That’s because, in a healthy mouth, there’s a balance: friendly bacteria keep harmful ones in check.
As long as this balance remains, plaque stays harmless and nothing bad happens.
But when this balance is disrupted and “bad” bacteria take over, plaque becomes harmful and oral diseases result.
This can create a domino effect, because harmful bacteria can team up, become more resistant and aggressive, and overpower the friendly bacteria.
Here’s how plaque can lead to cavities and gum disease:
Cavities
Cavities happen when specific bacteria that produce acids take over and dominate.
These bacteria use sugar as their main energy source. As they break down sugar, they release acids that attack your teeth, causing decay.
What makes it tricky is that when these bacteria produce too much acid, they create an acidic environment in your mouth. Only the harmful bacteria that can survive in this acidity thrive, while the good ones die off.
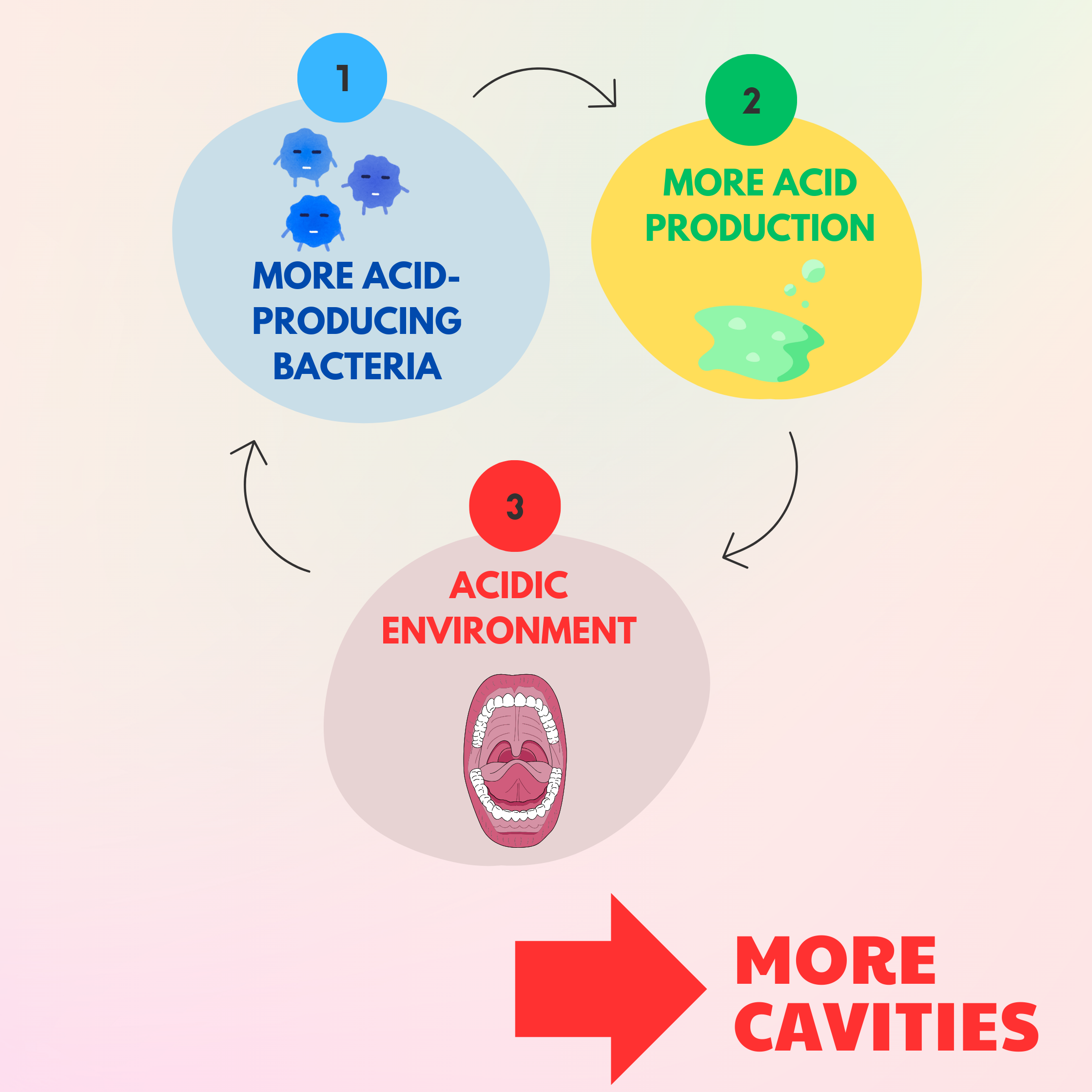
This sets up a vicious cycle: cavity-causing bacteria grow stronger and outnumber the friendly bacteria. And more acid-producing bacteria means more cavities.
Factors that fuel this cycle and turn plaque into a cavity-making machine:
- Dry mouth
- Poor oral hygiene
- Mouth breathing (which causes chronic dry mouth)
- Eating or drinking sugary and acidic foods and drinks too often
- Frequent snacking between meals
Gum Disease
The most aggressive bacteria that damage the tissues supporting your teeth have one thing in common: they thrive in oxygen-free environments. These are called anaerobic bacteria.
The narrow, deep spaces between your teeth and gums (along the gumline) are perfect hiding spots for these anaerobic bacteria because these areas naturally have less oxygen.
When plaque builds up along the gumline and isn’t removed regularly, some of it can push deep into those spaces. Since these areas are difficult to clean with a toothbrush, plaque can remain hidden, allowing harmful bacteria to grow. The first signs are redness, swelling, and bleeding gums (inflammation).
If your immune system fails and pathogenic anaerobic bacteria win, the disease can progress to severe forms of gum disease. This can cause your gums, bone, and ligaments that hold your teeth in place to pull away and be destroyed.
From Plaque to Tartar: The Key Differences
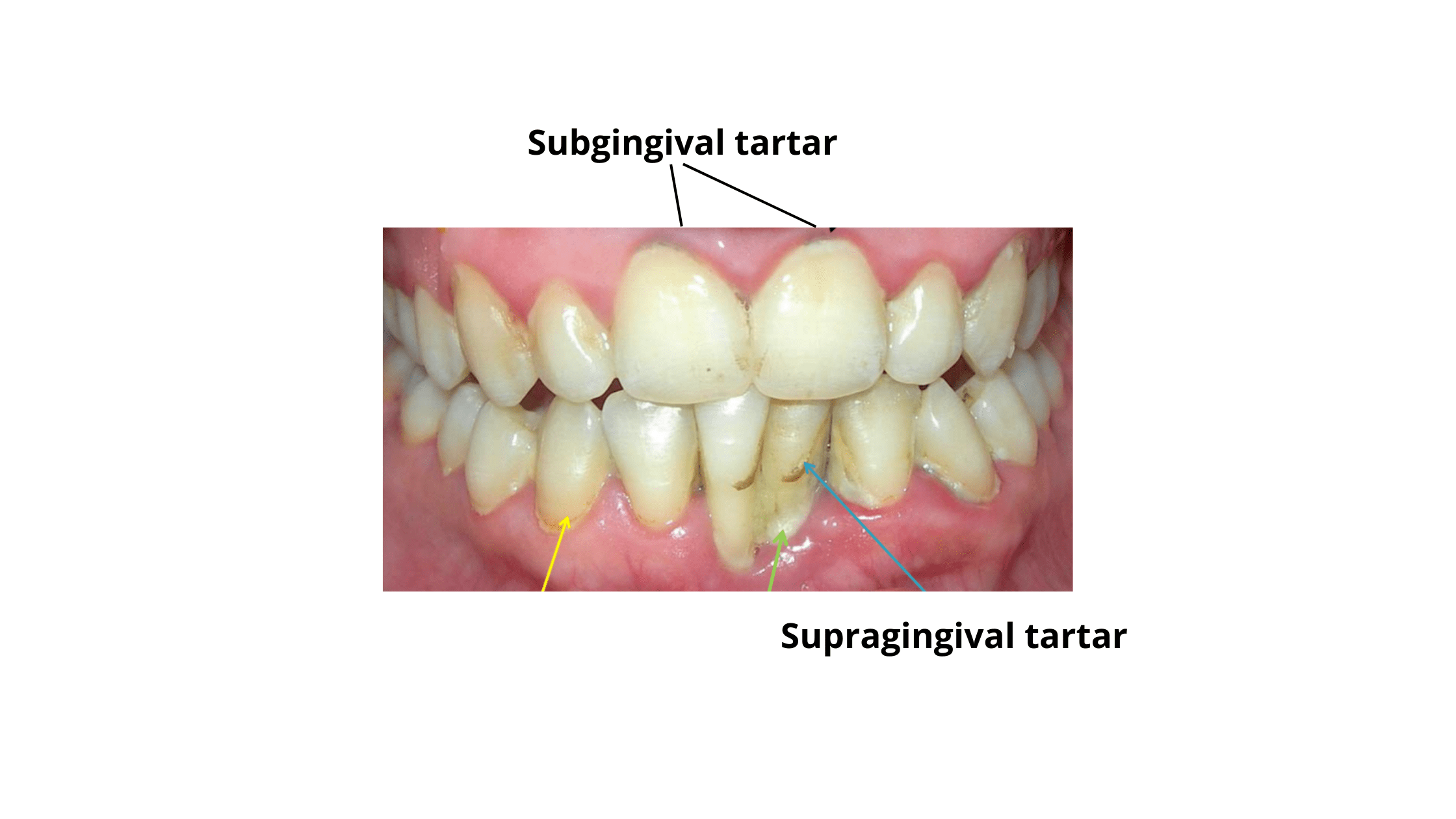
Plaque doesn’t always turn into tartar. Some people are more prone to tartar buildup than others.Tartar forms when plaque absorbs minerals from food and saliva, hardening and calcifying on your teeth.
This is more common in individuals whose saliva is naturally rich in minerals like calcium and phosphorus. Tartar also needs an alkaline (not acidic) environment to form.
Interestingly, those who are more prone to tartar buildup often have a lower risk of tooth decay and cavities.
That’s because the two conditions needed for tartar formation—mineral-rich saliva and an alkaline environment—are also big factors that protect teeth from cavities.
The area most likely to develop tartar is the back side of the lower front teeth, which face the major salivary gland ducts.
What’s the difference between plaque and tartar?
- Plaque is soft; tartar is hard.
- Plaque can be brushed away easily; tartar is sticky and much harder to remove.
- Tartar usually looks darker than plaque.
- You can control plaque buildup at home, but tartar requires special tools used by your dentist.
Why Tartar Should Be Removed
While tartar can be a sign of a lower risk of cavities, that doesn’t mean it’s good to have. If not removed, tartar can be a major risk factor for severe gum disease.Tartar is rough and porous, which means it can easily trap more plaque. It makes cleaning your teeth and gums much harder because it can block your floss and toothbrush from reaching certain areas.
Its hard texture can also irritate your gums directly, causing inflammation.
Additionally, tartar provides a perfect breeding ground for harmful anaerobic bacteria that cause gum disease. Because it’s extremely sticky and stays on your gums longer, it gives harmful bacteria plenty of time to work their way deeper into the tissues.
For these reasons, leaving tartar in place is never a good idea. The only way to remove it is through a professional cleaning procedure called scaling, performed by your dentist.
How to Keep Plaque and Tartar Under Control
You can’t stop plaque from forming—just like you can’t eradicate all bacteria from Earth.But you can keep it under control and prevent it from taking over your mouth.
The best way to control plaque buildup is by physically or manually removing it through good oral hygiene—brushing and flossing regularly.
Since plaque forms constantly, consistency is key.
Another important step is maintaining a healthy oral microbiome to prevent harmful bacteria from taking over.
Here are some tips for better plaque and tartar control:
- Brush at least twice a day for a full two minutes, using fluoride toothpaste or alternatives like hydroxyapatite.
- Floss once a day using dental floss, interdental brushes, or a water flosser.
- Clean your tongue daily with your toothbrush or, ideally, a tongue scraper.
- Limit sugary foods and drinks, as they feed cavity-causing bacteria.
- Avoid snacking between meals.
- Fix dry mouth by staying hydrated and chewing sugar-free gum between meals.
- Support friendly bacteria with probiotic foods like yogurt, kefir, pickles, and other fermented foods. Just make sure they’re sugar-free to avoid feeding harmful bacteria.
- Visit your dentist regularly, every six months, for check-ups. If you’re prone to tartar buildup, you might need more frequent professional cleanings.
-
Antimicrobial resistance of Pseudomonas aeruginosa biofilms - ScienceDirect
https://www.sciencedirect.com/science/article/pii/S1286457903002260 -
[Does food affect tartar deposition?] - PubMed
https://pubmed.ncbi.nlm.nih.gov/34747162/ -
Impact of Dental Plaque Biofilms in Periodontal Disease: Management and Future Therapy | IntechOpen
https://www.intechopen.com/chapters/56535 -
Dental plaque as a biofilm and a microbial community – implications for health and disease | BMC Oral Health
https://link.springer.com/article/10.1186/1472-6831-6-s1-s14