Why Bone Loss Happens in Teeth And How You Can Fix It
 Bone loss around teeth can happen to anyone at some point, whether due to gum (periodontal) disease, trauma, tooth loss, or simply the natural aging process.
Bone loss around teeth can happen to anyone at some point, whether due to gum (periodontal) disease, trauma, tooth loss, or simply the natural aging process.
While it can be a natural part of aging, premature bone loss is a real issue. In this case, something causes the bone to shrink faster than it should. It might not seem like a big deal, but over time it can lead to serious dental problems — such as shifting or loosening of teeth, bite issues, and even tooth loss.
From a treatment point of view, bone loss also makes tooth replacement and restorations more challenging, since options like dental implants rely on strong, healthy bone for support.
If you’ve noticed signs of bone loss around your teeth, the first step is to know what’s causing it and address the root of the problem as early as possible. That’s exactly what we’ll discuss— along with the most effective treatment options and techniques to help rebuild and restore lost bone.
In this article...
1. What is the bone that supports our teeth?
2. What causes bone loss in the teeth?
3. Bone Loss After Tooth Loss: What Are My Options?
4. Bone Loss Due to Gum Disease: Treatment Options
5. How to stop and prevent further bone loss?
What is the bone that supports our teeth?
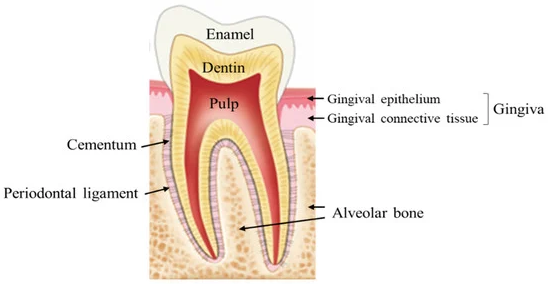 The bone that supports our teeth is called the alveolar bone. It surrounds and holds each tooth in place with the help of tiny fibers known as periodontal ligaments.
The bone that supports our teeth is called the alveolar bone. It surrounds and holds each tooth in place with the help of tiny fibers known as periodontal ligaments.
What makes this bone unique is its ability to change shape and volume depending on what happens to your teeth. For instance, when you chew, the pressure stimulates the bone underneath, helping it stay strong and healthy.
However, when one or more teeth are lost, that natural stimulation stops. As a result, the bone begins to shrink and weaken over time.
Bone loss can also occur due to gum disease, but for a different reason. In this case, harmful bacteria release toxins that trigger intense inflammation, gradually eroding the bone and destroying other supporting tissues. The result is loose teeth that may eventually fall out. In fact, gum disease is the leading cause of tooth loss in adults.
What Causes Bone Loss in Teeth?
Several factors can trigger or worsen bone loss around the teeth. Some act directly on the bone, while others have an indirect effect — and often, they work together.1. Direct Causes of Bone Loss
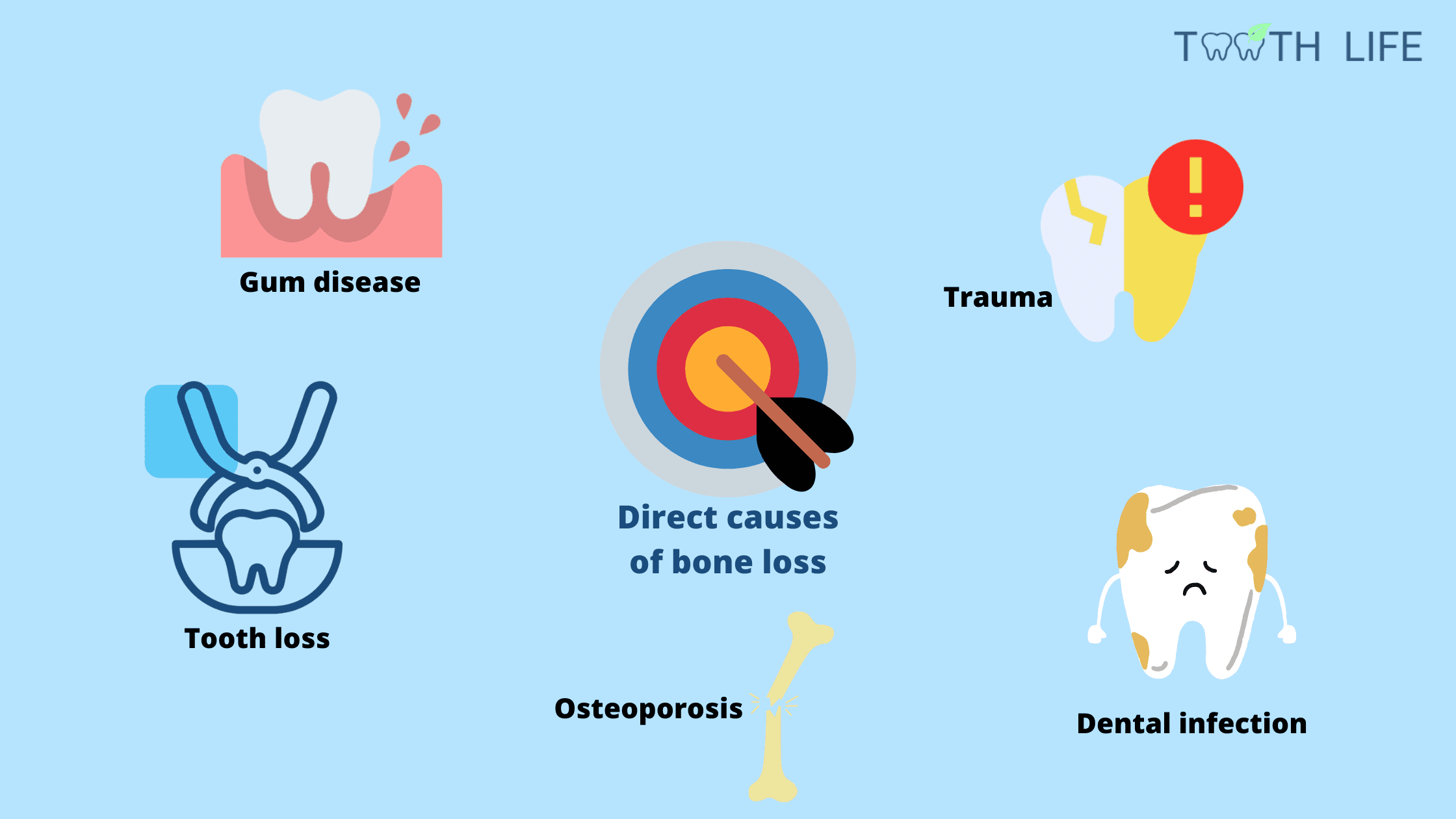
Tooth Loss
When a tooth is lost, the bone that once supported it begins to shrink — especially during the first year. The more teeth you lose, the greater the bone loss becomes.
If the missing tooth isn’t replaced with an implant, this bone loss continues over the years.
But why an implant in particular? Because it’s the only replacement option that actively stimulates the bone and prevents it from resorbing. Other options, like bridges and dentures, only replace the visible part of the missing teeth and don’t stimulate the underlying bone.
If the missing tooth isn’t replaced with an implant, this bone loss continues over the years.
But why an implant in particular? Because it’s the only replacement option that actively stimulates the bone and prevents it from resorbing. Other options, like bridges and dentures, only replace the visible part of the missing teeth and don’t stimulate the underlying bone.
Gum Disease
If not treated, gum disease can severely and permanently damage the tissues that hold your teeth in place — including the supporting bone.
You might notice your teeth becoming loose, shifting, or developing unusual gaps, and in some cases, even changes in your bite.
You might notice your teeth becoming loose, shifting, or developing unusual gaps, and in some cases, even changes in your bite.
Tooth Infection
The most common cause is a cavity. Bacteria gradually eat through the hard layers of the tooth and eventually reach the nerve.
Once inside, the infection can spread beyond the root tip, forming an abscess. The buildup of pus, bacteria, and inflammation can destroy nearby bone tissue and may ultimately lead to tooth loss.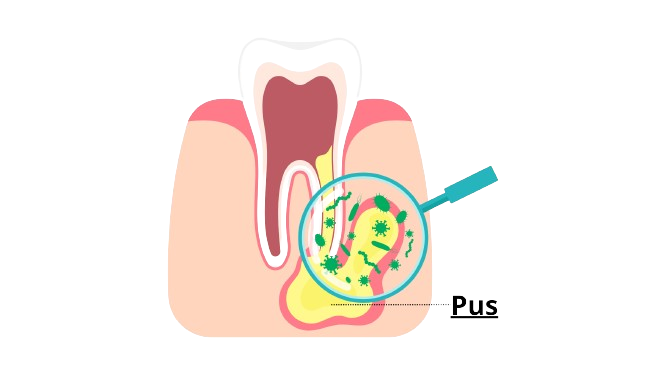
Once inside, the infection can spread beyond the root tip, forming an abscess. The buildup of pus, bacteria, and inflammation can destroy nearby bone tissue and may ultimately lead to tooth loss.
Osteoporosis
Osteoporosis is a condition that weakens bones by reducing their density, making them more porous and fragile — and the jawbone is no exception.
According to one study, the prevalence of osteoporosis in adults aged 50 and over increased from 9.4% in 2007–2008 to 12.6% in 2017–2018.
According to one study, the prevalence of osteoporosis in adults aged 50 and over increased from 9.4% in 2007–2008 to 12.6% in 2017–2018.
2. Indirect Causes of Bone Loss
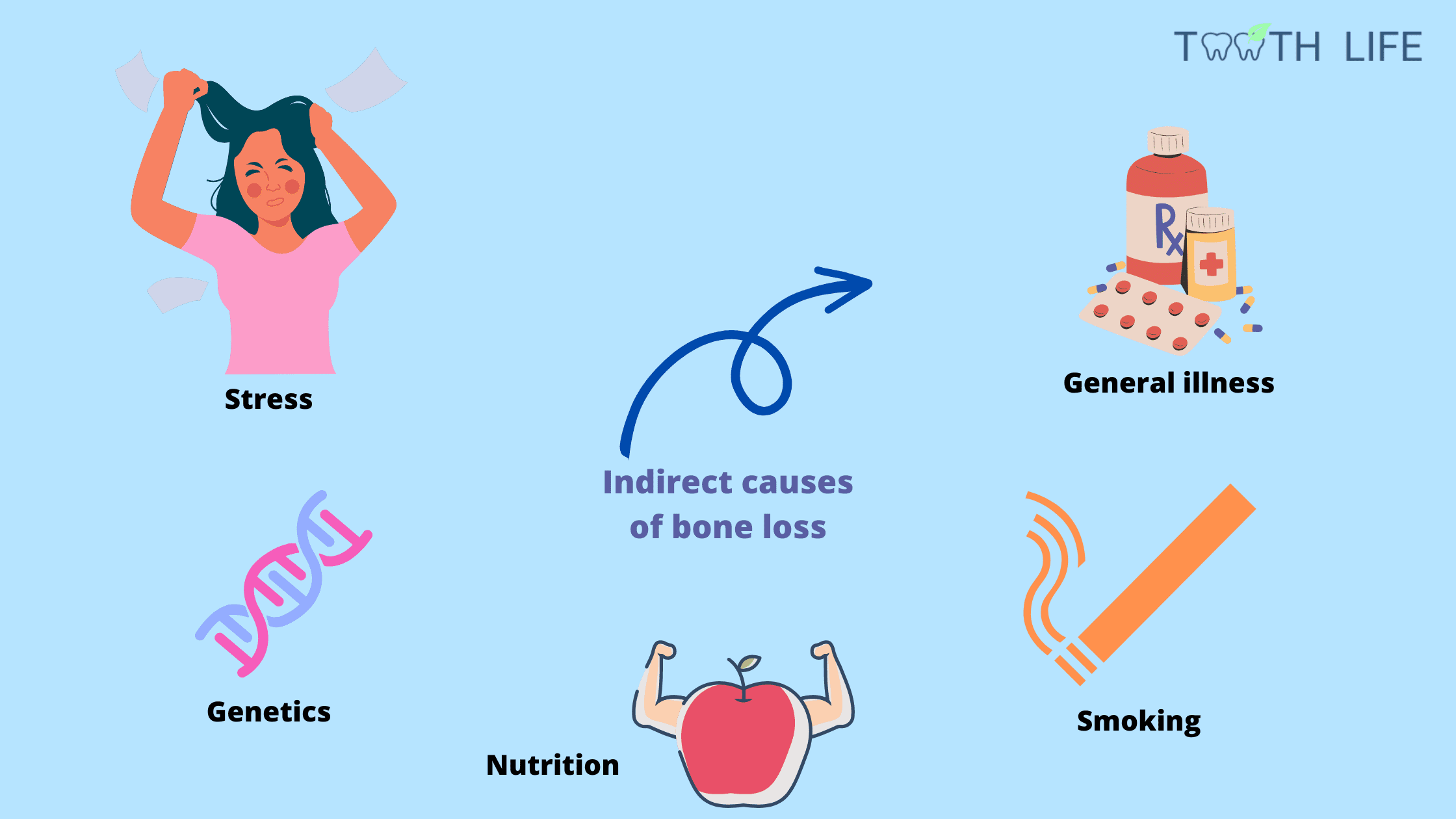
Medical Conditions That Weaken the Immune System
Certain health conditions — such as diabetes, blood disorders, HIV infection, and cancers or their treatments — can weaken the immune system.
When the immune system is not working properly, it struggles to fight off harmful bacteria, making gum disease and other dental infections more aggressive and harder to control.
When the immune system is not working properly, it struggles to fight off harmful bacteria, making gum disease and other dental infections more aggressive and harder to control.
Stress
Stress affects more than just your mood — it impacts your mouth and overall health, too.
Short-term stress is normal and can even be a good thing. But chronic, long-lasting stress compromises the immune system and promotes chronic inflammation throughout the body.
Studies show that people under constant stress are more likely to develop severe gum disease and experience greater tissue and bone destruction.
Short-term stress is normal and can even be a good thing. But chronic, long-lasting stress compromises the immune system and promotes chronic inflammation throughout the body.
Studies show that people under constant stress are more likely to develop severe gum disease and experience greater tissue and bone destruction.
Smoking
Tobacco contains hundreds of harmful chemicals that damage cells and tissues. Since the mouth is the first to be exposed to tobacco smoke, it’s also the first to suffer.
Smokers are up to six times more likely to develop advanced gum disease than non-smokers, and they tend to experience faster bone loss, gum recession, and tooth loss.
Smokers are up to six times more likely to develop advanced gum disease than non-smokers, and they tend to experience faster bone loss, gum recession, and tooth loss.
Nutrition
A diet lacking in essential nutrients can affect how well your body maintains healthy bones and gums.
- Calcium and Vitamin D: Help preserve bone density and support remineralization.
- Vitamin C: Is the fuel for collagen production — the main building block protein for gums and bone. A severe deficiency is linked to gum inflammation and may promote advanced gum disease.
Teeth Crowding
Crowded or overlapping teeth are harder to keep clean. Plaque tends to build up in tight spaces, which can worsen inflammation and increase the risk of gum disease and bone loss.
Bruxism
Bruxism is the habit of grinding or clenching teeth, often during sleep. The constant pressure can not only wear down your teeth but also strain their supporting tissues, which can worsen existing bone loss and gum problems.
Bone Loss After Tooth Loss: What Are My Options?
Bone loss can begin within just a few months after losing one or more teeth.The longer you wait to replace a missing tooth, the more bone is lost, making dental implant placement difficult or even impossible.
The following bone augmentation techniques are commonly used to rebuild lost bone and prepare the site for implant placement. Here’s a quick overview of each one:
1. Guided Bone Regeneration (GBR)
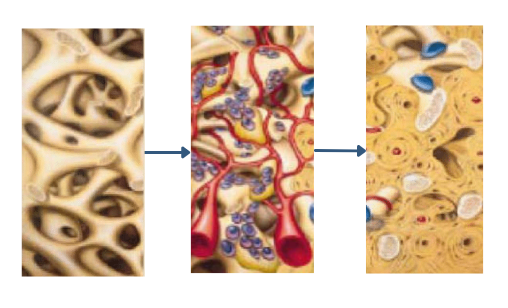 In this procedure, your dentist opens the gum to expose the bone, then places a bone graft material over the area.
In this procedure, your dentist opens the gum to expose the bone, then places a bone graft material over the area.
A special membrane covers the graft to protect it and guide new bone growth during healing. Finally, the gum tissue is repositioned and stitched.
2. Bone Block Grafting
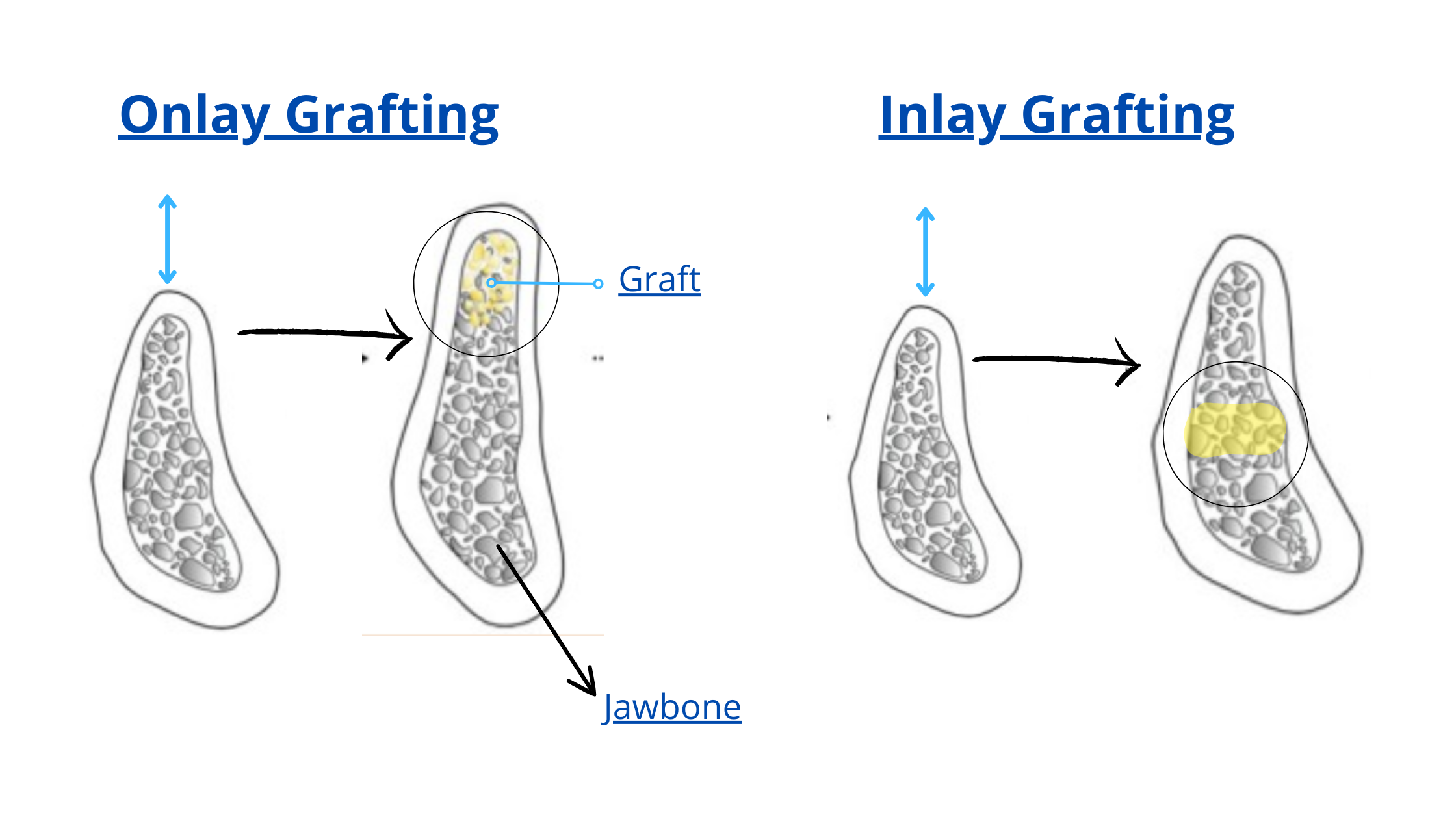 This method uses a piece or "block" of bone, either taken from your own body (autograft) or from a human donor (allograft).
This method uses a piece or "block" of bone, either taken from your own body (autograft) or from a human donor (allograft).
The bone block is fixed into the deficient area to increase volume and strength.
Depending on your case, your dentist may recommend an onlay graft (on top of existing bone) or an inlay graft (graft placed within the bone).
3. Ridge Expansion
When the bone ridge is too narrow to place implants, it can be widened surgically using special instruments.
The biggest advantage of this technique is that implants can often be placed immediately, at the same time, reducing overall treatment time.
The biggest advantage of this technique is that implants can often be placed immediately, at the same time, reducing overall treatment time.
4. Segmental Osteotomy
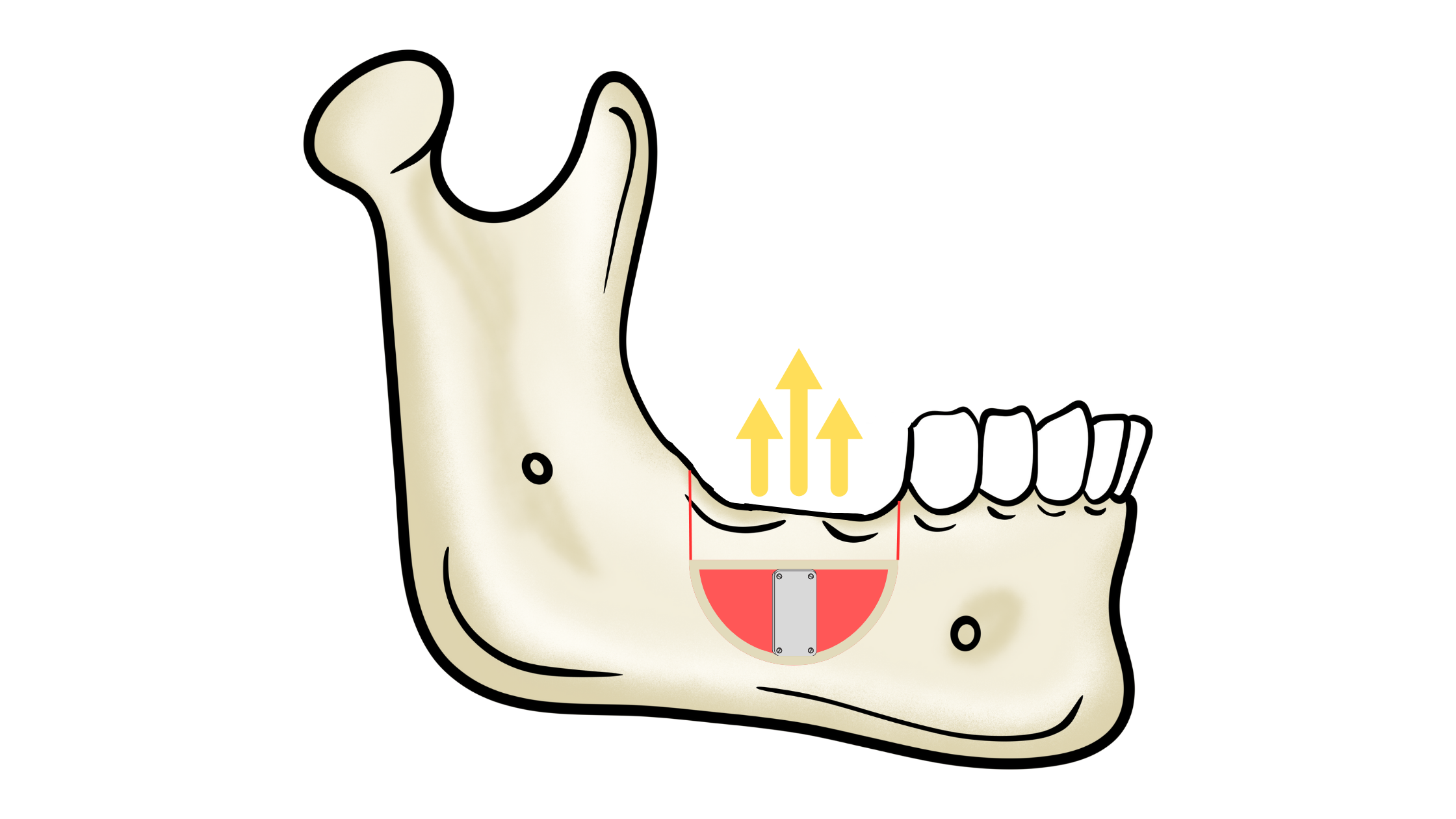
This technique is used when bone height is insufficient, with enough width.
It involves cutting and repositioning a segment of bone upward to increase height, then stabilizing it in place.
5. Sinus Lifting
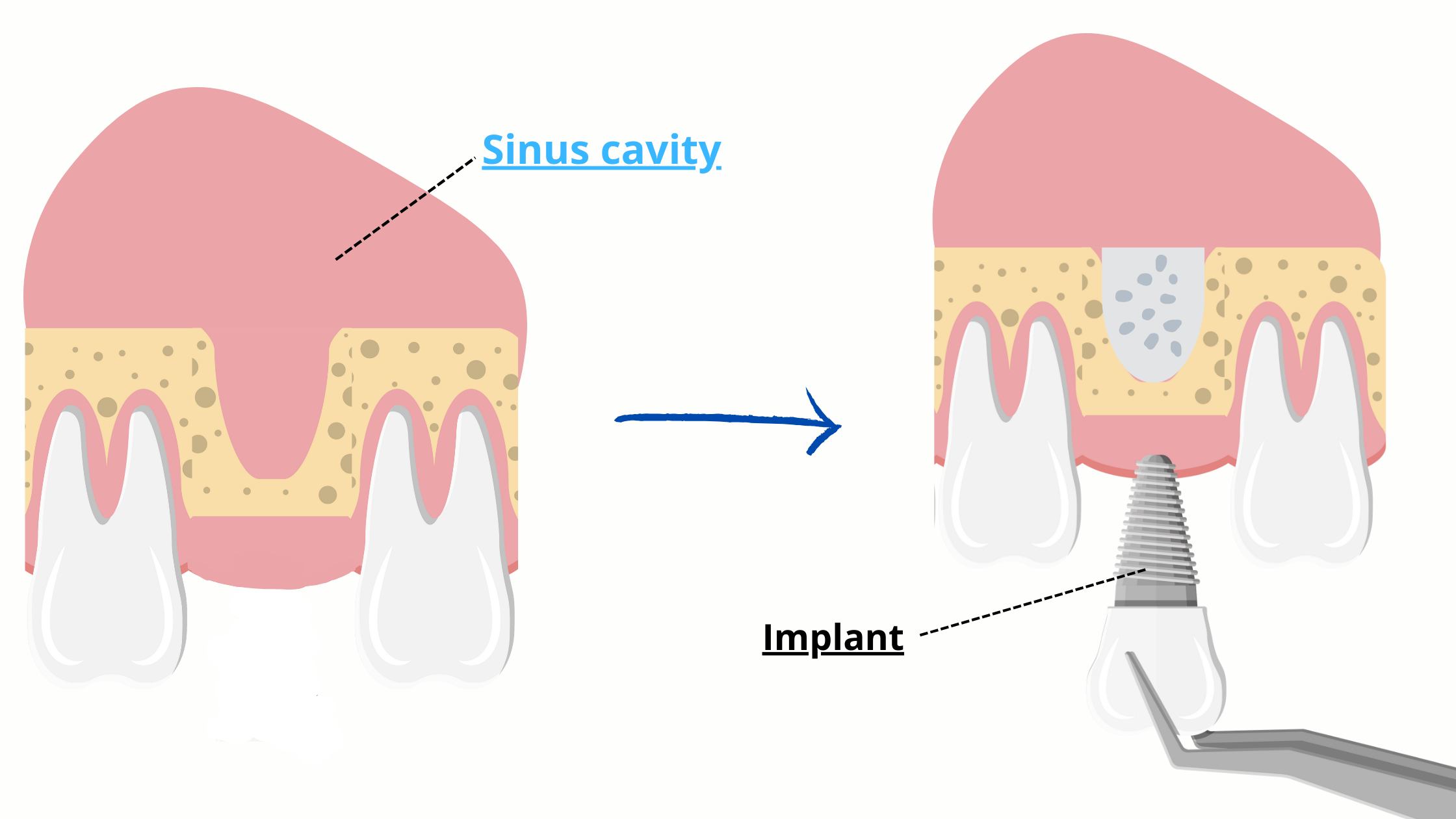
In the upper jaw, loss of the back teeth can cause the sinus cavity to expand, reducing bone volume.
A sinus lift (or sinus augmentation) creates space between the sinus and the jawbone, which is then filled with graft material to build up enough bone for implant placement later on.
A sinus lift (or sinus augmentation) creates space between the sinus and the jawbone, which is then filled with graft material to build up enough bone for implant placement later on.
Bone Loss Due to Gum Disease: Treatment Options
Treating bone loss caused by gum disease requires a different approach.In most cases, non-surgical treatment is the first line of treatment— and it’s often enough to stop the disease and allow the tissues to heal naturally.
Surgical treatment may be considered when the damage is more extensive or when non-surgical options haven’t been successful.
Regardless of the method used, maintaining excellent oral hygiene is a prerequisite for long-term success and to prevent the disease from coming back.
Here are the most common treatment options for bone loss due to gum disease:
- Deep Teeth Cleaning (Scaling and Root Planing)
Your dentist may recommend a deep cleaning, which involves two steps: scaling and root planing.
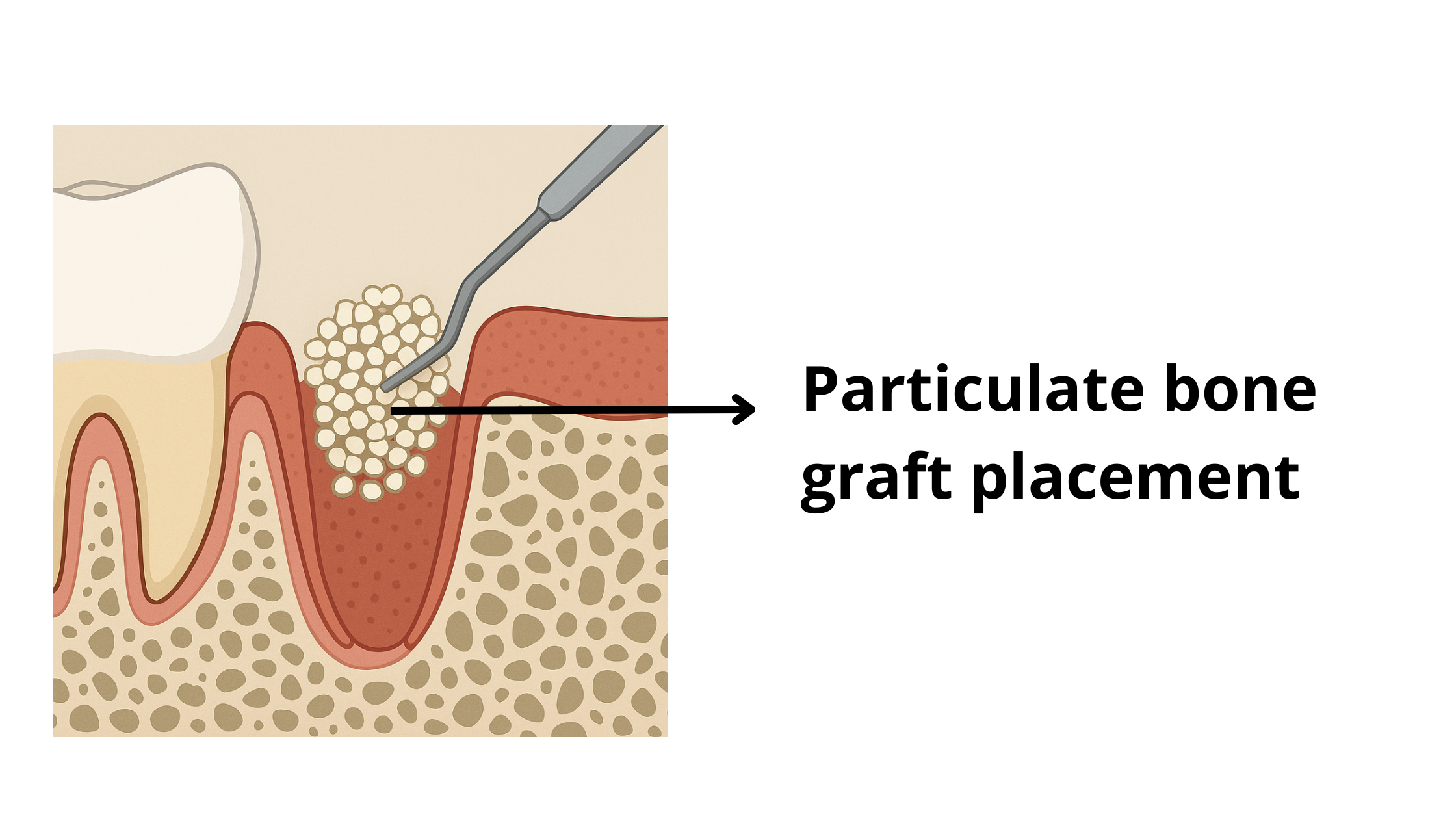
This procedure removes plaque and tartar from above and below the gum line — the main culprits behind gum disease. Once the surfaces are clean, the gums, ligaments, and bone have a better chance to heal and reattach to the teeth. - Bone grafting
In cases of severe bone loss, a bone graft may be used to fill and rebuild the affected area. However, this option isn’t suitable for everyone and is determined on a case-by-case basis, depending on the extent and location of the damage. - Growth Factors and Matrix Proteins
These are natural biological substances found in the body that can be applied during treatment to promote tissue healing and regeneration.
How to Stop and Prevent Further Bone Loss
The best way to deal with jawbone loss is to fix the real culprits as early as possible.Why is acting early so important? The longer you wait, the more severe the bone loss becomes. And the more bone you lose, the more complex and costly the treatment will be.
Whether bone loss is caused by missing teeth or gum disease, it won’t stop on its own if the underlying issues aren’t addressed.
So, the best course of action is to act fast before the situation requires more advanced, costly, and invasive procedures.
Here are some tips:
- Replace Missing Teeth as Soon as Possible: After a tooth extraction, a dental implant can usually be placed after about four months of healing. Don’t delay — bone loss occurs rapidly in the first six months. If there isn’t enough bone to support the implant, a bone graft may be needed, which adds to the treatment time and cost.
- Socket Preservation: This procedure is performed at the same time as the tooth extraction. The empty socket is immediately filled with bone graft material, helping to preserve bone volume and prevent the jawbone from collapsing during healing (see image below).
- Treat Gum Disease: Once gum disease reaches the bone and deeper supporting tissues, it cannot be cured at home. Professional deep dental cleaning, along with good oral hygiene at home, is the only way to stop further bone loss.
- Lifestyle Changes: Any habits that contribute to bone loss should be tackled. These include smoking, teeth grinding (bruxism), chronic stress, and a poor diet. Stopping these habits will benefit not only your teeth and gums but also your overall health.
- Aging and bone loss: new insights for the clinician https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3383520/
- Trends in osteoporosis prevalence among adults aged 50 and over from 2007–2008 through 2017–2018 differed by sex. https://www.cdc.gov/nchs/products/databriefs/db405
- Gum Disease https://www.cdc.gov/oralhealth/fast-facts/gum-disease/index.html
- The use of autogeneous mandibular bone block grafts for reconstruction of alveolar defects https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4555953/
- Maxillary vertical alveolar ridge augmentation using sandwich osteotomy technique with simultaneous versus delayed implant placement: A proof of principle randomized clinical trial https://pubmed.ncbi.nlm.nih.gov/36239176/
- Onlay grafts http://www.dr-beaupere-chirurgien-dentiste.fr/en/inlay-onlay-graft.php