The Different Healing Stages of a Dental Bone Graft
 If you’ve lost too much bone, a dental bone graft can help restore it and make many treatments possible, especially dental implants.
If you’ve lost too much bone, a dental bone graft can help restore it and make many treatments possible, especially dental implants.
After getting a bone graft, you might be wondering about the healing process. How long does it take for the graft to fully integrate with your jawbone? And what stages does it go through to get there?
Don’t worry—we’ll walk you through each healing stage step by step. We’ll also go over possible complications, so you’ll know what’s normal and when something might be wrong.
Table of content
What is a Dental Bone Graft?
Dental bone grafting is a common procedure with a high success rate. It usually involves adding bone or synthetic material to your jawbone to rebuild lost volume.Why might you need this procedure? The most common reason is to prepare your jaw for a dental implant.
If your jawbone is too weak or has lost too much volume, it cannot support an implant properly. In this case, a bone graft may be needed first.
Other times, a bone graft may save a natural tooth that has lost too much bone due to gum disease.
There are different types of graft materials your dentist might use, including:

Autogenous Graft: This type uses bone taken from your own body, usually from your lower jaw.
It has several benefits—it contains living cells that help grow new bone, and there’s no risk of rejection (it’s your own tissue).
The downside? It requires a second surgical site to collect the bone.
Allogenic Graft: This graft comes from a human donor, often a cadaver. The bone is treated and processed to remove any living cells and ensure it’s completely clean and safe. It’s readily available from bone tissue banks and doesn’t require a second surgery.
Xenogeneic Graft: Similar to an allogenic graft, but the source is an animal species, usually cows (bovine).
Synthetic Material: These are artificial biomaterials designed to do the same job as real bone. They’re also called bone substitutes.
The Healing Stages of Dental Bone Graft
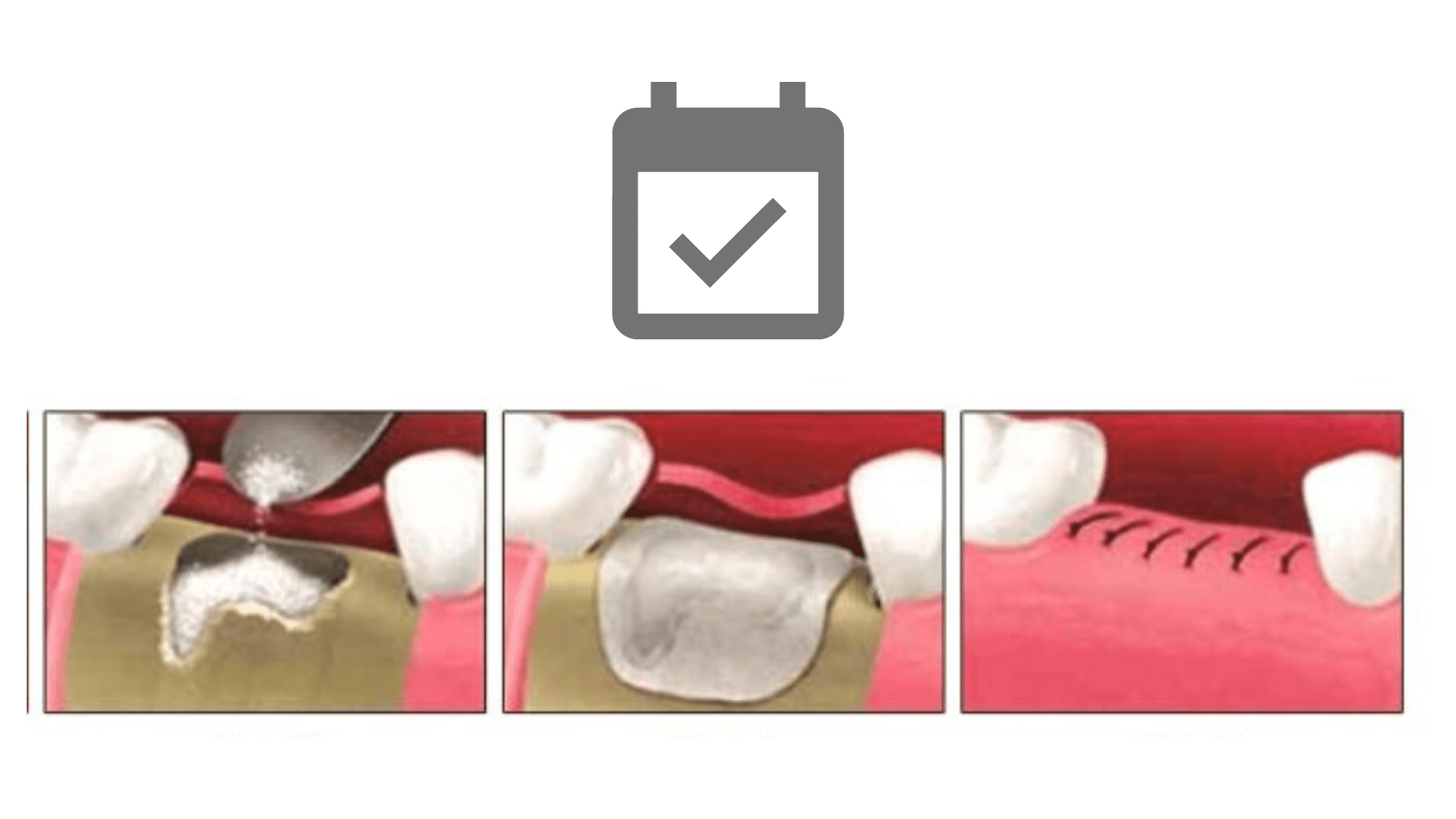
Before placing the bone graft, your dentist first needs to cut the gums to expose the bone underneath.The gums usually heal quickly, often within the first two weeks. But the bone graft takes much longer to fully heal.
One important thing to know is that the graft material isn’t living tissue, so it doesn’t actually “fuse” with your jawbone by itself. Instead, your body gradually breaks it down and replaces it with new, fresh bone.
Think of a bone graft like a foundation or scaffold. It’s similar to how a support stick helps a young plant grow straight. The graft provides a base for new cells and blood vessels to grow, so your body can gradually replace it with real, living bone.
Here are the different healing stages of a dental bone graft:
1. Inflammation Phase: The First 4 Days
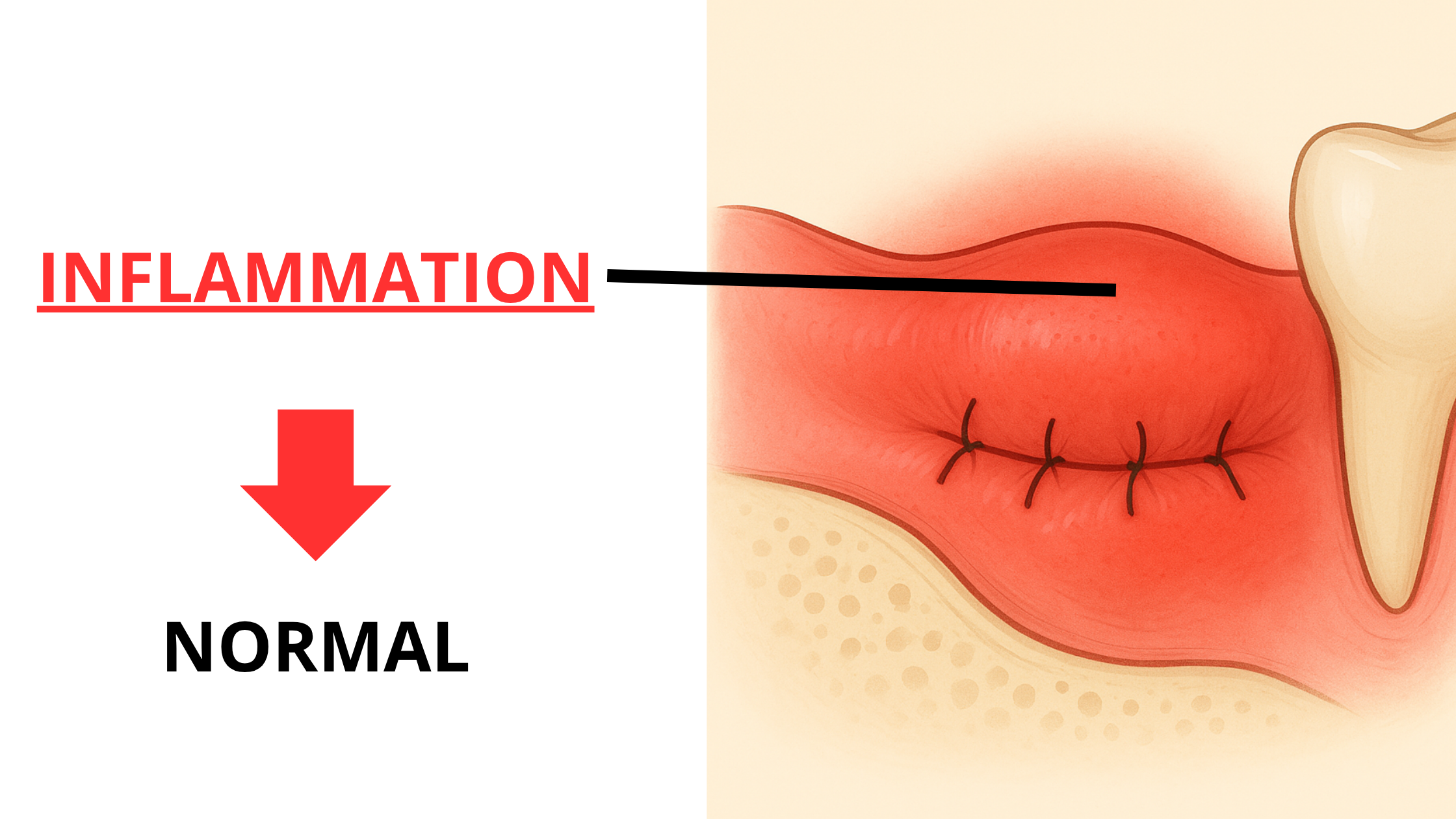
Right after the procedure, your body triggers an inflammatory response to start the healing process. This stage usually lasts up to four days.
During this phase, your blood vessels expand to bring in immune cells and nutrients. Their job is to clean the area and prepare it for the next steps.
You may notice redness, swelling, and some discomfort around the surgical site. Don’t worry, these are completely normal and temporary.
A blood clot also forms between the graft and the jawbone right after the procedure. This clot helps stop the bleeding and holds the graft in place. It’s also rich in growth factors that attract new cells and promote the formation of blood vessels.
At this stage, it’s very important to avoid putting pressure on the area. This can damage the blood clot, which can lead to bleeding. It can also cause the graft to loosen and prevent it from settling properly.
2. New Blood Vessels: Next 4 Weeks
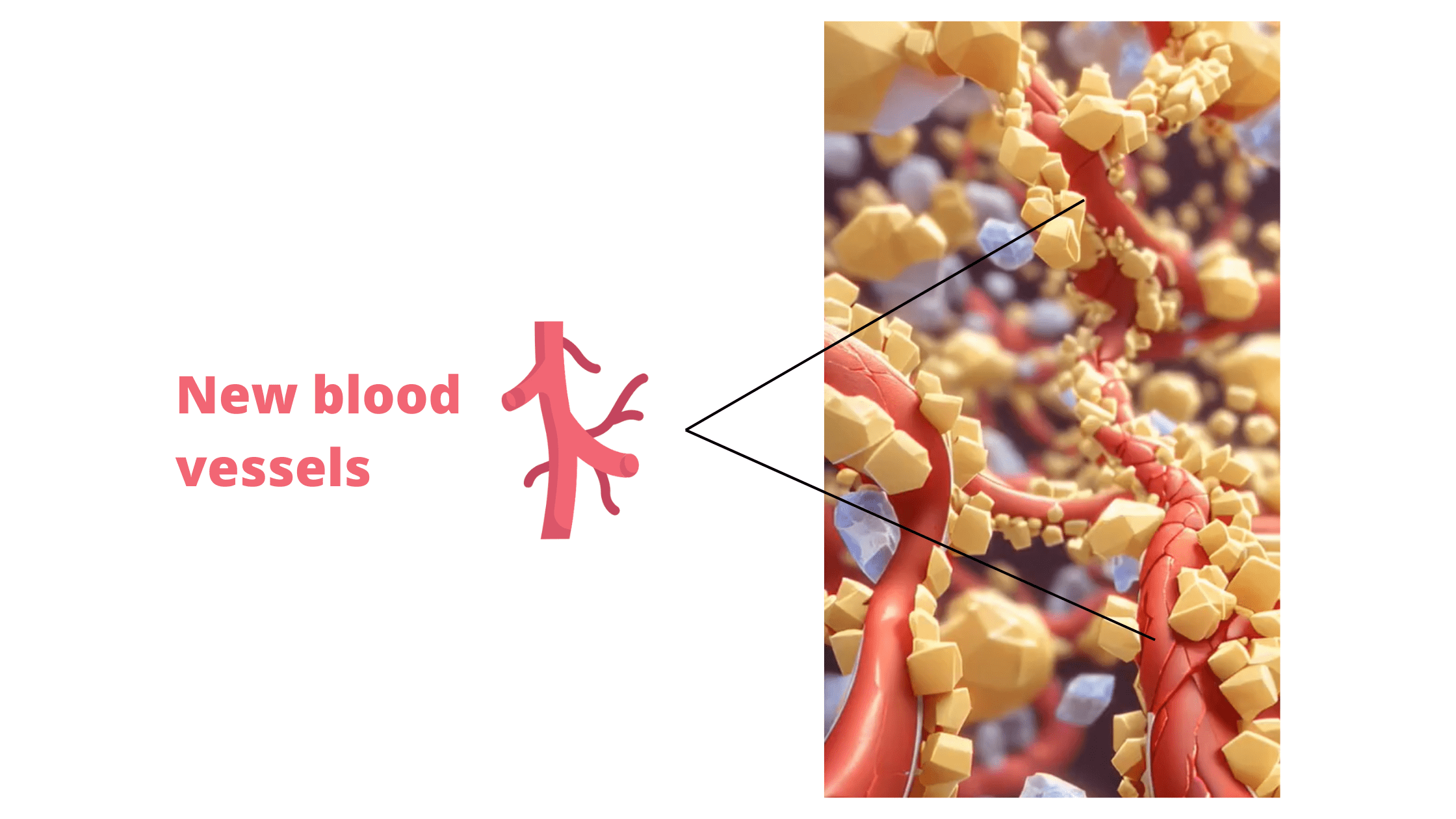
As the inflammation starts to fade (usually around day 4), tiny blood vessels begin to grow around and into the graft. This process continues over the next few weeks.
These new blood vessels bring in the cells and nutrients your body needs to start building new bone.
New bone formation typically begins around weeks 3 to 4, when the graft starts to fuse and take hold.
How quickly blood vessels form depends on the type of graft material used. If the graft is porous (like a sponge with tiny openings), blood vessels can grow into it more easily and quickly.
But if the graft is dense and compact, like cortical bone, the process takes longer since it’s harder for vessels to grow through it.
3. Bone Resorption and Formation Cycle
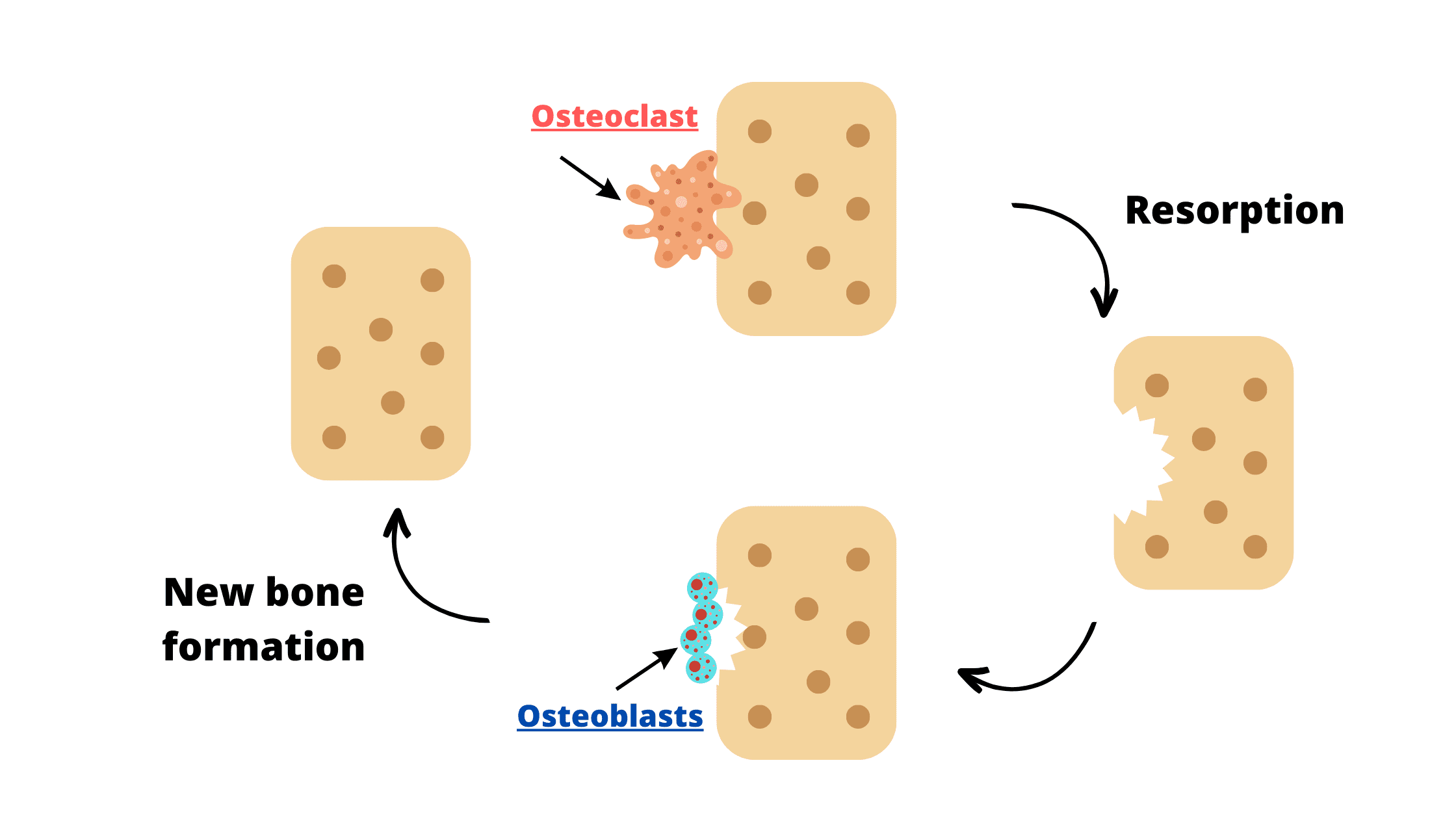
This is the slowest phase of healing and can take several months, or even years.
Once blood vessels have grown into the graft, the healing process follows this cycle:
- Bone resorption by osteoclasts: These cells begin to break down the graft material, creating space for new bone to grow.
- Bone formation by osteoblasts: The spaces left by osteoclasts are then filled in with new bone by another type of cell called osteoblasts.
The cycle of resorption and formation is part of the natural bone remodeling process. It will continue over time until the graft is replaced, either partially or completely, by your body’s own living bone.
How Long Does the Healing Process Take?
Your soft tissues (the gums) usually heal quickly. In most cases, stitches can be removed safely after the first week. But if you have resorbable (dissolvable) sutures, there's no need—they’ll disappear on their own.It takes a bit longer for the bone graft to fully integrate and fuse with your jawbone—usually around 4 to 6 months, and sometimes even longer.
The goal is to wait until your jaw is strong and stable enough to support the next step, such as placing implants.
But, healing time can vary from person to person. Factors like your age, general health, and the type of graft used can all affect how fast you heal.
Potential Complications
During the first four days, especially in the inflammation phase, you might experience some swelling, pain, and difficulty opening your mouth. Don't fret; these are normal and actually part of the healing process.But, like with any surgery, there's always a slight risk of complications, although they're quite rare. Here are some things to watch for:
- Infection: Sometimes, bacteria can enter the site and cause an infection, especially if oral hygiene instructions are not followed properly. This can affect both the donor and recipient sites. Warning signs include severe pain, pus coming out of the area, bad breath or a foul taste, and swelling that gets worse.
- Rejection: This is a small risk and occurs when your body doesn't recognize and accept the graft. As a result, blood vessels won't form over the graft, and it won't survive, breaking down quickly. This is more common with allogenic grafts, where the graft comes from another person.
- Bone particles coming out: That's common and doesn’t mean the graft is failing. However, if you notice larger pieces or excessive loss along with signs of infection, don’t delay seeing your dentist.
- Hematoma and bruising: This happens when blood leaks beneath the skin and surrounding tissue, causing bluish discolorations. It’s temporary and harmless, and usually goes away on its own within 5 to 10 days. But if it lasts longer or comes with other symptoms, talk to your dentist..
Factors That Affect Bone Grafting Success
Several factors can have an impact on the speed and effectiveness of bone graft healing. These include:- Oral Hygiene: Maintaining excellent oral hygiene after the procedure is crucial. It helps prevent infections that can impair the success of the bone graft. Your dentist will give you specific instructions, like using antiseptic mouthwash, salt water rinses, and an extra soft toothbrush for the first few weeks. Be sure to follow these exactly.
- Smoking: Tobacco and its by-products contain harmful chemicals that slow down healing. Smoking narrows blood vessels, which reduces the flow of nutrients and healing cells to the area.
Many studies show that smoking increases the risk of bone graft failure and can lead to poorer results. So, try to avoid smoking for at least the first two weeks after your procedure. - Overall Health: Certain medical conditions can weaken your immune system or affect blood flow, which can slow down healing. One common example is diabetes. It can impact blood circulation, weaken your immune response, delay wound healing, and raise the risk of infection.
- Medications: Some medications, like long-term corticosteroid therapy and immunosuppressants, can lower your immune response, which increases the risk of infections. It’s important to discuss all your medications with your dentist before the procedure so the necessary precautions can be taken.
Optimize Healing and Minimize Complications
While side effects from the procedure are temporary and usually go away on their own, there are steps you can take to support your recovery and reduce discomfort. Here are some helpful aftercare tips:- Change your dressing regularly at home, using fresh gauze pads for your gums. If you experience bleeding, apply gentle pressure to the surgical site for a few minutes. If bleeding persists excessively, reach out to your dentist.
- Follow all the medications as directed by your dentist, including pain relievers, mouthwashes, and antibiotics if prescribed.
- Stick to a soft and warm diet, avoiding hot, hard, and crunchy foods during the first week.
- Don't brush the surgical site during the initial week. Afterward, use a soft toothbrush with gentle motions to clean the area.
- Starting the day after surgery, rinse your mouth gently with the prescribed antiseptic mouthwash or warm salt water until fully healed. Avoid spitting forcefully during the first two days to protect the blood clot.
- Avoid strenuous activities or exercices that could disrupt the graft during the initial week.
- Apply ice to the surgical site for 10 minutes every 20 minutes during the first 24 hours. This will help reduce swelling and discomfort in the next days. After the first 24 hours, switch to warm compresses.
- Keep your follow-up visits with your dentist to monitor healing.
- Bone grafts in dentistry - PMC (nih.gov)
- Biological principles of bone graft healing - ScienceDirect
- La cicatrisation des greffes osseuses - ScienceDirect
- The effect of cigarette smoking on dental implants and related surgery - PubMed (nih.gov)
- The Etiology and Management of Dental Implant Failure: A Review - PMC (nih.gov)