Can You Actually Reverse Tooth Decay? (5 Key Steps to Follow)
 If you have tooth decay and are wondering if it can be reversed, the short answer is yes. However, as you may have heard, tooth decay is not always treatable at home.
If you have tooth decay and are wondering if it can be reversed, the short answer is yes. However, as you may have heard, tooth decay is not always treatable at home.
When the damage is limited to the surface level of your teeth, you can take steps to restore and heal them effectively from home.
Once tooth decay has progressed deeper and created a hole, a professional treatment by your dentist is required.
Keep reading to discover the 5 essential proven steps to reverse tooth decay before it's too late.
This article may contain affiliate links, which means I may earn a small commission at no additional cost to you if you make a purchase through these links. I only recommend products and services that I believe will add value to my readers. Thank you for supporting my blog!
In this article:
1. The Right Steps to Reverse Tooth Decay Effectively at Home
2. How Does Tooth Decay Start and Develop?
3. When is Tooth Decay No Longer Reversible?
4. Other Causes of Tooth Decay
The Right Steps to Reverse Tooth Decay Effectively at Home
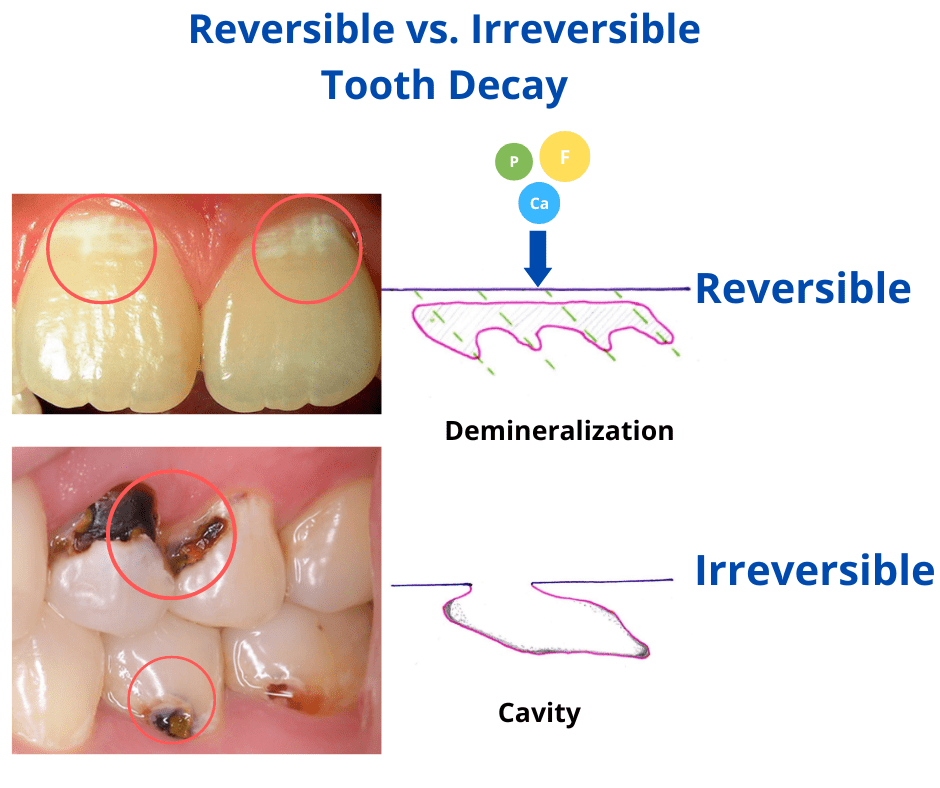
If you're dealing with early-stage tooth decay, there are steps you can take to reverse the damage and prevent it from getting worse.Early decay often shows up as white or brown spots on the tooth surface and hasn’t yet developed into a cavity. But if a deep hole has already formed, it’s crucial to see your dentist because this level of damage can no longer be reversed at home.
Here are the most effective, clinically proven methods to stop or even reverse early tooth decay:
- Perfect your oral hygiene
- Consider fluoride
- Remineralizing treatments
- Support your saliva
- Maintain a healthy diet
1. Oral Hygiene

Why is oral hygiene so important? Because it helps eliminate plaque—the main cause of tooth decay. Plaque is a soft, sticky film filled with bacteria that builds up constantly on your teeth. If left unchecked, it can thicken and not only damage your teeth but also block minerals from reaching and repairing them.
Removing plaque and keeping it under control should be your top priority when fighting tooth decay. Here’s how:
- Brush your teeth twice a day for 2 minutes with the right technique: It's not just about brushing—it's about brushing properly. Use a soft-bristled toothbrush and move it gently in small, circular motions for about 2 minutes. Avoid brushing too hard or using horizontal strokes, as these can wear down your enamel. Think of it as massaging your teeth and gums, not scrubbing them.
- Switch to an electric toothbrush: Research shows that electric toothbrushes are more effective at removing plaque than manual ones. Plus, they take the guesswork out of the brushing technique, as the toothbrush does most of the work for you—all you need to do is guide it over your teeth and gums.
- Wait 30 minutes after eating sugary or acidic foods before brushing: After consuming sugary or acidic items, your teeth are more vulnerable to losing minerals. Brushing immediately can make this worse. Waiting for about 30 minutes gives your saliva time to neutralize the acidity and protect your teeth.
- Clean between your teeth: These areas are tricky to reach with a regular toothbrush and make up around 40% of your tooth surfaces. If you skip them, almost half of your teeth remain coated in plaque and trapped food particles! Use dental floss, an interdental brush, or a water flosser—whichever you prefer—and aim to do this once a day, ideally before bed.
2. Consider Fluoride

Fluoride has long been a powerful weapon against cavities and an effective way to reverse early tooth decay. Here’s how it helps:
- When you get fluoride from water, food, or oral care products, some of it binds to your enamel, replacing lost minerals and making it stronger against acid attacks.
- Fluoride also has antibacterial properties that target the harmful bacteria causing cavities. It even stops these bacteria from sticking to your teeth, reducing plaque buildup and promoting healthier teeth and gums.
There are two main ways to get fluoride:
- Collective Sources: Depending on where you live, fluoride may be added to tap water, salt, or even flour. For example, in the U.S., about 74% of people served by community water systems receive fluoridated water.
- Personal Use: This involves using fluoridated oral hygiene products such as toothpaste, dental gels, or mouthwash.
The Best Fluoride Toothpaste to Reverse Tooth Decay
Most toothpastes on the market contain fluoride, but if you're looking to reverse tooth decay, there are two important factors to keep in mind:
- Look for a seal of acceptance (such as from the ADA or a trusted dental organization).
- Choose a non-abrasive formula that is gentle on your enamel to avoid causing further damage. Some great options include ProNamel by Sensodyne and Arm & Hammer Peroxicare Toothpaste.
The safest fluoride concentration in OTC toothpastes is between 1,000–1,500 ppm. Using higher concentrations can pose risks to both your teeth and your overall health.
3. Fluoride Alternatives and Supplements
Recently, several alternatives to fluoride have emerged to help repair teeth and reverse early damage, without the potential side effects of fluoride.
These products typically focus on replenishing your teeth with the minerals they are naturally made of: calcium and phosphorus.
The best part? Your body and teeth are already familiar with these minerals, so there's no risk of toxicity.
One of the most well-known alternatives is nano-hydroxyapatite (n-HA), which is the natural building block of our teeth. It’s commonly used as an active ingredient in fluoride-free toothpaste brands like Boka and RiseWell.
Besides your regular toothpaste, you can add another product to your routine for extra remineralization, like a dental gel, cream, or mouthwash.
-
Dental Gel: Some great fluoride-free options include CariFree Fluoride-Free Gel (with n-HA) and R.O.C.S. Remineralizing Gel (with calcium, phosphorus, and magnesium).
To use, apply a thin layer of gel to your teeth with a toothbrush and leave it on for 1-2 minutes. Spit out the excess but don't rinse, drink, or eat for at least 30 minutes. It's best to do this once a day, preferably before bedtime. - Biomin Calcium: Biomin is made of tiny mineral particles that slowly dissolve in saliva to form hydroxyapatite, which coats and remineralizes the teeth. One fluoride-free toothpaste containing Biomin in its formula is Dr. Collins Biomin Restore.
- CCP-ACP (Recaldent): This remineralizing ingredient is found in products like Recaldent Chewing Gum, GC Tooth Mousse, and MI Paste Cream.
4. Support Your Saliva

Think of saliva as your mouth's natural cleanser—it helps wash away food particles and balance the acidity in your mouth.
Saliva also acts as a mineral carrier, delivering minerals to your teeth. Without a healthy flow of saliva, other remineralization treatments won’t work effectively.
Here are some tips to boost your saliva:
- Avoid Snacking Between Meals: Saliva does its best work between meals. By avoiding frequent snacking, you give your saliva a chance to clean and regenerate your teeth naturally.
- Consider Xylitol: Xylitol is a sugar substitute that not only stimulates saliva production but also helps fight cavity-causing bacteria and reduces the acid attacks. Chewing sugar-free gum with xylitol between meals is a great way to boost saliva and reduce plaque buildup.
- Stay Hydrated: A dry mouth increases the risk of cavities. Staying hydrated throughout the day helps keep your mouth moist, reduces acidity spikes, and prevents bacteria from accumulating and forming plaque.
5. Mind Your Diet

One study found that improving diet by reducing sugary cereals and increasing calcium and vitamin D intake significantly lowered the risk of tooth decay in children.
Alongside your oral hygiene routine, paying attention to your eating habits is just as important. What you eat and drink has a direct impact on the health of your teeth and mouth.
Here are some tips:
- Reduce sugar intake: Lower acidity and reduce cavity-causing bacteria. This also helps your teeth regain essential minerals.
- Aim for a balanced diet: Focus on a natural and varied diet that meets your daily needs for both micro and macronutrients. Avoid refined sugars and processed foods—they harm not only your teeth but also your overall health.
- Probiotic foods: Include yogurt, kefir, and sauerkraut in your meals. These foods help boost friendly bacteria and balance the microbiome in both your mouth and gut.
- Consider the last food you eat: The last food you eat at a meal affects your mouth’s acidity for the next minutes. Try to finish your meals with tooth-friendly foods that aren’t sweet, acidic, or sticky—like dairy products, vegetables, or whole grains.
How Does Tooth Decay Start and Develop?
Tooth decay happens when many factors work together to slowly damage the hard parts of your teeth—enamel and dentin.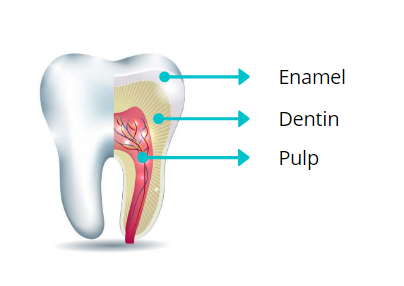
Natural teeth are made of three layers:
- Enamel: The outermost, hard, mineral-packed layer.
- Dentin: The layer beneath the enamel, also mineral-rich.
- Pulp: The soft center containing nerves and blood vessels.
The acids in your mouth are mainly produced by cavity-causing bacteria.
Your mouth’s acidity level isn’t constant—it goes up and down throughout the day.
When acidity is high, your teeth lose minerals in a process called demineralization.
When the acidity drops back to normal, your teeth can regain some of those minerals through remineralization.
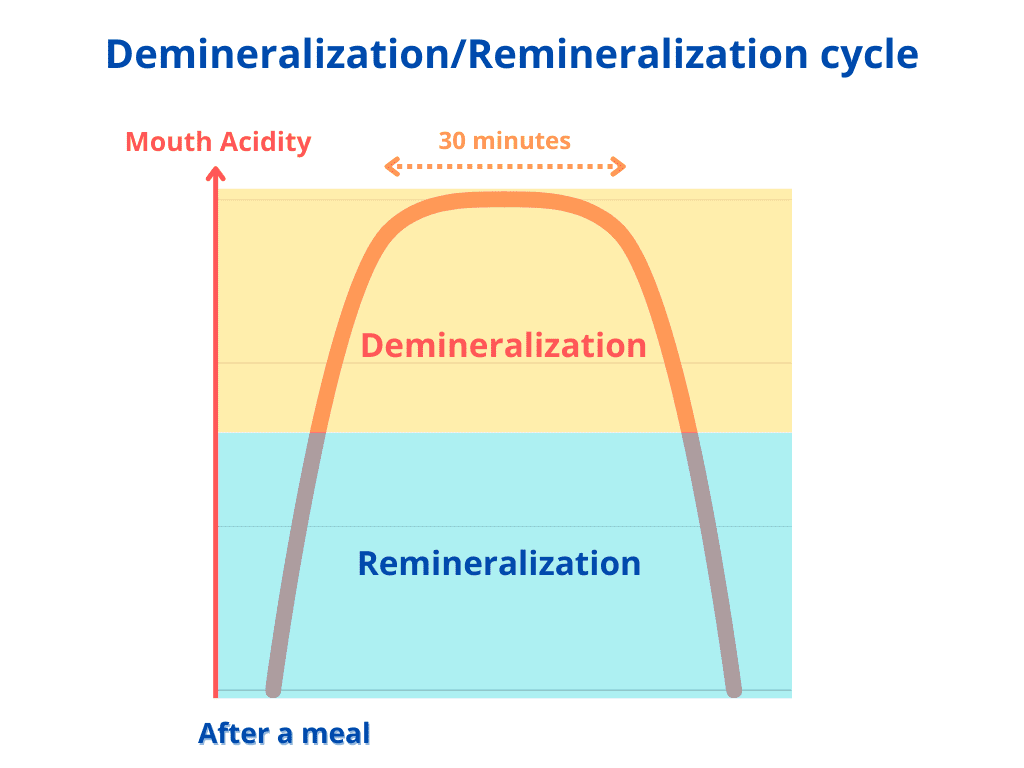
In healthy individuals, this demineralization–remineralization cycle works well and keeps the teeth safe from damage. Here’s how it works:
- After eating or drinking something sweet or acidic, the acidity in your mouth rises. This causes demineralization, where the enamel temporarily loses minerals.
- About 30 minutes later, as the acidity naturally decreases, remineralization kicks in. Lost minerals are restored to the enamel with help from saliva, fluoride toothpaste, water, and mineral-rich foods like tea, fish, dairy products, and vegetables.
Cavities form when this cycle becomes unbalanced.
If your teeth are exposed to acid too often—due to frequent snacking, sugary foods, dry mouth, or slow saliva flow—demineralization lasts longer, and remineralization doesn’t have enough time to repair the damage. Over time, this leads to the breakdown of enamel and the formation of cavities.
When is Tooth Decay No Longer Reversible?
As long as the decay is limited to the tooth's surface, there’s still a chance to restore lost minerals and heal your teeth naturally.To check whether a cavity is still in its early, reversible stage, dry your teeth and look at them in the mirror.
- Early decay often shows up as white or brown chalky spots—these are signs of demineralization.
- At this stage, you shouldn’t feel any pain, because the damage is limited to the enamel, which doesn’t have nerves.
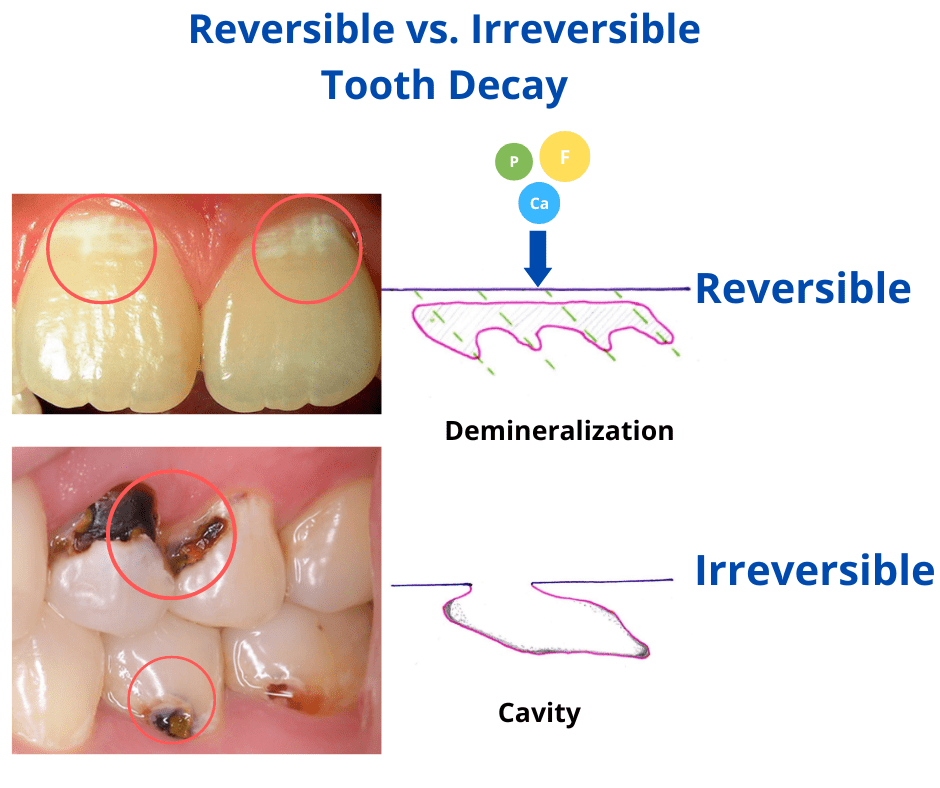
At this early stage, the damage is superficial and responds well to home treatments such as fluoride or remineralizing products.
However, if you notice a visible cavity or deep hole, the decay has progressed and is no longer reversible.
At this point, bacteria have reached deeper layers of the tooth and are continuing to damage it from the inside.
Home remedies won’t be enough to stop it, so professional dental treatment is necessary.
Other Causes of Tooth Decay
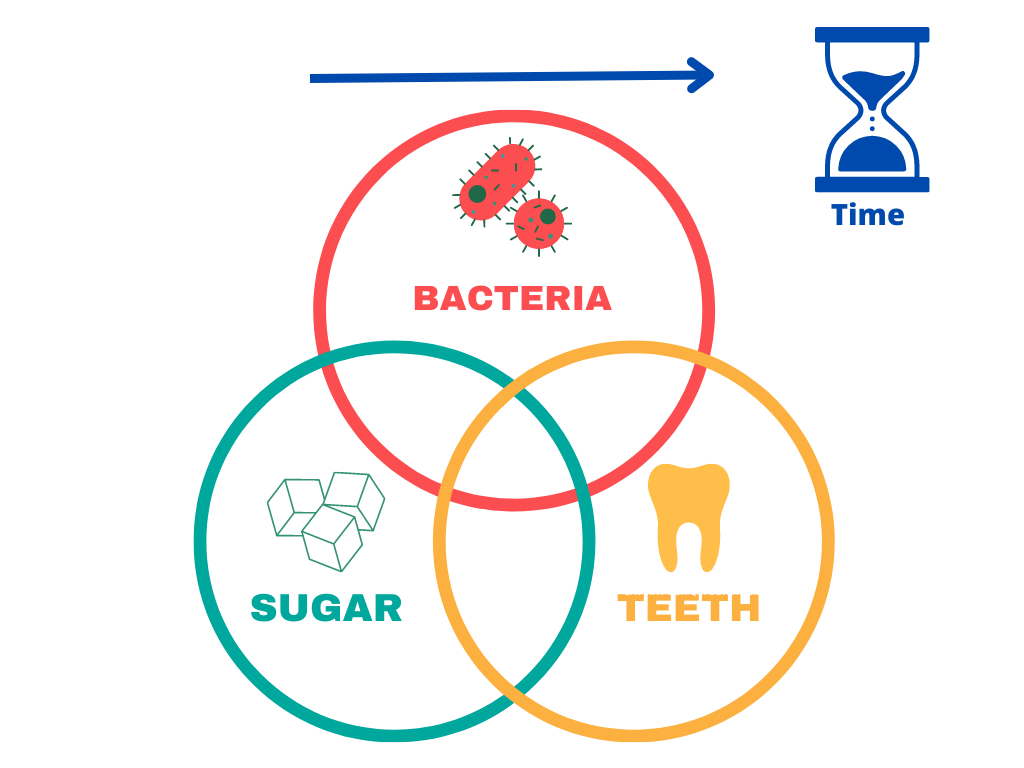
It’s easy to think that cavities are only caused by poor oral hygiene—but the truth is more complex.
Some people hardly ever brush and still don’t get cavities, while others seem to do everything right and still struggle with tooth decay.
In reality, cavities result from a mix of factors working together over time. Here are some of the most important ones:
- Diet – A diet high in carbohydrates and low in essential vitamins and minerals weakens your teeth and makes them more vulnerable to decay.
- Saliva – When saliva flow is reduced—due to medications, health conditions, or smoking—the risk of decay increases.
- Oral hygiene – Without proper oral hygiene, plaque builds up, raising the risk of cavities.
- Enamel defects – Some people have weaker teeth due to genetic or developmental enamel defects. These teeth are more prone to decay and often require special care to avoid damage.
Other factors that influence cavity risk include:
- The types of bacteria present in your mouth
- The composition and flow of your saliva
- Your genetics
- Your immune system
- The alignment of your teeth—whether they are straight or crowded
- Is there evidence for Novamin application in remineralization?: A Systematic review https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7068624
- [Casein phosphopeptide--amorphous calcium phosphate (CPP-ACP) and its effect on dental hard tissues] https://pubmed.ncbi.nlm.nih.gov/19306597/
- Treatment of orthodontic white spot lesions with a remineralizing dentifrice applied by toothbrushing or mouth trays. https://europepmc.org/article/med/10686860
- Remarks on THE INFLUENCE OF A CEREAL-FREE DIET RICH IN VITAMIN D AND CALCIUM ON DENTAL CARIES IN CHILDREN https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2520490/