The different healing stages after a tooth extraction (with pictures)
 Tooth extraction is the most routine procedure, although it's the last resort when a tooth can no longer be kept in the mouth.
Tooth extraction is the most routine procedure, although it's the last resort when a tooth can no longer be kept in the mouth.
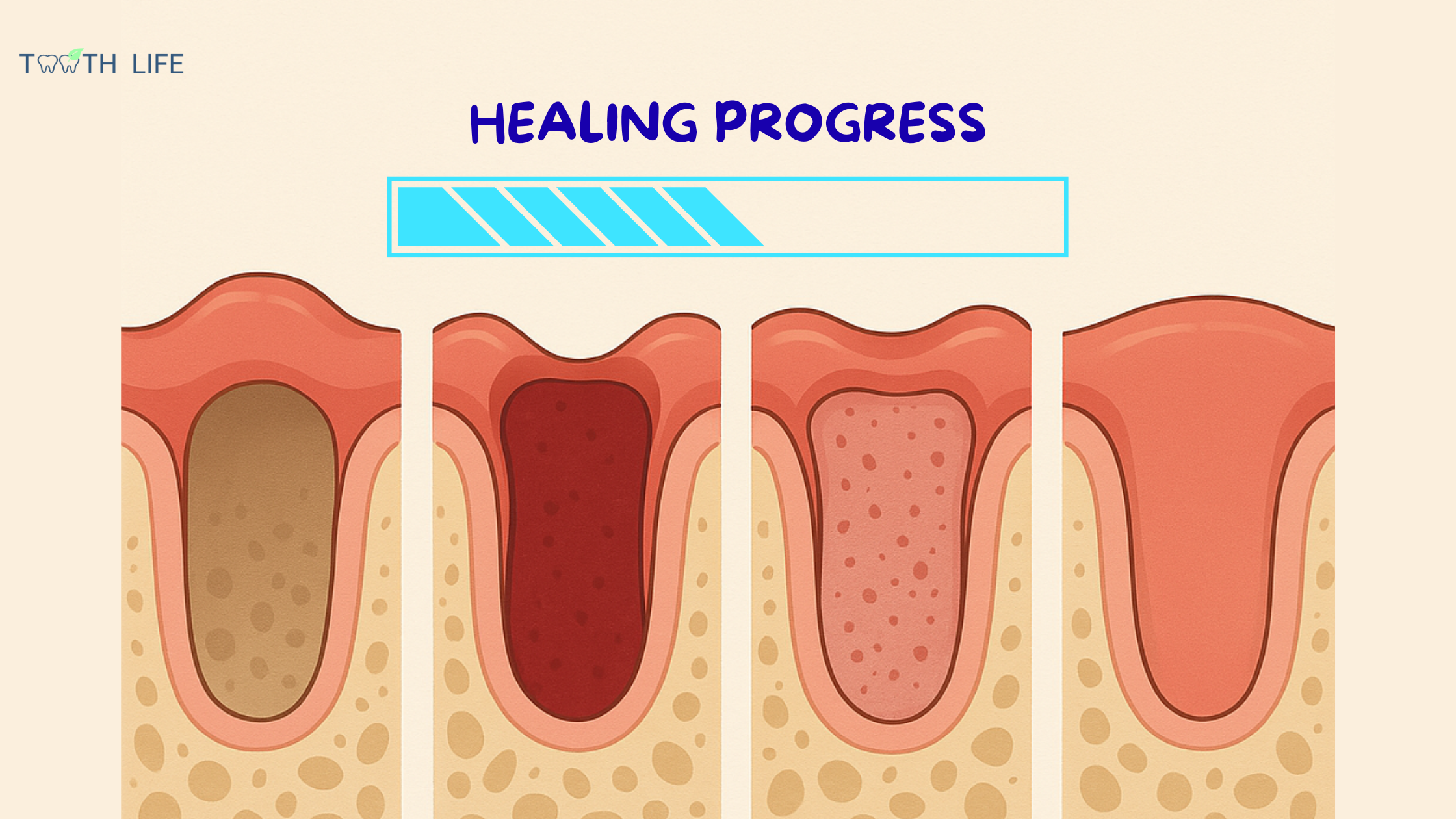
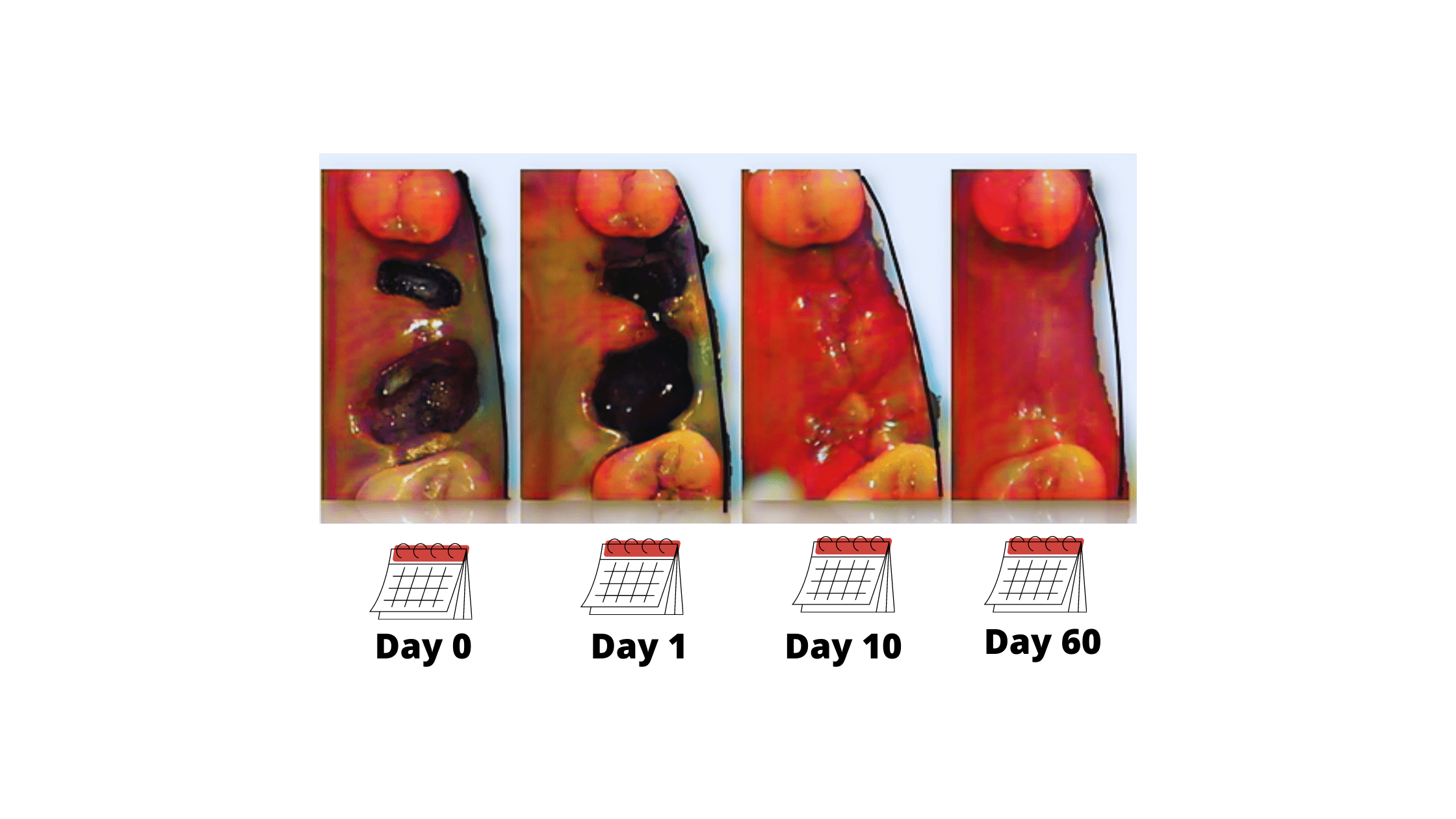
After extraction, the healing process goes through several stages that can take several weeks or even months. The goal is to close the wound and fill the empty socket with new bone.
Some initial side effects are completely normal. Understanding the different healing stages can help you manage them better and ensure a smooth recovery.
In this article, we will go over the different healing stages after a tooth extraction and give you tips on how to care for your mouth during each step.
In this article...
The different healing stages after a tooth extraction:
1. Day 1-3: Blood clot formation and inflammation
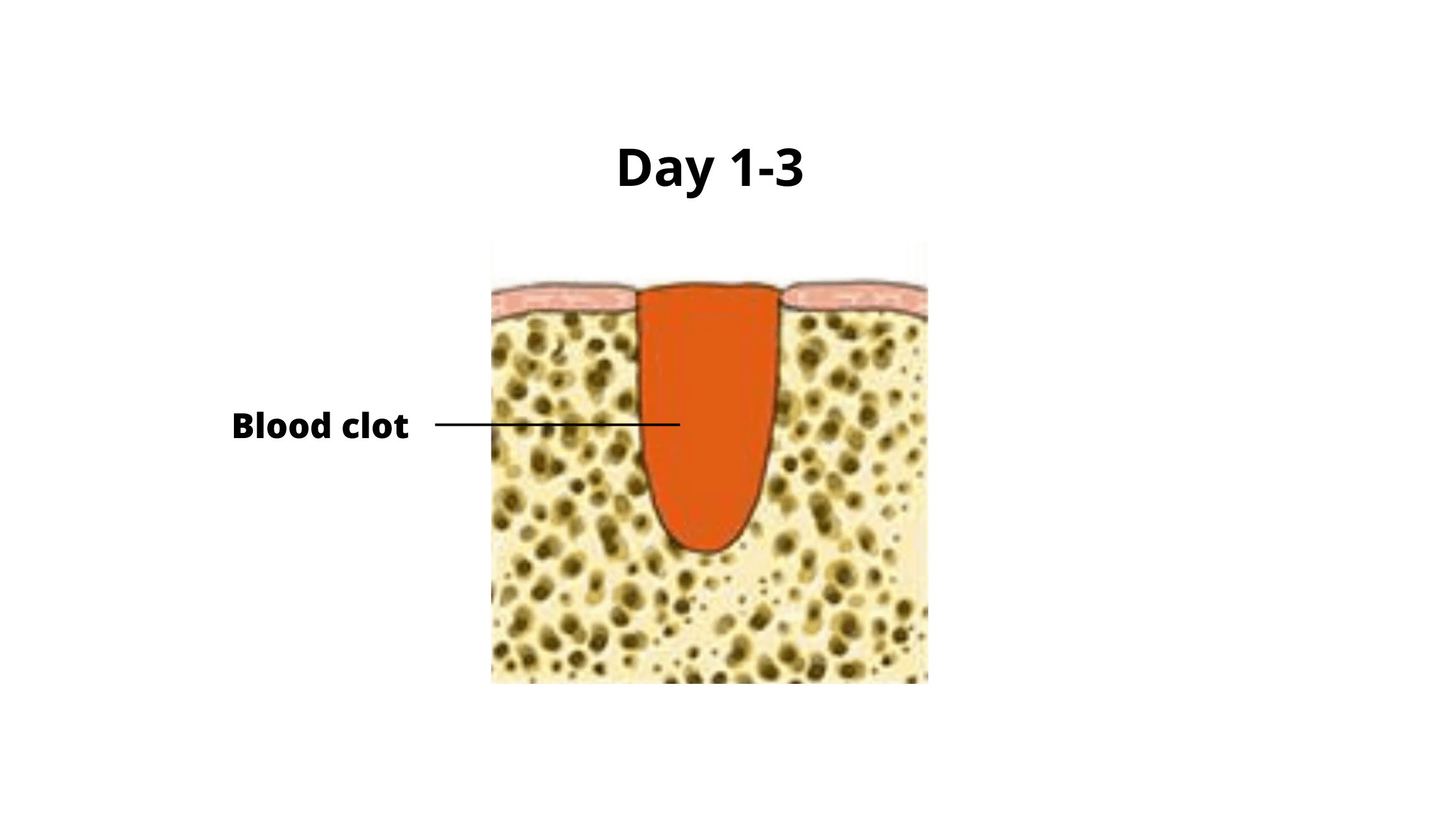 Immediately after the procedure, a blood clot begins to form.
Immediately after the procedure, a blood clot begins to form.
This clot is a reddish, jelly-like mass that fills and protects the socket. It not only stops the bleeding but also contains living cells, proteins, and growth factors that kickstart the healing process.
At the same time, your body triggers an inflammation to clean the wound. This reaction peaks during the first 24 hours. So, it’s completely normal to experience pain, swelling, and redness around the first three days.
These early side effects are temporary and should gradually improve over the first week.
Some tips for this phase:
1. Protect the blood clot:
- Don’t smoke
- Don’t drink alcohol
- Don’t rinse your mouth, spit, or use a straw on the first day
- Don’t brush or floss near the extraction site
- Avoid hot food and drinks
- Avoid intense physical activity
2. Manage the pain and swelling:
- For the first 24 hours, apply an ice pack to the affected area for 10 to 15 minutes at a time, several times a day.
- Take pain medication as directed by your dentist.
- From the second day on, rinse with salt water (one teaspoon of salt in a glass of warm water).
3. Manage bleeding:
- Prepare a small piece of sterile gauze and place it directly on the extraction site,
- Bite on it and hold the pressure for at least 30 minutes,
- Don't suck on the wound or run your tongue over the extraction site.
2. Day 4-5: Granulation tissue formation
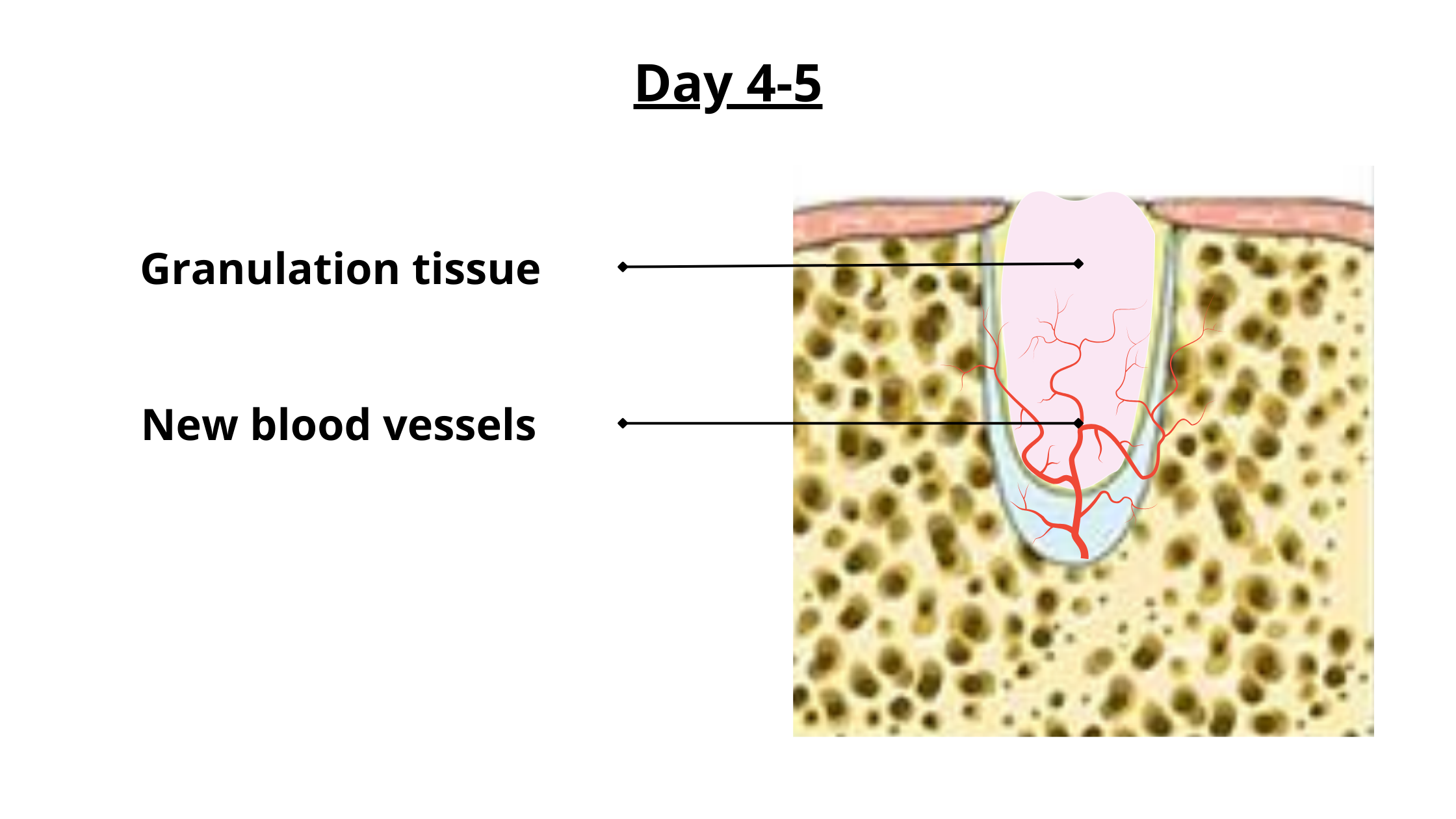 At this stage, the blood clot gradually changes to a pale pink or whitish color and turns into granulation tissue. This tissue is tougher and more stable, held firmly in place by new blood vessels that grow through it.
At this stage, the blood clot gradually changes to a pale pink or whitish color and turns into granulation tissue. This tissue is tougher and more stable, held firmly in place by new blood vessels that grow through it.
Granulation tissue acts as a scaffold, allowing new cells to move into the area and begin rebuilding the bone and closing the wound.
You may still feel some pain during meals or at night, but it should be less intense as the inflammation continues to fade.
What to do at this stage?
- Continue to take medications as prescribed by your dentist.
- Continue to rinse your mouth with salt water or a mouthwash as directed.
- Stick to a soft diet for now. You'll soon be able to return to your regular solid diet as healing progresses.
- Brush and floss gently to avoid food build-up and a potential infection.
- If you experience any unusual symptoms or complications, such as severe pain, fever, or excessive bleeding, contact your dentist or surgeon right away.
3. Week 1-2: Early bone formation
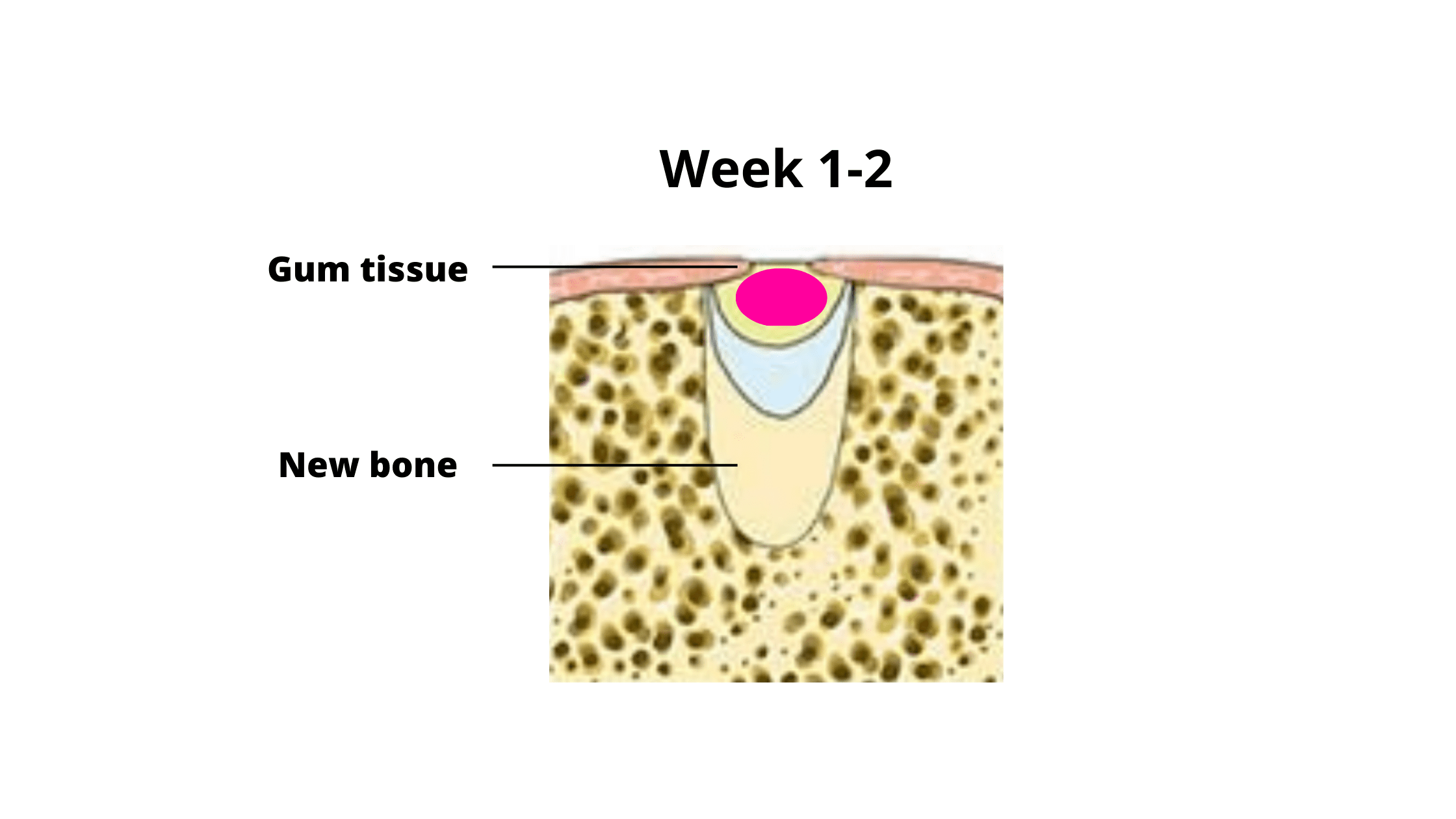 By this stage, most of the swelling, pain, and discomfort should have gone away.
By this stage, most of the swelling, pain, and discomfort should have gone away.
The gum tissue is fully healed and covers the wound. The empty socket left by the extracted tooth begins to fill with new bone. This new bone is still immature at first, but it will continue to strengthen over the next few weeks.
4. Week 4-16: Complete bone formation and maturation
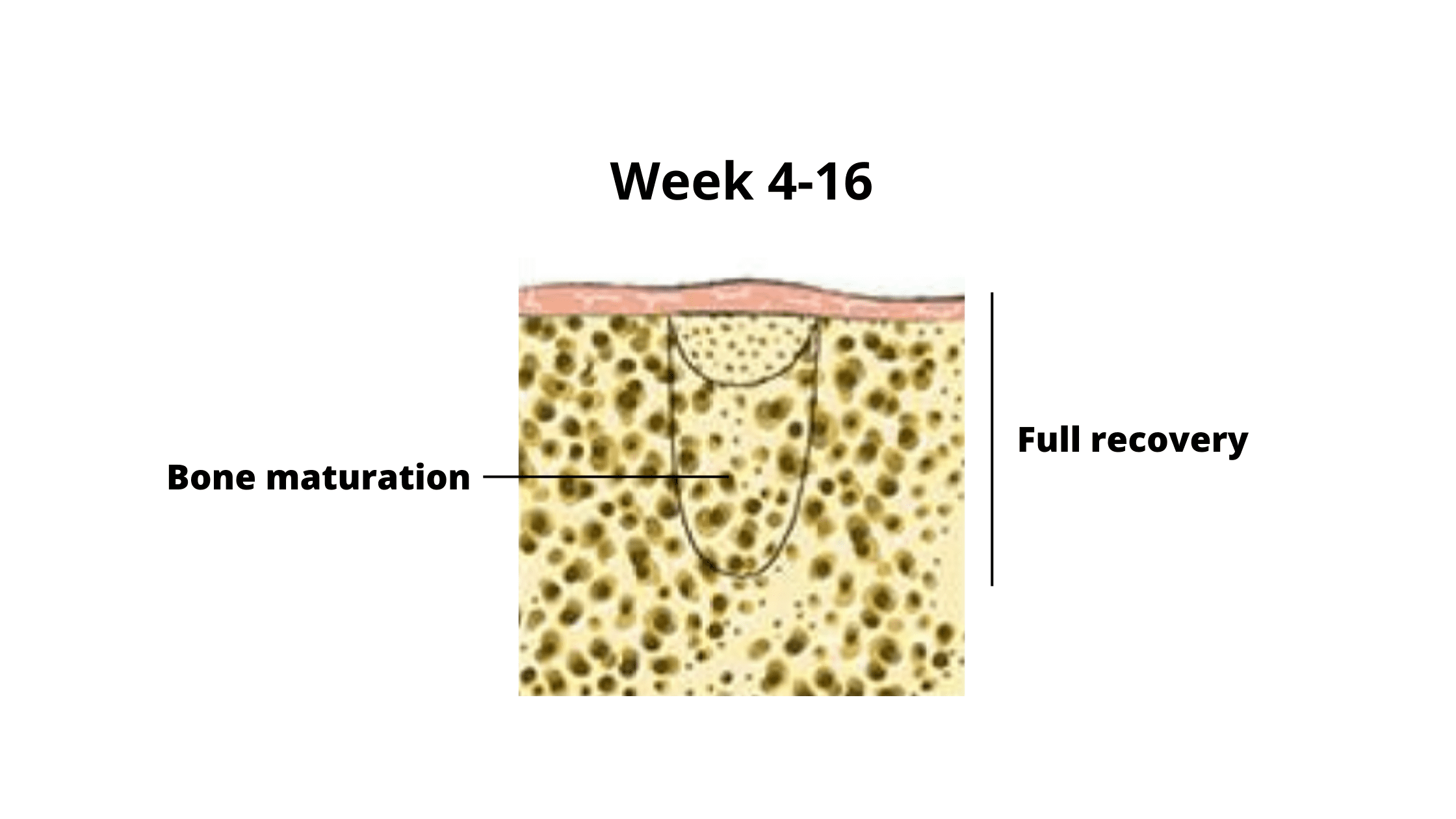 The immature bone gradually starts to harden and become stronger through a process called mineralization.
This phase can take weeks to months, depending on factors like your age, overall health, and the body’s ability to repair.
The immature bone gradually starts to harden and become stronger through a process called mineralization.
This phase can take weeks to months, depending on factors like your age, overall health, and the body’s ability to repair.
Even after the socket has healed, the bone continues to remodel and reshape over time. When a tooth is missing, the bone may start to shrink or break down due to lack of stimulation.
This bone loss occurs most rapidly during the first year after extraction, then continues at a slower rate over time.
How can you prevent bone loss?
The only effective solution is to replace the missing tooth with an implant. Implants function like natural teeth, keeping the bone stimulated and helping preserve its shape and volume.
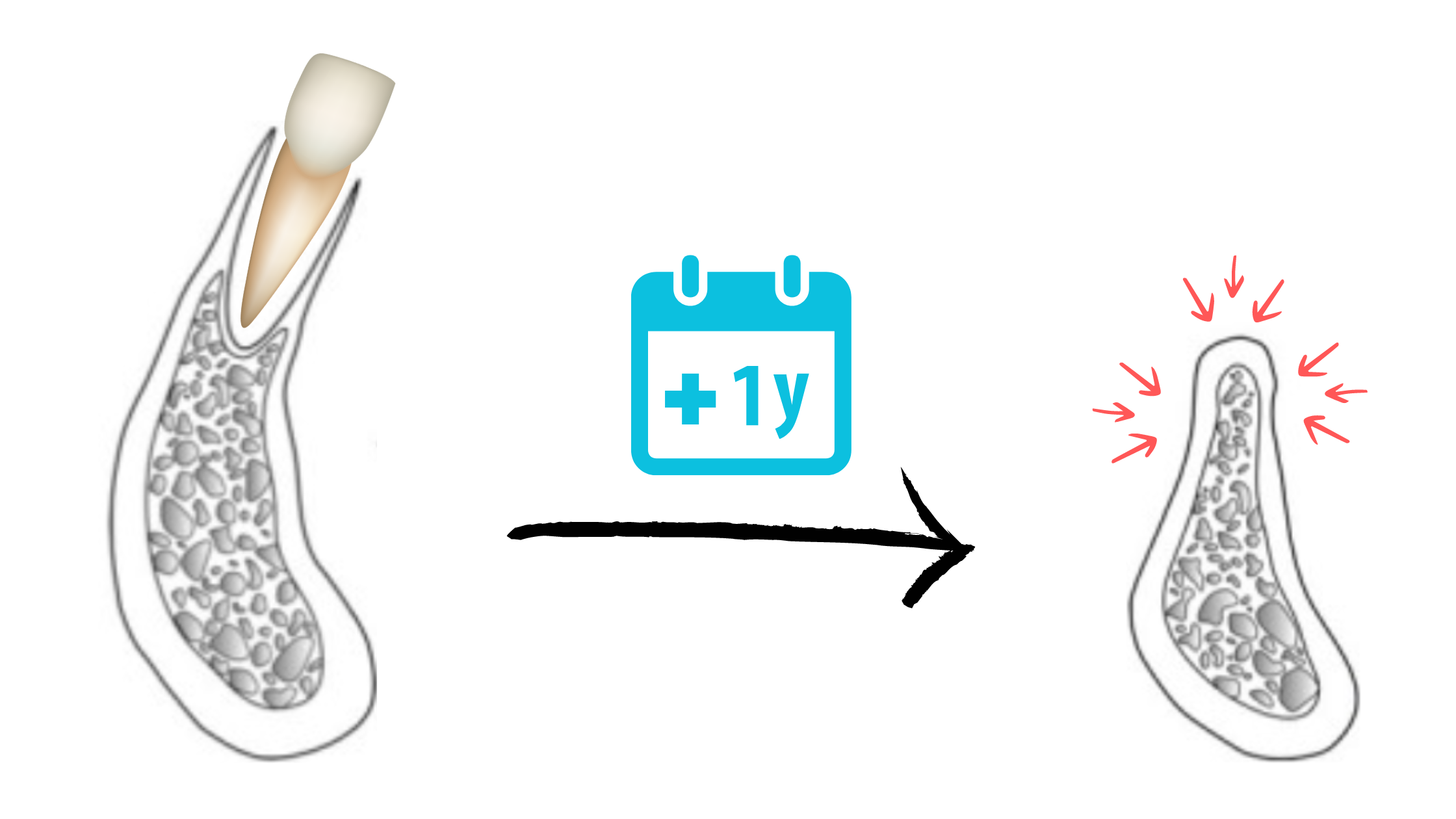
Bone loss after tooth extraction (1)
What factors can impact healing?
The time it takes for a tooth extraction wound to heal and the way tissues mature can vary from person to person. Several factors can impact healing, including:1. Smoking:
Smoking is one of the main causes of complications after tooth extraction. Tobacco contains hundreds of harmful chemicals that reduce blood flow and affect how cells function, slowing down healing.
A study found that smokers are three times more likely than non-smokers to develop a painful complication called “dry socket,” which happens when the blood clot is lost too soon.
Smoking can also worsen bone loss after healing, making future implant placement more challenging.
2. Extraction Technique:
More complex extraction procedures, such as those involving drilling on the bone, can lead to longer recovery times compared to simple extractions.
3. Age:
As we age, the body’s ability to heal and repair slows down. Older individuals may experience slower healing and more bone loss after extraction.
4. Following Your Surgeon's Instructions:
It’s very important to carefully follow the post-op instructions from your dentist or surgeon. These cover your diet, physical activity, and medications. Not following these instructions can cause complications and delay healing.
5. Nutrition:
The body needs different nutrients to build tissues and produce strong, healthy bone. Make sure your diet is healthy and covers your needs of vitamins, minerals, and proteins.
6. Oral hygiene:
Good oral hygiene helps keep the extraction site clean and prevents infection. Starting the second day, gently brush your teeth—avoiding the wound—and rinse your mouth with salt water several times daily. Don’t forget to clean your tongue too.
7. Certain Medical Conditions:
Medical conditions like diabetes can slow down healing and increase the risk of infection.
People with diabetes or other immune system conditions need to be extra careful during recovery to prevent infections.
How do I know if the healing is failing?
Tooth extraction is usually a safe procedure, but sometimes healing can be delayed or complicated—especially in people who smoke or have diabetes.Here are some symptoms to watch for:
The blood clot did not form:
If the blood clot does not form correctly or is dislodged within the first day, it can cause excessive bleeding and lead to a dry socket, which is extremely painful and can also delay healing.
Bad breath and pus leaking:
If you notice yellowish or pale fluid leaking from the wound, or bleeding without a clear reason, this could be a sign of infection. If you think the socket might be infected, don’t wait—see your dentist right away. Infections won’t heal on their own and can only get worse.
Swelling days after the procedure:
Swelling is a normal side effect after surgery. It usually peaks around the third day and then gradually goes down.
However, if the swelling keeps getting worse instead of improving, or if it comes with severe pain, bad breath, pus discharge, or fever, it could be a sign of a socket infection or facial cellulitis.
If you suspect an infection, again, don’t delay it!
Severe pain that's getting worse:
Intense, persistent, or throbbing pain that doesn’t get better over time should not be ignored.
Also, sudden pain that returns after having disappeared should be checked by your dentist.
Fever, nausea, vomiting, difficulty breathing:
These are signs of a serious systemic infection and should be taken very seriously.
While they are rare in healthy people, those with weakened immune systems are more vulnerable.
If you experience any of these symptoms, seek emergency medical care immediately.
- Wound healing of extraction sockets https://onlinelibrary.wiley.com/doi/abs/10.1111/etp.12016
- Smoking as a Risk Factor for Dry Socket: A Systematic Review https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9317683/
- Diabetes & Oral Health https://www.nidcr.nih.gov/health-info/diabetes
- Aetiology of dry socket: a clinical investigation https://pubmed.ncbi.nlm.nih.gov/5244107/
- Complications After Dental Treatment https://www.msdmanuals.com/home/mouth-and-dental-disorders/urgent-dental-problems/complications-after-dental-treatment