Tooth Extraction: Everything You Need to Know
 Most dental treatments aim to keep teeth in the mouth as long as possible. However, sometimes extraction or tooth removal is the last option.
Most dental treatments aim to keep teeth in the mouth as long as possible. However, sometimes extraction or tooth removal is the last option.
While the thought of having a tooth removed may cause some anxiety, understanding the process and what to expect before, during, and after the procedure can help ease your concerns and ensure a smooth recovery.
In this article, we will cover everything you need to know about tooth extraction, from the reasons why you may need it, to the potential risks and complications, and the best ways to care for your mouth during the healing process.
Key takeaways:
- Tooth extraction is a common dental procedure that involves removing a damaged or decayed tooth from the mouth.
- The procedure is performed under local anesthesia. You may experience some symptoms, such as pain, swelling and bleeding in the days following the extraction. These reactions are normal and temporary. .
- It's important to follow your dentist's instructions for aftercare, including avoiding smoking, alcohol, and strenuous physical activity.
- Complications from tooth extraction are rare but can include dry socket, infection, and nerve damage.
- After healing, it's important to consider replacing the missing tooth to prevent bone loss and tooth displacement.
What is tooth extraction?
Tooth extraction is a dental procedure in which a tooth is removed from its socket in the jawbone. This treatment is usually the last option to consider when the tooth is severely damaged, decayed, or infected and cannot be restored with other dental.Although the thought of tooth extraction may sound scary, the good news is that the procedure is usually less painful than most people think. Thanks to advanced anesthesia techniques, your dentist can numb the area around the tooth, and you won't feel any pain during the procedure. Your dentist may also recommend pain medication to manage any discomfort you may experience after the treatment.
When does tooth extraction become necessary?
As dentists, we always strive to conserve teeth whenever possible. In most cases, we will try to save a tooth with conservative treatments like root canal therapy, crowns, or fillings. However, in some situations, tooth extraction becomes necessary. Here are the most common reasons why:- Significant tooth decay: When a large portion of the tooth is destroyed, it may be difficult to restore it with a crown or filling. The tooth may not be able to support a restoration, and extraction may be necessary.
- Tooth fracture: Superficial tooth fractures can usually be repaired with a crown or filling. However, if the fracture extends deep into the tooth or reaches the roots, the tooth may not be salvageable, and extraction may be the only option.
- Failed root canal treatment: Root canal therapy has a high success rate, but there are cases where the procedure may fail or become difficult to redo. In these cases, the tooth may need to be removed.
- Severe destruction of the bone around the tooth: Teeth are held in place by the surrounding bone. If the bone is severely destroyed, the tooth may not have enough support to stay in place.
- Severe tooth crowding: Sometimes, teeth may become too crowded. Extraction of one or more teeth may be necessary to make room for proper alignment as part of orthodontic treatment.
What do I need to know before having a tooth extraction?
Tooth extraction is generally a safe procedure, but it's essential to be aware of any risks or potential complications, especially if you have certain medical conditions. Here are some important things to consider before the procedure:- Taking blood thinners: If you are taking blood thinners, your dentist or surgeon may need to adjust your medication before the procedure to prevent excessive bleeding. Therefore, it's essential to inform your dentist before the extraction of any medications you are taking.
- Medications and conditions that affect the immune system: These can include diabetes, leukemia, chemotherapy, and corticosteroids, which can increase the risk of infection after the extraction. Your dentist or surgeon may need to take additional precautions to ensure that the area around the extraction site remains sterile and infection-free.
- High risk of endocarditis: Endocarditis is a bacterial infection that can affect the heart valves. People at high risk include those with a heart device or congenital heart disease. If this is your case, your dentist or surgeon may prescribe antibiotics before and after the procedure to reduce the risk of infection.
The different techniques of tooth extraction:
There are two main techniques of tooth extraction: simple extraction and surgical extraction.Simple Extraction:
This is a fast and straightforward technique that is typically used to remove moderately damaged teeth with simple anatomy. Here are the steps involved in the procedure:
- Anesthesia: Before starting the procedure, the dentist will administer local anesthesia to numb the area around the tooth.
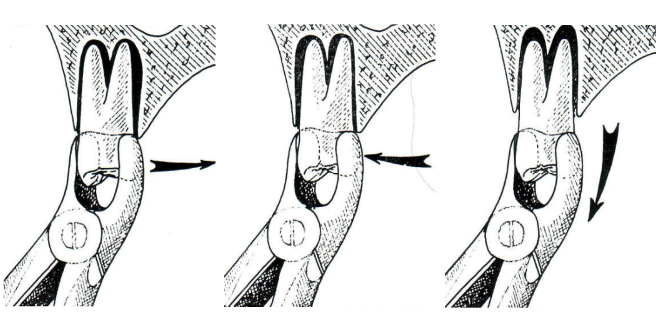
- Loosening the tooth: The dentist will then use a special tool called an elevator to loosen the tooth from the socket.
- Removing the tooth: Once the tooth is sufficiently loosened, the dentist will use forceps to remove it from the socket.
- Cleaning the socket: After the tooth is removed, the dentist will clean the socket and may pack it with gauze to help control bleeding.
- Post-operative instructions: The dentist will provide you with post-operative instructions, including how to care for the extraction site and what to do if you experience any pain or swelling.
Surgical Extraction:
This is a more complex procedure that requires a small incision in the gum and the removal of part of the bone surrounding the tooth to gain access to it.
This technique is indicated when the tooth is too damaged or when the shape of the roots is unusual, making the simple extraction technique difficult.
The image below shows how the roots of a wisdom tooth are curved, requiring a more complex procedure.

Curved root requiring a surgical extraction
What to expect after the procedure?
After tooth extraction, your body will undergo several natural reactions as it begins to heal. Here's what you can expect in the first few hours and days following the procedure:1. Numbing Sensation:
To extract the tooth, your dentist will give you a local anesthetic. This can cause a numbing sensation that may last for a few hours after the procedure. During this time, be careful not to bite your cheeks, lips, or tongue. If you experience any problems related to the anesthesia, contact your dental surgeon immediately.2. Bleeding:
After removing the gauze your dentist placed in your mouth after the procedure, you may experience bleeding. Here's how to control it:- Place a piece of sterile gauze on the extraction site and bite down on it for a few minutes.
- Avoid using a straw, rinsing, or spitting for at least 24 hours to prevent dislodging the blood clot that forms in the extraction site.
- Don't smoke or drink alcohol for the first week, as this can irritate the wound and delay healing. If bleeding persists or becomes severe, contact your dental surgeon immediately.
3. Swelling and Pain:
It is common to experience some pain and swelling in the area where the tooth was removed. This is a natural reaction of your body's immune system and should resolve within a few days. To reduce swelling and manage pain, try the following tips:- Apply a cold compress to the affected area for the first 24 hours.
- Rinse your mouth with warm salt water on the second day.
- Eat soft foods and avoid hot, spicy, or hard foods.
- Take pain relievers as recommended by your dental surgeon.
4. Limited Mouth Opening:
After tooth extraction, you may experience limited mouth opening due to swelling or pain. This can make it difficult to speak, eat, and brush your teeth. You can use a warm compress to relax your jaw muscles.The potential complications of tooth extraction:
While tooth extraction is generally considered a safe and routine procedure, as with any medical intervention, there are potential complications that can arise.Some complications can occur during the procedure itself, while others may develop in the days and weeks following the extraction. It's important to be aware of them so you can take steps to minimize your risk and seek prompt treatment if necessary.
Here are the most common potential complications during and after the procedure:
During the procedure:
- Anesthesia-related complications: such as an allergic reaction or excessive sedation.
- Trauma to adjacent teeth or soft tissues: if the dentist or surgeon accidentally damages neighboring structures while removing the tooth.
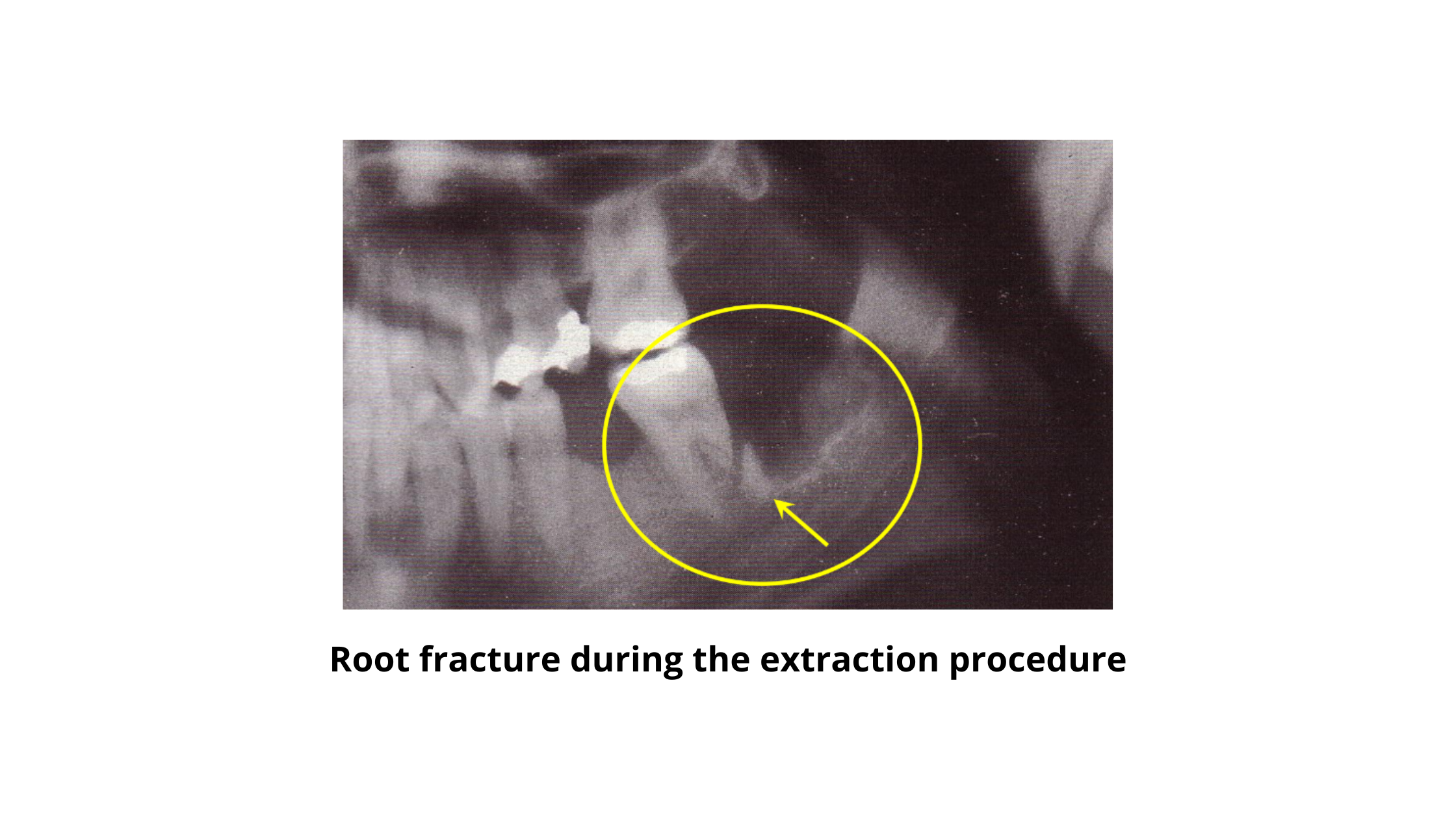
- Bone fracture: If the tooth is difficult to extract, or if the bone is weakened by conditions such as osteoporosis, the bone supporting the tooth may come out.
- Sinus damage: if the tooth being extracted is located near the sinuses and the surgeon accidentally creates a hole or tear in the sinus membrane.
After the procedure:
- Dry socket: occurs when the blood clot that forms in the socket where the tooth was removed becomes dislodged or dissolves, exposing the underlying bone and nerves. This can delay the healing process.
- Infection: if bacteria enter the extraction site and multiply, leading to swelling, pain, and fever.
- Hematoma: occurs when blood collects under the skin, causing discoloration, swelling, and discomfort.
- Bleeding: normal in the first few hours after the procedure but can become problematic if it persists or becomes severe.
- Nerve damage: can occur if the nerves in the surrounding area are damaged during the extraction, leading to numbness or tingling in the lips, tongue, or jaw.
Healing and recovery:
Healing and recovery after tooth extraction can take some time. It usually takes about 1-2 weeks for the socket to heal, but this can vary depending on the complexity of the extraction and your healing ability.Remember that the blood clot that forms immediately after surgery is crucial to a good recovery. It protects the underlying bone and nerves and promotes new tissue formation.
Therefore, you should not damage or manipulate the clot by sucking into the wound or spitting vigorously for the first day. Doing so can dislodge it and cause dry socket, one of the most common post-operative complications.
It is also vital to follow your dentist or surgeon's instructions carefully. These instructions may include guidelines on pain management, oral hygiene, diet, and physical activity.
What comes next?
Once the socket has healed, the next step is to replace the missing tooth.This is an essential step because leaving the gap between your teeth can lead to a range of problems. These include bone loss, shifting of the remaining teeth, and difficulty chewing.
Implants are an excellent option for replacing a missing tooth as they mimic the natural tooth root and stimulate the bone, preventing bone loss. They also provide a durable, long-lasting solution.
A dental bridge is another option that can replace a missing tooth. While it doesn't stimulate the bone, it offers a stable and functional replacement that prevents tooth displacement and ensures efficient chewing.
It is essential to discuss these options with your dentist to determine the best course of action for your situation.
- Assessment of extracting molars and premolars after root canal treatment: A retrospective study https://www.sciencedirect.com/science/article/pii/S1013905219300215
- Wound healing of extraction sockets https://onlinelibrary.wiley.com/doi/abs/10.1111/etp.12016
- Case Report: Late Complication of a Dry Socket Treatment https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3022165
- Alveolar Osteitis https://www.ncbi.nlm.nih.gov/books/NBK582137/
- The bacteremia of dental origin and its implications in the appearance of bacterial endocarditis https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3909435/
- Complications After Dental Treatment https://www.msdmanuals.com/home/mouth-and-dental-disorders/urgent-dental-problems/complications-after-dental-treatment