Tooth Extraction Complications: A Comprehensive Guide with Pictures

Tooth extraction is one of the most routine dental procedures. It is usually quick, straightforward, and with minimal risk of complications.
However, just like any surgical procedure, certain risks do exist, especially when the extraction is complex or takes longer than usual. Complications can occur during the procedure, immediately after, or even in the weeks or months that follow.
We’ll break down the most common complications after a tooth extraction, so you know exactly what to expect — and how to manage them properly for a smooth, pain-free recovery.
However, just like any surgical procedure, certain risks do exist, especially when the extraction is complex or takes longer than usual. Complications can occur during the procedure, immediately after, or even in the weeks or months that follow.
We’ll break down the most common complications after a tooth extraction, so you know exactly what to expect — and how to manage them properly for a smooth, pain-free recovery.
In this article:
1. Common Pre-Extraction Concerns (what I often get asked)
2. Complications During the Tooth Extraction Procedure (Intraoperative side effects)
- Anesthesia-Related Complications
- Injury to Adjacent Teeth and Surrounding Soft Tissue
- The Tooth May Break Off
- Bone Damage during Tooth Extraction
- Sinus Exposure
- Bleeding During Tooth Extraction
3. Immediate Complications After Tooth Extraction (Postoperative side effects)
- Dry Socket
- Bleeding After Tooth Extraction
- Infections
- Nerve Complications
- Difficulty Opening the Mouth (Trismus)
- Subcutaneous Emphysema
4. Long term side effects
5. Factors that Increase the Risk of Complications
6. Ensure a Smooth Recovery
7. Takeaway
Common Pre-Extraction Concerns (what I often get asked)
Before the tooth extraction procedure, it's normal to have some common concerns. Many patients often ask about pain, swelling, bleeding, and how the procedure may affect their daily activities. Here are the most common questions:Will it hurt?
Pain when the numbness wears off is completely expected. This can be managed by pain medication.Will I swell?
Swelling is completely normal after the procedure. It's a natural part of the healing process, and we'll discuss ways to reduce it.What if I bleed?
Some bleeding in the first day is common. However, heavy bleeding may require additional treatment.Will I be able to work?
You may need a day or two off to rest and recover.What should I eat?
Eating may be challenging initially. You may have difficulties swallowing and opening your mouth. But as healing progresses, you can gradually resume your usual diet. These expected postoperative side effects are temporary and part of the healing process. They are completely different from the complications we'll discuss next.Complications are uncommon, unexpected issues that can arise during or after the procedure..
Potential Complications During the Tooth Extraction Procedure (Intraoperative side effects)
What the Studies Say:
Below are studies on wisdom tooth removal complications:
- Sebastiani (2014): Intraoperative complication rate of 6.19%, mainly tuberosity fracture ((the bone behind the upper wisdom teeth)) and bleeding.
- Sayed (2019): Complication rate of 3.7%, mostly tuberosity fracture, root fracture, and bleeding.
Anesthesia-Related Complications
Dental anesthesia is a routine and safe part of many dental procedures. It helps ensure your treatment is comfortable and pain-free.
Complications from dental anesthesia are rare. Even when they do happen, they’re usually minor and temporary. These can range from mild pain, bleeding, or nerve irritation to more serious (but very rare) issues like cardiovascular reactions, toxicity, or allergies.
- Discomfort: You might feel a slight sensation at the injection site, but it’s usually minimal and barely noticeable.
- Nerve injury: If this occurs, you may experience temporary tingling, prickling, or numbness. These sensations almost always resolve on their own. For lower molars, there’s a small risk of the anesthetic being injected near the facial nerve, which controls your facial movements. This can cause temporary facial weakness or paralysis, but it typically disappears within a few hours.
- Blood vessel injury: Accidental injury to a small blood vessel can lead to internal bleeding, which may cause mild swelling, bruising, or difficulty opening your mouth. That's also harmless and usually resolves quickly.
- Serious reactions (rare): Allergic reactions, cardiovascular issues, or anesthetic toxicity are very rare but can be serious. Warning signs include skin rashes, facial swelling, chest pain, palpitations, dizziness, or difficulty breathing.
Injury to Adjacent Teeth and Surrounding Soft Tissue
When the dentist loosens the tooth using sharp instruments, there’s a risk of accidentally injuring nearby teeth or surrounding soft tissues.
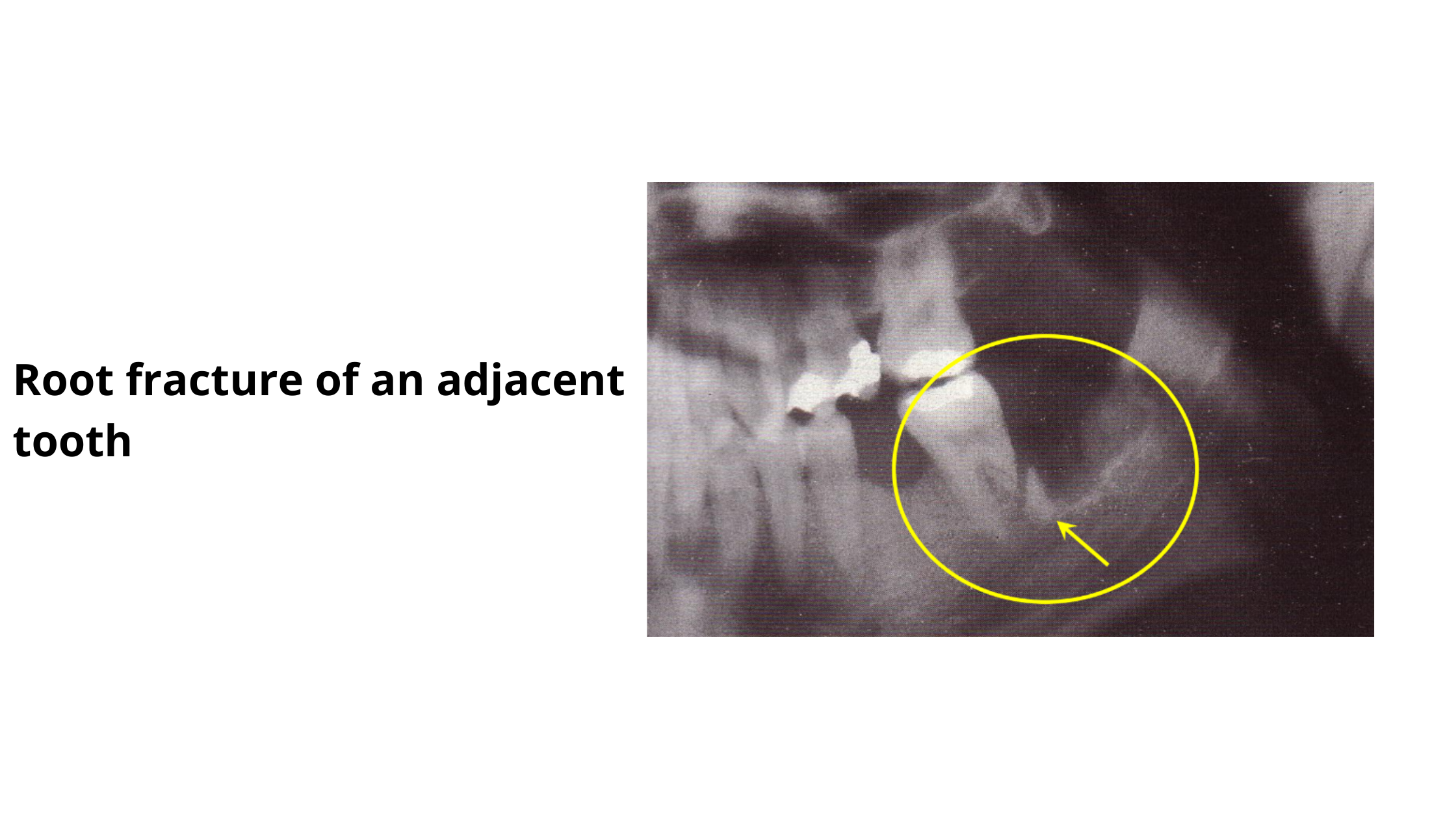
When a nearby tooth is accidentally damaged, the injury may be as small as a tiny crack or, worse, the roots can break and become dislodged, which can ultimately lead to tooth loss.
The surrounding soft tissues — including the cheeks, lips, tongue, and roof of the mouth — can also be accidentally injured. They may be cut or pierced, causing pain and bleeding.
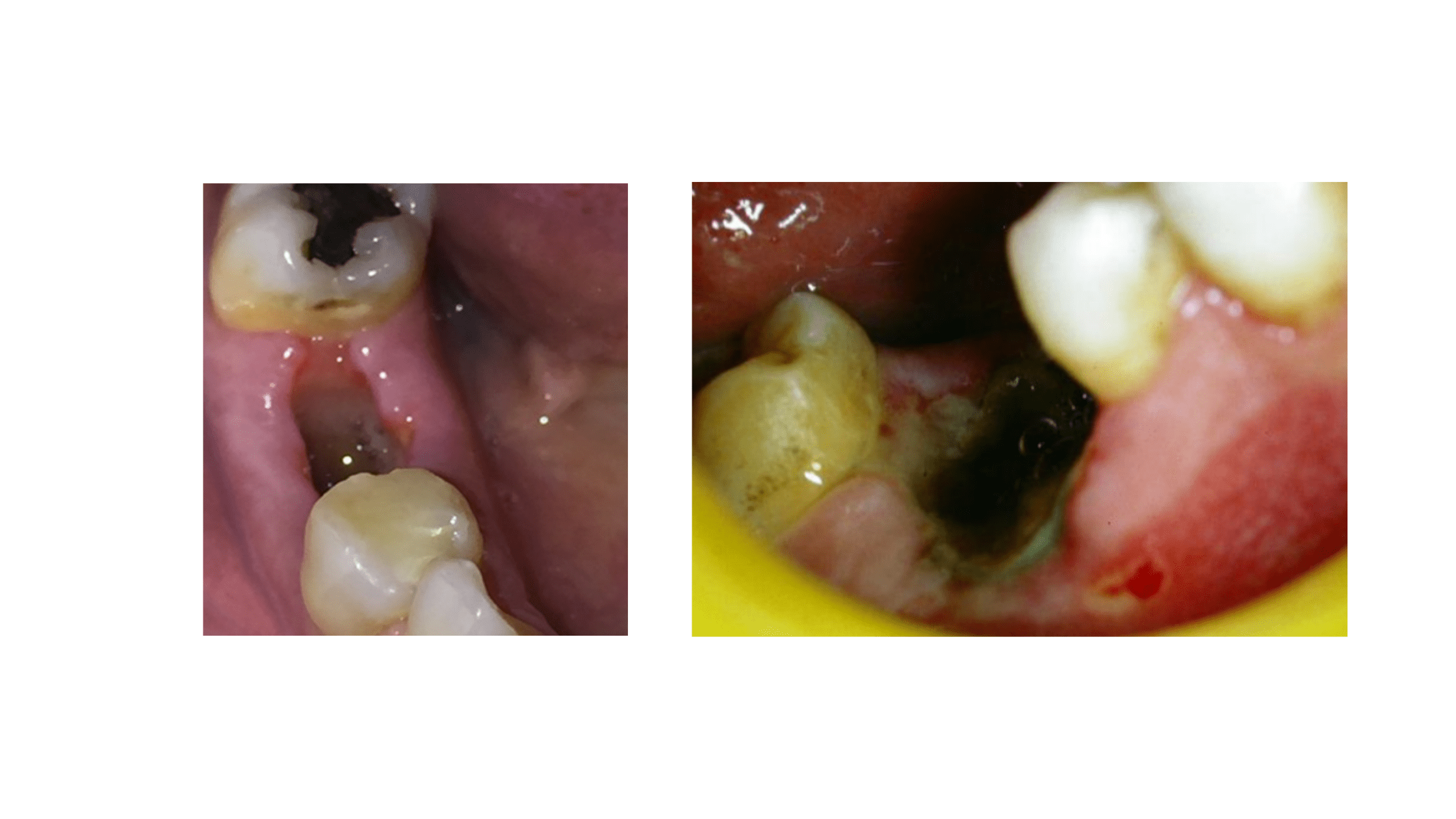
The Tooth May Break Off
A relatively common complication is when the tooth breaks off during the procedure. Instead of coming out entirely, the tooth may fracture, leaving a portion of the root trapped within the bone.
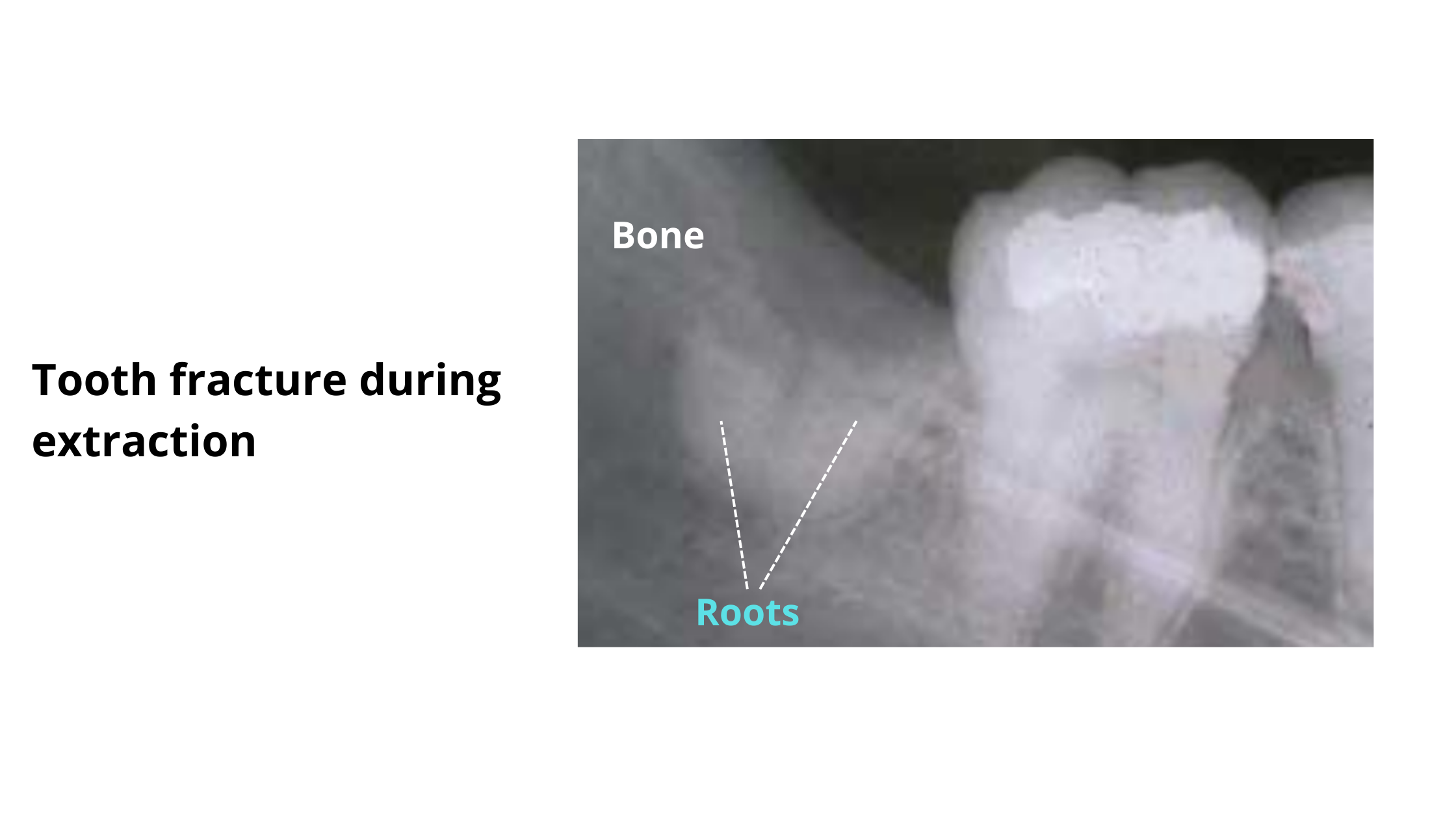
This is more likely when the tooth is already weak or has undergone a root canal, as it can easily fracture.
The trapped roots can be removed with ease, but it's not always the case. Often, they require removal some of the supporting bone, which can lead to a longer recovery time.
Bone Damage during Tooth Extraction
It's not uncommon for a small bone fragment to break off or come out with the tooth. Usually, this is a minor issue and should not be a cause for concern.
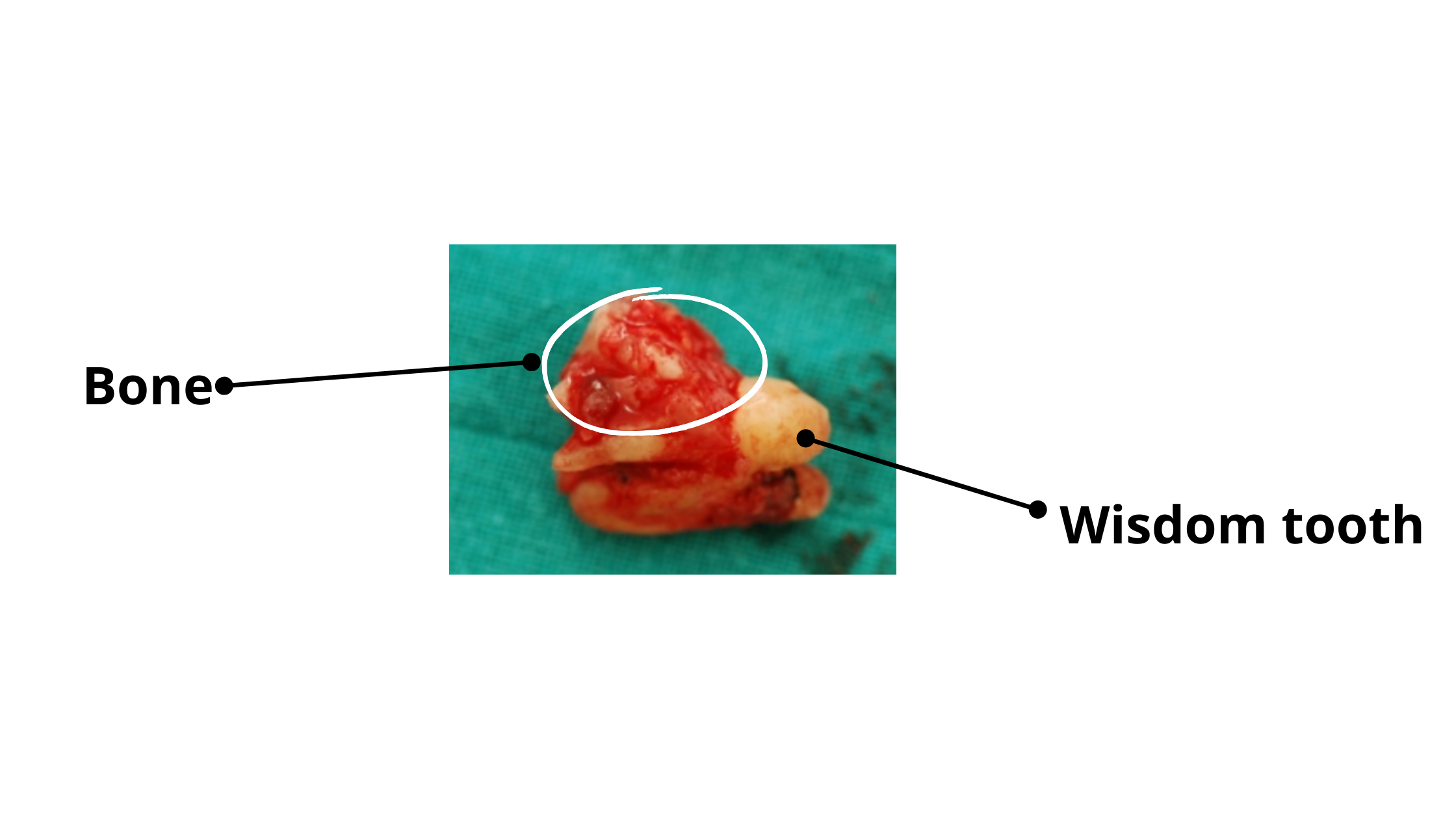
In more severe cases, when a large portion of bone becomes loose or displaced, the dentist can reposition and stabilize it so it can heal and fuse with the jawbone.
If the bone damage is so extensive and involves the deepest part of the jaw, it’s a more serious complication that requires immediate care from a specialist, such as a maxillofacial surgeon or ENT.
Sinus Exposure
The sinuses are air-filled bony cavities located in the cheekbones, on either side of the nose.
The most common cause of sinus exposure is the removal of the back teeth of the upper jaw. The highest-risk teeth are the second molar and wisdom teeth, followed by the first molar and then the first premolar.
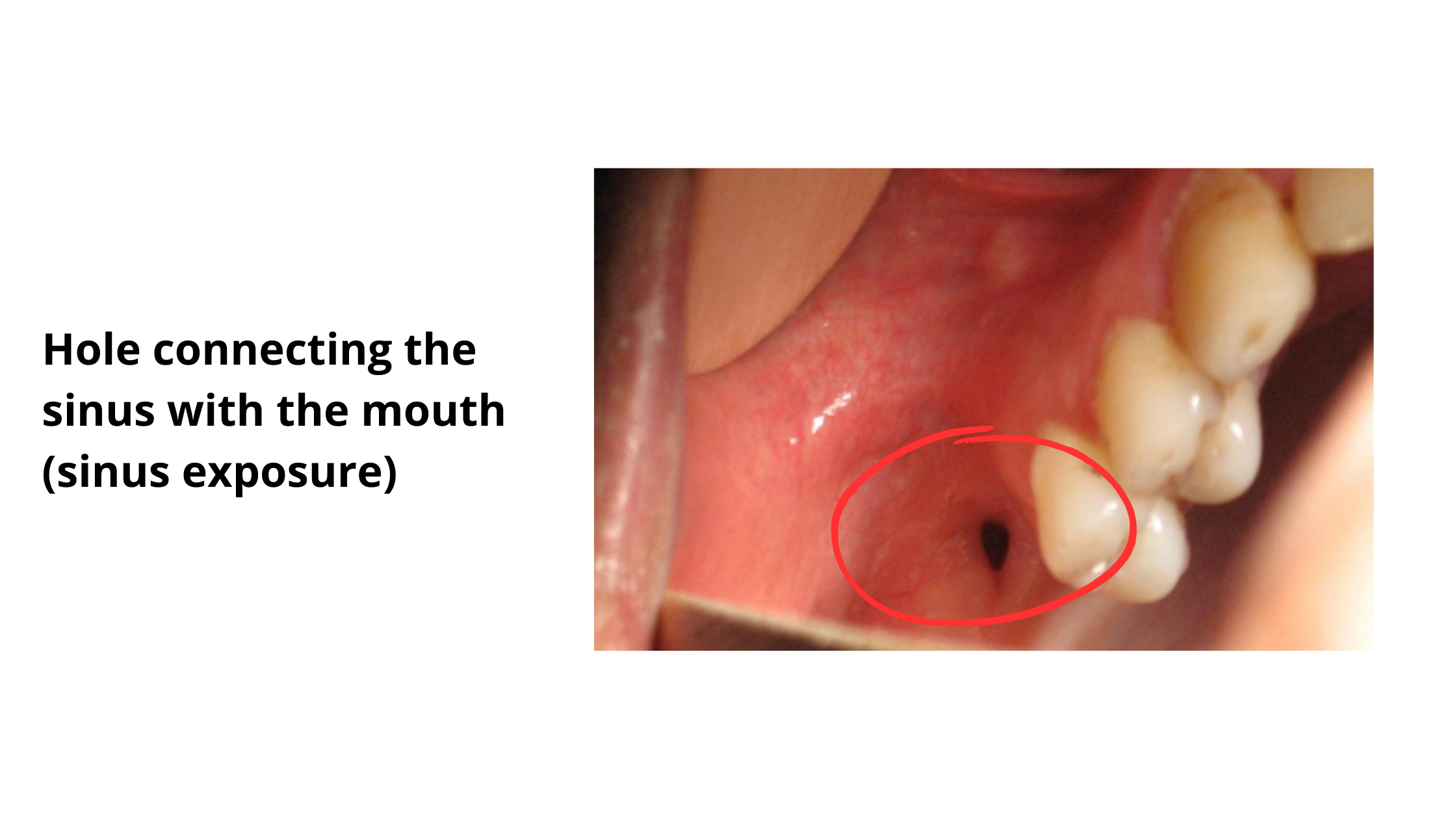
These upper back teeth are located just below the sinuses and can have direct connections to them. During extraction, the soft sinus lining may be damaged or perforated, creating an open passage between the mouth and the sinus.
This can allow saliva, food debris, and bacteria to enter, potentially causing sinus infection (sinusitis).
Symptoms of sinus damage during the procedure include:
- Feeling as if an instrument is being pushed upward
- Excessive bleeding during the procedure
- A piece of bone coming out with the tooth
- Pus leakage from the wound, sinus pressure, and nasal congestion (later symptoms of sinusitis)
Bleeding During Tooth Extraction
While bleeding during the procedure is typically manageable and controllable, it can be serious for patients with specific medical conditions.
Patients with conditions that affect blood clotting — such as hemophilia, platelet deficiency (thrombocytopenia), clotting factor deficiencies, or those taking blood thinners — may have more severe and potentially life-threatening bleeding.
That's why it's so important to inform your dentist or surgeon of any medical conditions, as well as any medications you are currently taking. Some measures may need to be taken for a safer procedure.
Immediate Complications After Tooth Extraction (Postoperative side effects)
What the Studies Say:
Studies on post-operative wisdom tooth complications found:
- Chiapasco (1993): Postoperative complications occurred in 4.3% of lower wisdom teeth and 1.2% of upper wisdom teeth.
- Sigron (2014): Overall complication rate was 8.4% for 1,199 extractions; dry socket was the most common.
- Sayed (2019): Postoperative complications occurred in 8.3%; nerve injuries were most frequent (7.2%).
Dry Socket
Dry socket is one of the most common post-operative complications. It occurs in about 0.5–5.6% of cases, and up to 30% for surgically removed lower wisdom teeth.
After a tooth is extracted, a blood clot forms in the empty socket. This clot stops bleeding and protects the wound as it heals.
Dry socket happens when the clot is lost too early or fails to form, leaving the socket exposed. It usually appears 2–3 days after the extraction and causes severe pain that can be so bad that it does not respond to painkillers.
On top of that, dry socket delays healing and can increase the risk of infection in the socket.
Bleeding After Tooth Extraction
Bleeding can continue for a few hours after the procedure. This is completely normal and usually mild. You can manage it at home by gently biting on a clean compress for a few minutes.
Sometimes, blood mixes with saliva, making the bleeding appear heavier than it actually is.
Internal bleeding happens when the blood pools inside the wound and spreads into deeper tissues, causing bruising — the black, green, or yellow discoloration often seen after surgery. Bruising is harmless and fades as the body clears the blood.
Occasionally, blood can collect in one spot under the skin, forming a firm, rubbery lump called a hematoma. Most hematomas are harmless and disappear naturally as healing progresses.
When to Seek Help:
- Excessive Bleeding: Reach out to your dentist if bleeding is too excessive or you cannot control it on your own.
- Persistent Bruising or Hematoma: Bruising or hematoma that doesn't resolve after a week or so should also prompt you to talk to your dentist to rule out any infection.
Infections
Infections after dental extractions can sometimes occur, even after a smooth procedure. They may develop immediately or several days later.
These infections happen when bacteria from the mouth enter the socket, often due to something trapped in the wound, such as a food particle, a piece of tartar, or a fragment of the tooth.
The type of infection depends on the tooth’s position and whether it was previously infected. These include:
- Socket Infection (Alveolitis): Infection develops inside the bony socket. Signs include pus, grey/brown material filling the socket, bad taste, bad breath, and red, swollen gums. Pain is usually mild compared to dry socket.
- Bone Infection (Osteitis): Infection spreads deeper into the jawbone, causing severe pain, swelling, fever, fatigue, and swollen neck lymph nodes.
- Facial Cellulitis: Infection spreads to surrounding facial soft tissues, like the cheek, chin, or under the tongue, forming a drainage path (fistula).
- Sinusitis: Only occurs with upper back teeth when the sinus lining is accidentally damaged, allowing bacteria or debris to enter and cause infection.
Nerve Complications
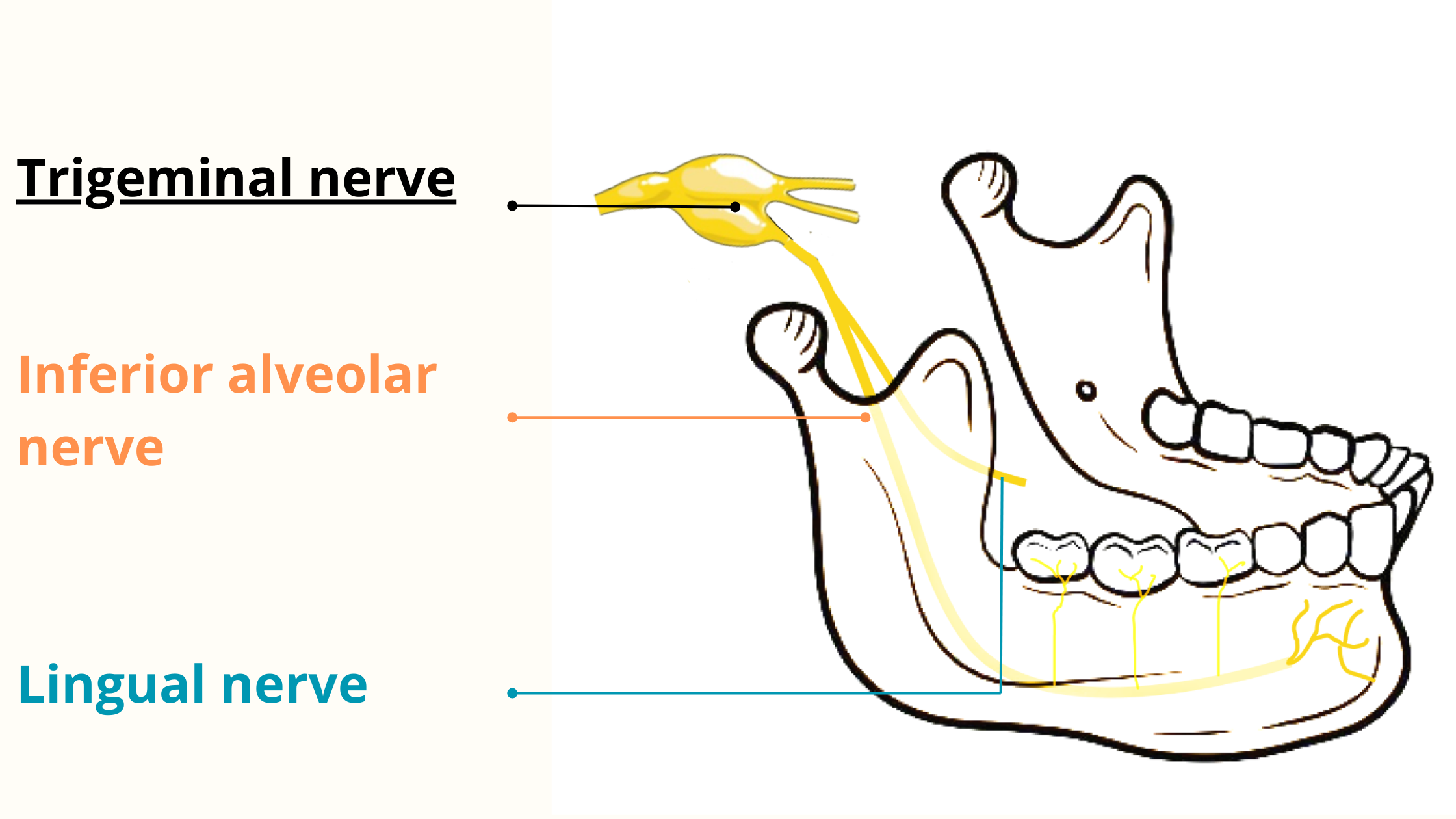
Nerve complications are frequently associated with lower wisdom teeth, as these are often close to major nerves like the inferior alveolar nerve (IAN) and the lingual nerve (LN). Sometimes, these nerves are in direct contact with the roots, making an injury almost inevitable.
The IAN and LN are sensitive nerves responsible for providing sensation to most of the mouth and face, including the teeth, lips, tongue, lower cheeks, and chin.
Injuring these nerves may lead to lasting sensory disturbances such as tingling, numbness, or a burning sensation. But this can never lead to facial paralysis, as these nerves do not control muscle movement.
The duration of symptoms can vary, ranging from a few weeks to over a year. Permanent damage is rare, occurring in no more than 2% of cases.
Difficulty Opening the Mouth (Trismus)
Having trouble opening your mouth, known as "Trismus," is a common and expected reaction after a dental extraction.
Keeping your mouth open for a long time during an extraction can put strain on the muscles and joints. This is especially true for more complex or lengthy procedures.
Damage to a muscle — whether from a needle or a sharp instrument — can cause muscle soreness that limits how wide you can open your mouth. Internal bleeding or swelling can also put pressure on the muscles, further restricting jaw movement in the first few days.
Trismus typically resolves within one or two weeks following the extraction. However, if the difficulty persists longer, it may indicate an underlying issue, such as an infectious complication or trauma.
Subcutaneous Emphysema
Subcutaneous emphysema is an extremely rare but potentially serious complication that can occur when air gets trapped under the skin.
The telltale sign is severe swelling that produces a crackling or popping sensation when touched, known as crepitus. Symptoms can appear rapidly, from a few minutes up to a few hours after the procedure.
While it's mostly harmless, subcutaneous emphysema can lead to severe infections. Trapped air along with bacteria can leak into nearby areas, potentially reaching vital structures like the neck, chest, and lungs.
Long term side effects
The following complications do not appear overnight after the procedure but after months or even years.Changes in Bone Shape After Healing
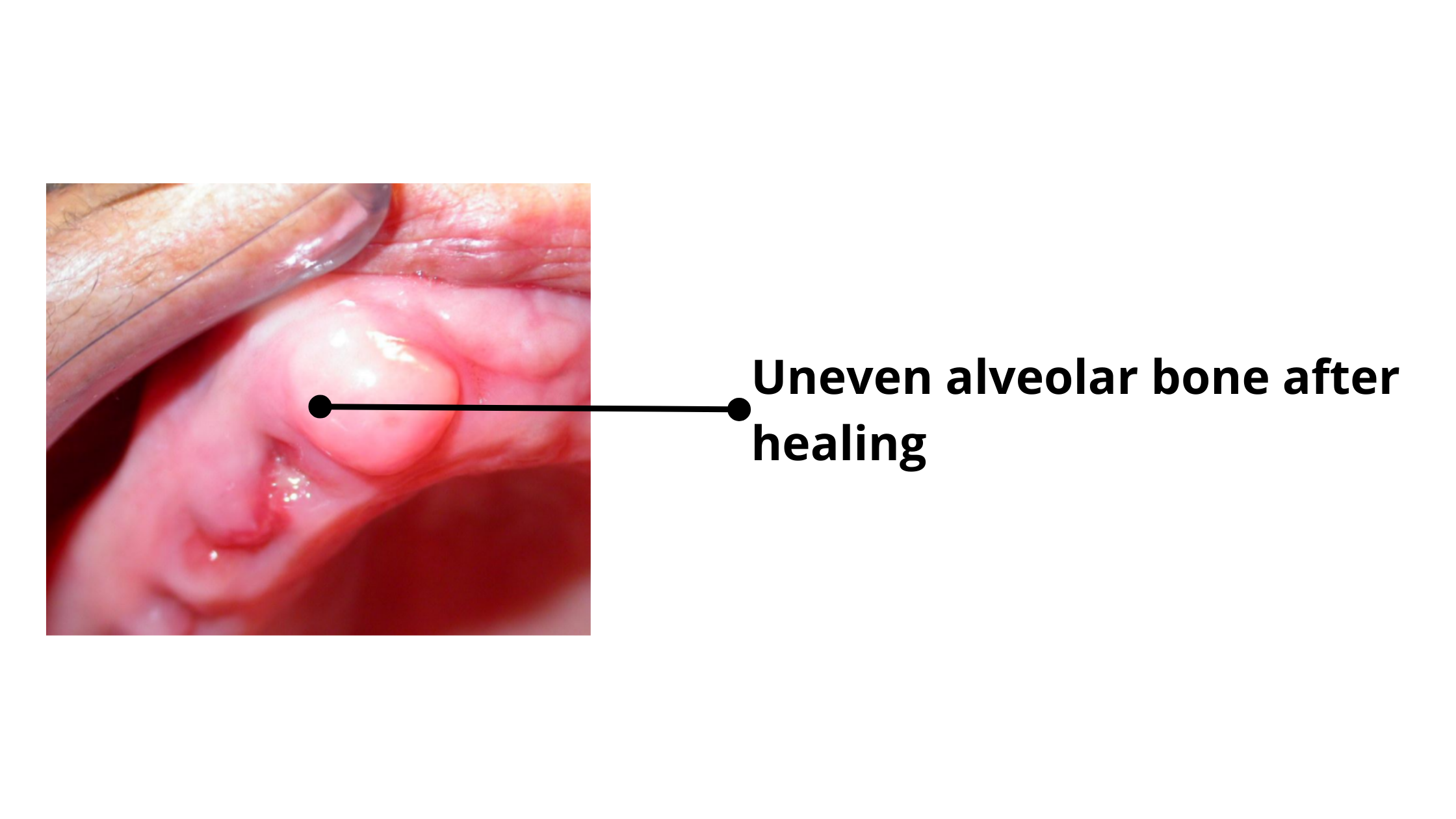
Following tooth extraction, the healing process may result in irregularities in the shape of the bone, where one surface becomes more prominent than the other. This can pose challenges, especially if you're planning to replace the missing tooth.
Before considering an implant or denture, the bone must first be leveled and smooth out to ensure both aesthetic and functional outcomes.
Bone Loss
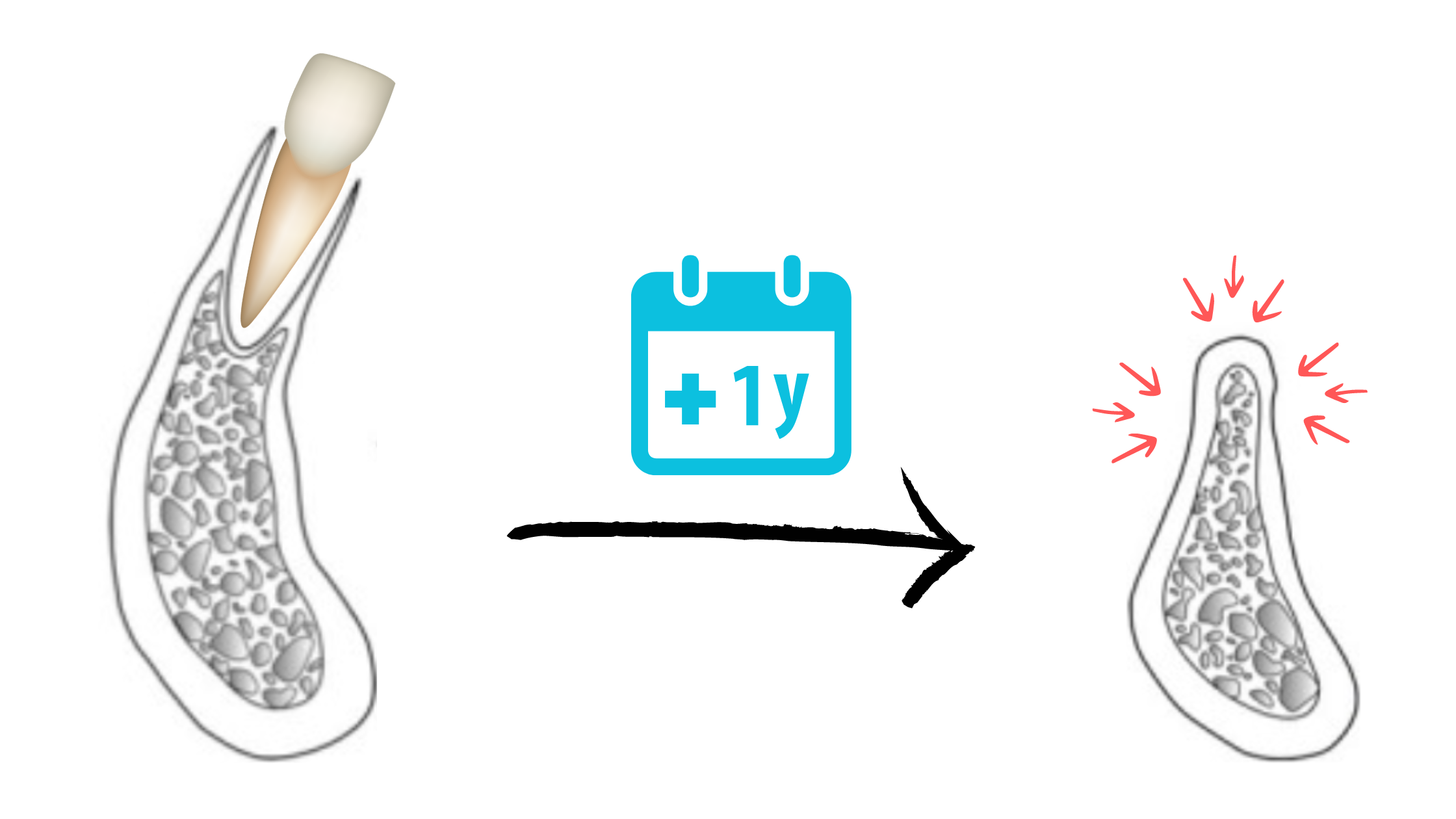
As soon as a tooth is lost, the jawbone no longer receives stimulation to maintain its shape and volume, and it begins to shrink.
Bone loss happens quickly: about 32% of width can be lost within 3 months, and 29–63% within 6–7 months. After that, bone continues to resorb more slowly over the following years.
This rapid bone loss can be reduced with socket preservation, where a bone graft is placed in the socket immediately after extraction.
Replacing the missing tooth with an implant as soon as possible is the most effective way to maintain bone stimulation and prevent collapse.
Teeth Shifting
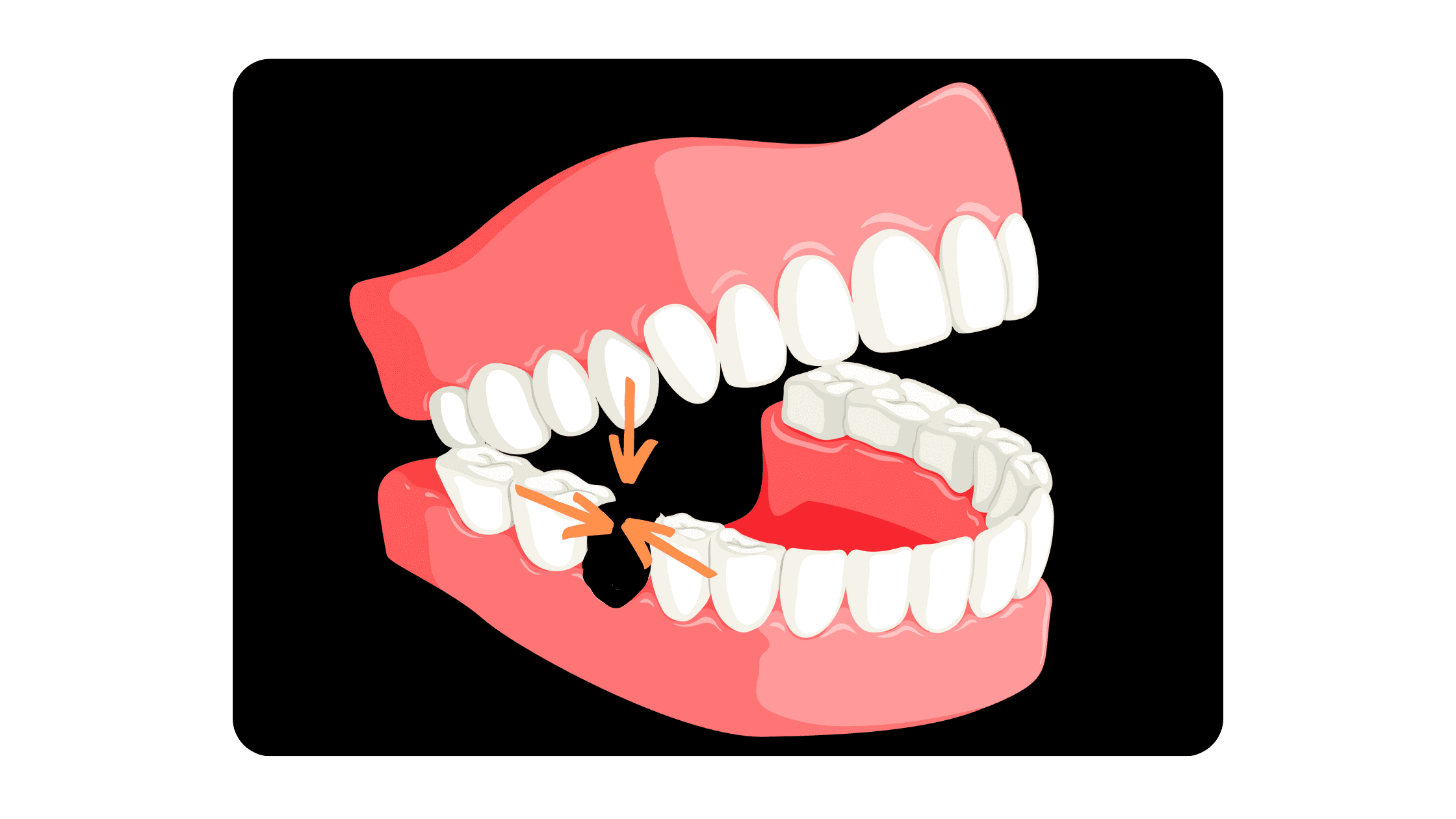
Teeth naturally HATE gaps and always tend to move toward contact with neighboring teeth.
After an extraction, nearby teeth can drift horizontally into the empty space, while opposing teeth may move vertically to fill the gap. This can lead to bite problems, misalignment, and increase the risk of cavities, gum disease, and jaw or muscle issues.
The best way to prevent this is to replace the missing tooth promptly. Alternatively, braces can be used to close the gap and stop unwanted tooth movement.
Bone Spur
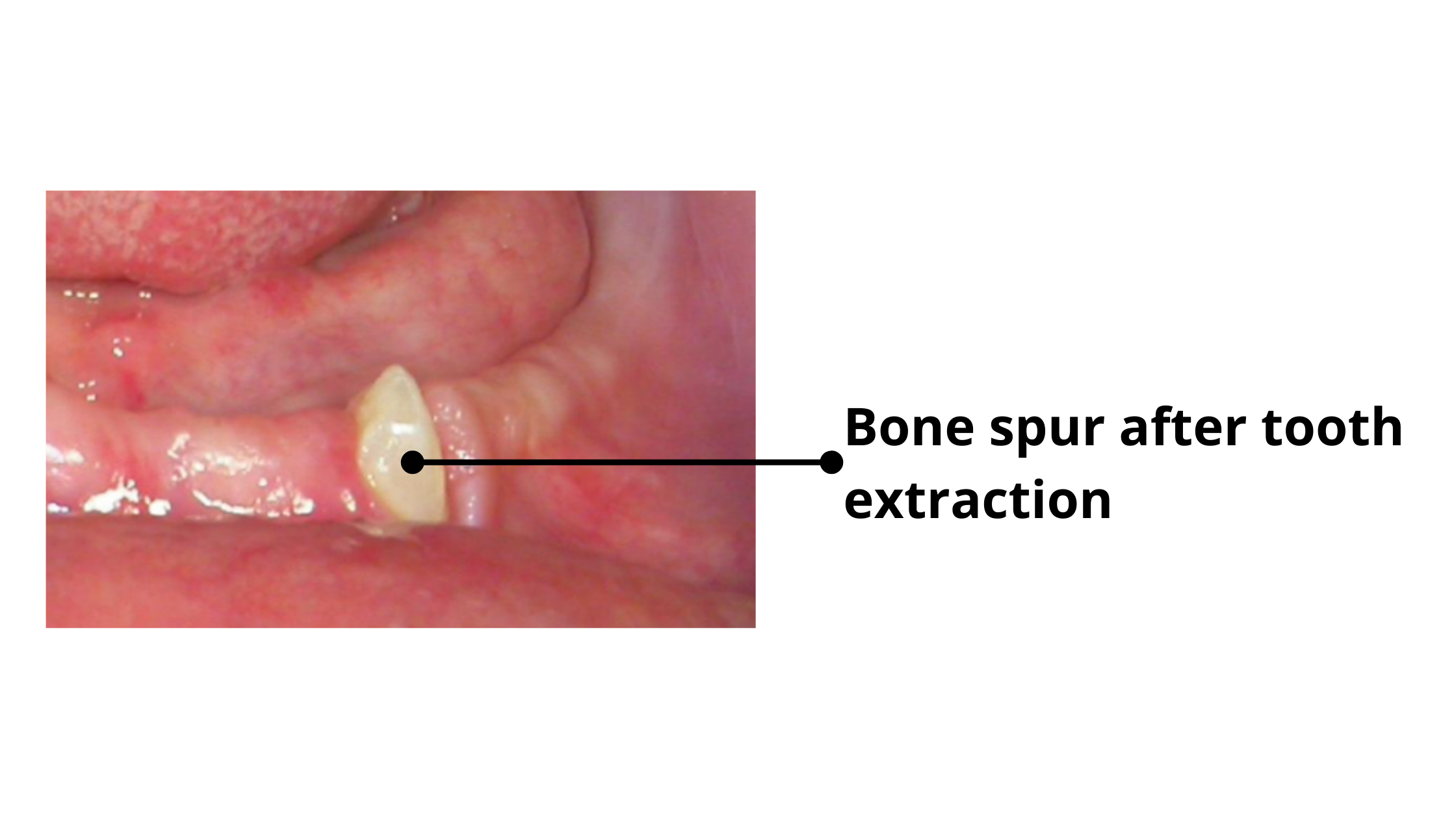
After healing, it’s not uncommon to see a small piece of bone or root fragment emerge from the gums. It may look concerning, but it’s usually harmless.
During the extraction, tiny fragments of bone or tooth roots can sometimes be left behind in the socket. The body treats these as foreign objects and gradually pushes them to the surface through the gum.
When they appear, the surrounding gum may look red, swollen, and feel tender. Most of the time, these fragments come loose on their own or can be easily removed.
Cysts and Tumors
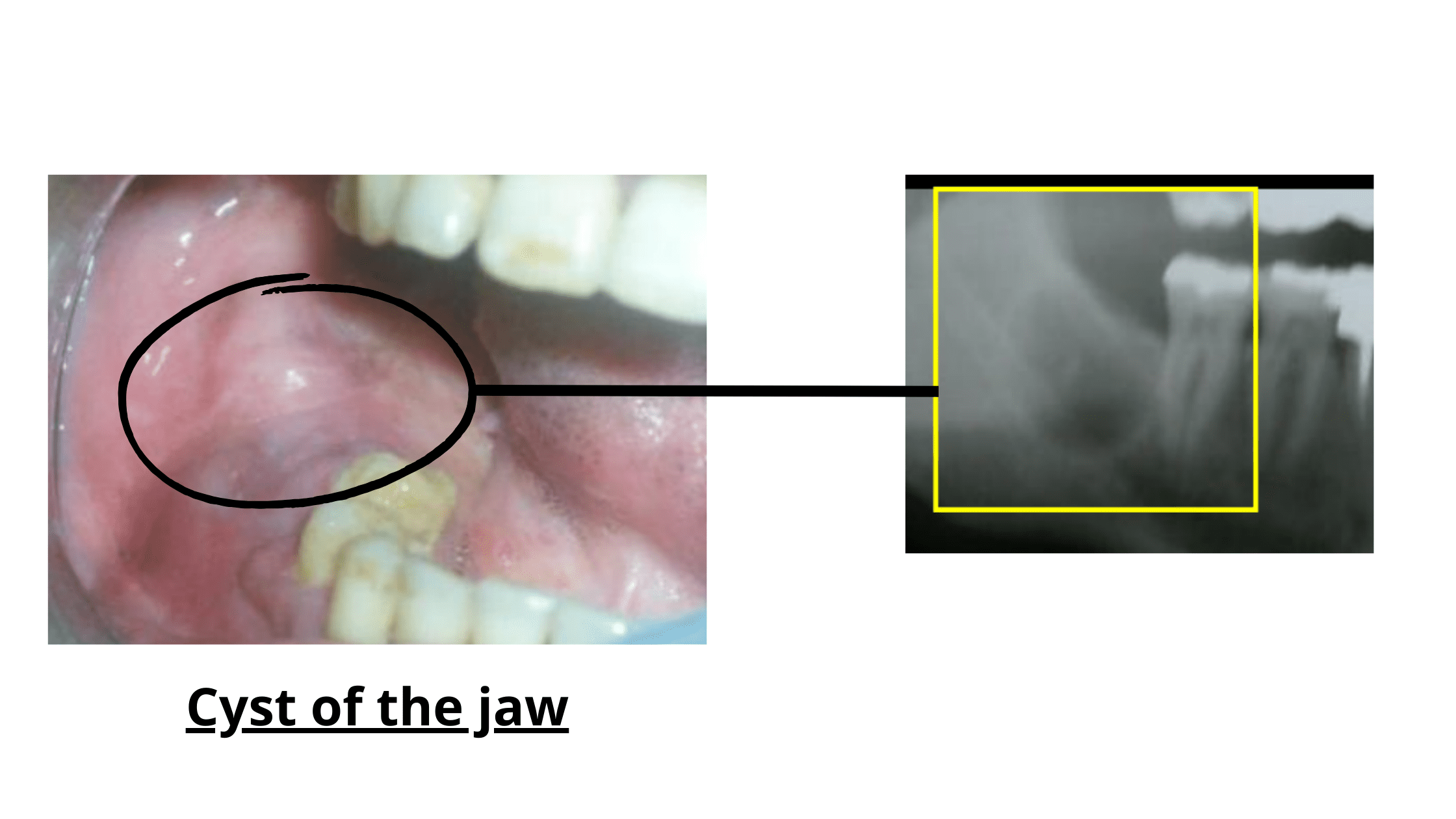
Cysts and tumors are two different types of abnormal growths. Cysts are cavities lined with cells and filled with fluid or other substances from the body. Tumors, on the other hand, result from abnormal cell growth.
Both cysts and tumors of the jaws are uncommon and usually benign (non-cancerous) conditions that can quietly progress without showing any noticeable symptoms.
They are often associated with impacted wisdom teeth (those embedded in the jawbone). Studies show that about 2.24% are linked to cysts and 1.16% to tumors.
If the abnormal growth is overlooked during the tooth extraction procedure, it will persist and continue to grow in the following months and years, leading to further symptoms.
Even if treated initially, there's a small chance it might come back, especially if the treatment isn't complete or if there's debris left in the surgical site.
Factors that Increase the Risk of Complications
Tooth extraction is usually routine and low-risk, but some factors can raise the risks. These include:- Procedure Complexity: Longer or more complicated extractions—like impacted teeth or those requiring bone removal—carry higher risks of complications, such as dry socket, infections, and more pain.
- Dentist’s Experience: Fully erupted teeth are usually easy to extract, but deeply impacted teeth, unusual root shapes, or teeth close to nerves may require some experience.
- Medical Conditions: Patients with weakened immune systems—due to diabetes, long-term corticotherapy, or cancer treatments (radiotherapy and chemotherapy)—are at higher risk of infections. Antibiotics may be prescribed before the procedure to prevent such risks.
- Following Postoperative Advice: Following your dentist’s or surgeon’s instructions is essential for a smooth and successful recovery. Below are some postoperative tips and recommendations.
Ensure a Smooth Recovery
On the Day of the Procedure:
- Numbness: When you return home, your mouth may feel numb for a few minutes. Avoid biting your lips or tongue during this time. Once the numbness wears off, pain will peak in the first few hours. You can manage any discomfort with painkillers as directed by your dentist.
- Bleeding: Your dentist will provide you with clean gauze pads to bite down on for 30 minutes. This will help stop or manage bleeding. If bleeding starts again, use a fresh, clean compress and repeat the process.
- Reduce Swelling: Apply ice to the cheek near the extraction site for 20 minutes every hour. After the initial 24 hours, switch to warmth, as cold is no longer effective.
- Oral Hygiene: Brush and floss your teeth as usual, staying away from the extraction site. If flossing feels uncomfortable, skip it until the area begins to heal. Starting from the second day, rinse your mouth several times a day with warm salt water to support healing and prevent infection.
- Diet: Stick to soft, lukewarm foods and avoid hot, spicy, or acidic items. Chew on the opposite side for the first few days, and gradually return to your regular diet as soon as you feel able to do so.
- Physical Activity: Limit physical activity in the first 24 hours. Sleeping with your head slightly elevated can help prevent bleeding.
- Prescription Medication: Follow your dentist's prescription carefully to manage pain and inflammation and reduce the risk of postoperative infection.
Don'ts After Tooth Extraction
- Do not smoke, rinse vigorously, or use a straw during the first three days. These can dislodge the blood clot and cause dry socket.
- Do not touch the wound with your tongue or finger.
- Avoid alcohol, hot, spicy, or hard foods and drinks.
- Do not chew on the side of the extraction.
- Avoid strenuous activity on the first day.
- Do not brush or floss near the extraction site for the first 72 hours.
The Next Days Until Full Recovery
- Rinse your mouth with lukewarm salt water three times a day (1/2 teaspoon of salt in a cup of water).
- Brush and floss daily, avoiding the extraction area for the first 72 hours.
- Stay away from hard and sticky foods like nuts, almonds, and popcorn.
- Bruising and difficulty opening your mouth may occur, but they should -improve within the first week.
- If you notice increasing pain, fever, nausea, bleeding, or severe swelling, contact your dentist promptly.
Takeaway
Tooth extraction, like any surgery, can cause mild side effects, such as pain, swelling, bruising, and bleeding. These are temporary and manageable at home.Serious complications—like heavy bleeding, infection, dry socket, or damage to nearby teeth—are rare. If you notice anything suspicious, like severe pain that doesn’t improve with painkillers or swelling and bruising that worsen, don't wait to contact your dentist. Early treatment is easier and more effective, and can spare you a long, painful recovery.
- Adverse effects following dental local anesthesia: a literature review - PMC (nih.gov)
- Les complications de l’anesthésie locale en odontologie | Dossiers du mois (lecourrierdudentiste.com)
- Side effects and complications associated with third molar surgery - PubMed (nih.gov)
- Intraoperative accidents associated with surgical removal of third molars (bvsalud.org)
- Complications of Third Molar Extraction - PMC (nih.gov)
- The most common complications after wisdom-tooth removal: part 1: a retrospective study of 1,199 cases in the mandible - PubMed (nih.gov)
- Dry Socket: Incidence, Clinical Features, and Predisposing Factors - PMC (nih.gov)
- Subcutaneous emphysema during mandibular wisdom tooth extraction: Cases series - PMC (nih.gov)
- Persistent trismus following mandibular third molar extraction and its management: A case report and literature review (spandidos-publications.com)
- Prevalence of cysts and tumors around the retained and unerupted third molars in the Indian population - PMC (nih.gov)
- The incidence of cysts and tumors associated with impacted third molars - PMC (nih.gov)