Socket Infection After Tooth Extraction: What You Should Know
Tooth extraction is a routine procedure, and problems are rare. While some post-operative side effects are completely normal, there are certain signs you should watch out for.
Don’t worry — we’ll break it down for you and help you tell the difference between normal healing and a possible socket infection, so you can better understand what’s really going on.
Don’t worry — we’ll break it down for you and help you tell the difference between normal healing and a possible socket infection, so you can better understand what’s really going on.
In this article:
1. Infection after Tooth Extraction (or Socket Infection): What exactly is it?
2. How to Tell if the Socket is Healing or Getting Infected
3. The Main Features of an Infection After Tooth Extraction
4. What Are the Risks of Having a Socket Infection?
5. When Does a Socket Infection Start and How Long Does It Last?
6. Is It Dry Socket or Socket Infection?
7. Treating Infection After Tooth Extraction
8. What to Do at Home in the Meantime
Infection after Tooth Extraction (or Socket Infection): What exactly is it?
When a tooth is extracted, the empty space left behind is called the socket.Right after a tooth is removed, the socket fills with a blood clot. This clot helps stop bleeding and protects the wound while it heals.
In some unusual situations, the clot can become a breeding ground for bacteria and cause a socket infection. This happens when "BAD" bacteria make their way deep into the wound. The causes can include food getting stuck, a piece of tartar, or even small fragments of tooth or bone left behind during the extraction.
Is it serious?
Usually, no. Most socket infections stay local and clear up with treatment. Your dentist will clean the socket (debridement) and may prescribe antibiotics.
But if left untreated, the infection can spread to surrounding tissues, including the face and jawbone. When the jawbone is affected, it can lead to a serious condition called osteomyelitis.
How to Tell if the Socket is Healing or Getting Infected
The first signs that often raise concern are pain and swelling, which are also normal parts of the healing process.Mild inflammation is expected after any surgery, including a tooth extraction. The resulting swelling and discomfort should gradually improve during the first week.
However, swelling and pain should not worsen over time or suddenly appear days later. If they’re accompanied by any of the following, it could be a sign of infection—and you should see your dentist as soon as possible:
- Pus (a thick yellow or white fluid) leaking from the socket
- Fever
- Swollen lymph nodes
- Bad breath
- A foul taste
Another concerning sign is seeing exposed bone, which may look white or gray.
Normally, you can't see the bone because the socket should be covered by a blood clot.
If the blood clot didn’t form properly or has been lost, it can lead to a painful condition known as dry socket.
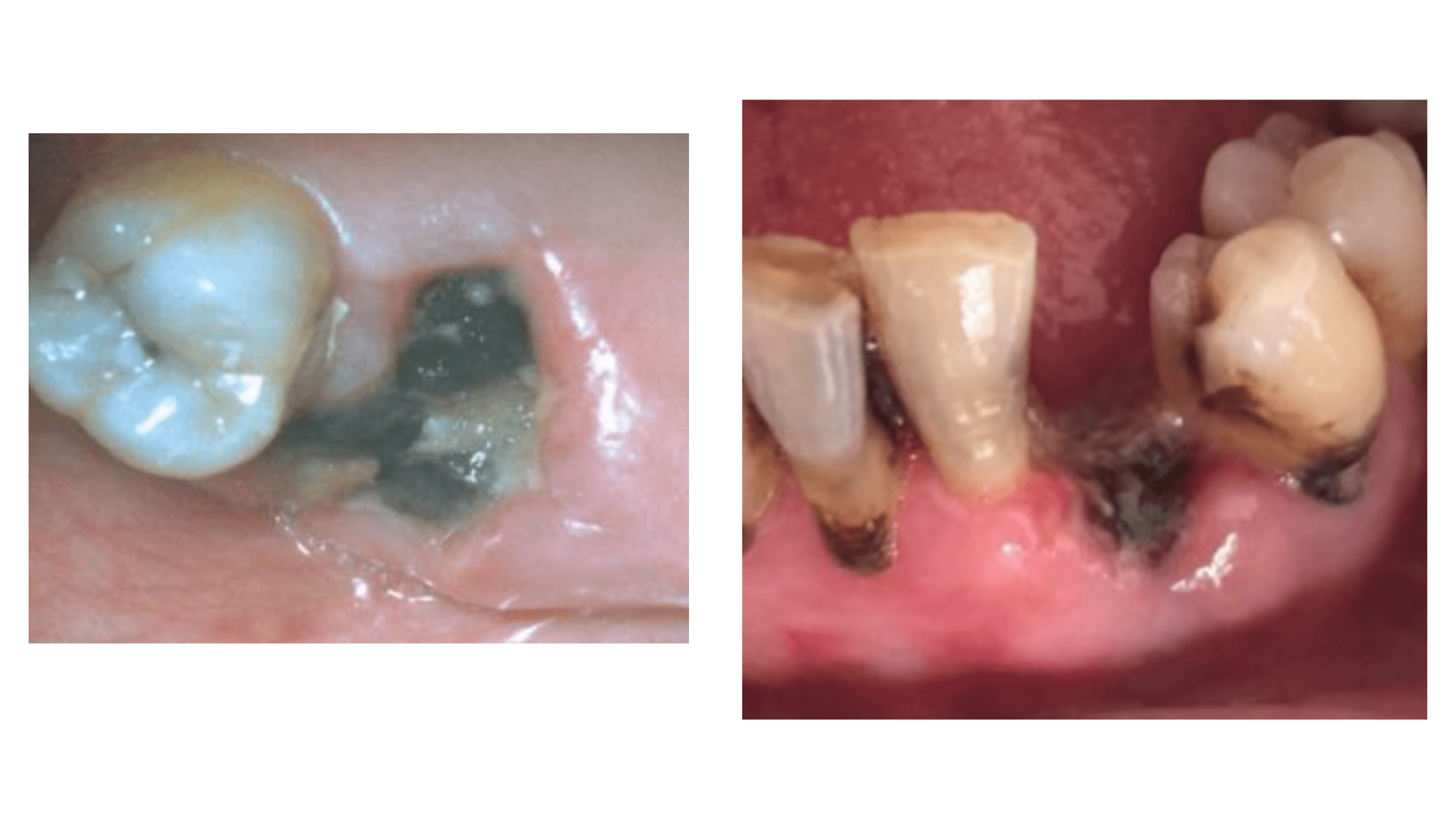
Also, if you notice the socket filled with something unusual — like a black or brown substance instead of a normal blood clot (as shown in the pictures above) — and you have other symptoms (like extreme pain or bad breath), talk to your dentist right away.
The Main Features of an Infection After Tooth Extraction
Socket infections have their own features that can help you spot them early. Here's what you should know:- The Pain: Typically intense and throbbing, and it gets worse if you touch the area with your tongue or finger. It can start on the same day of the procedure or a few days later.
- Socket Appearance: Covered by a brown or black substance, often with pus oozing.
- Gum Tissue Surrounding the Socket: Appears red, swollen, and tender.
- Systemic Signs: General signs include fever, tiredness, and swollen lymph nodes under the lower jaw.
- Additional Symptoms: Infection may cause bad breath, a bad taste, and difficulty opening the mouth.
What Are the Risks of Having a Socket Infection?
The risk of infection after a tooth extraction is quite low. In a study of 1,821 extracted teeth, only 25 cases (1.4%) developed postoperative infections. Many factors affect this risk, but the most common cause was complex procedures.Complex procedures are those that take longer and involve bone drilling.
Teeth that are impacted (embedded within the jawbone) are usually harder to remove than regular teeth.
While you can’t control the difficulty of the procedure, you can reduce your risk by carefully following your dentist’s postoperative instructions.
Actions like eating hard or crunchy foods, or rinsing and spitting forcefully during the first few days, can disrupt the blood clot too early. This can expose the socket and increase the chance of infection.
When Does a Socket Infection Start and How Long Does It Last?
Infections after tooth extraction usually begin within the first few hours or days following the procedure.The first signs include severe pain and an unusual appearance of the socket. Unlike normal healing, the pain lasts much longer and can continue for more than two weeks.
A socket infection cannot heal on its own. If left untreated, bacteria can spread to the facial tissues (causing cellulitis) or into the jawbone (causing osteomyelitis).
Since bone cannot stretch, pus and swelling inside the jawbone can press on nearby blood vessels and block blood flow. This means part of the bone may not receive enough blood and can die.
If this continues, it can cause severe bone loss and deformities of the jawbone. That’s why early treatment is crucial to prevent these serious complications.
Is It Dry Socket or Socket Infection?
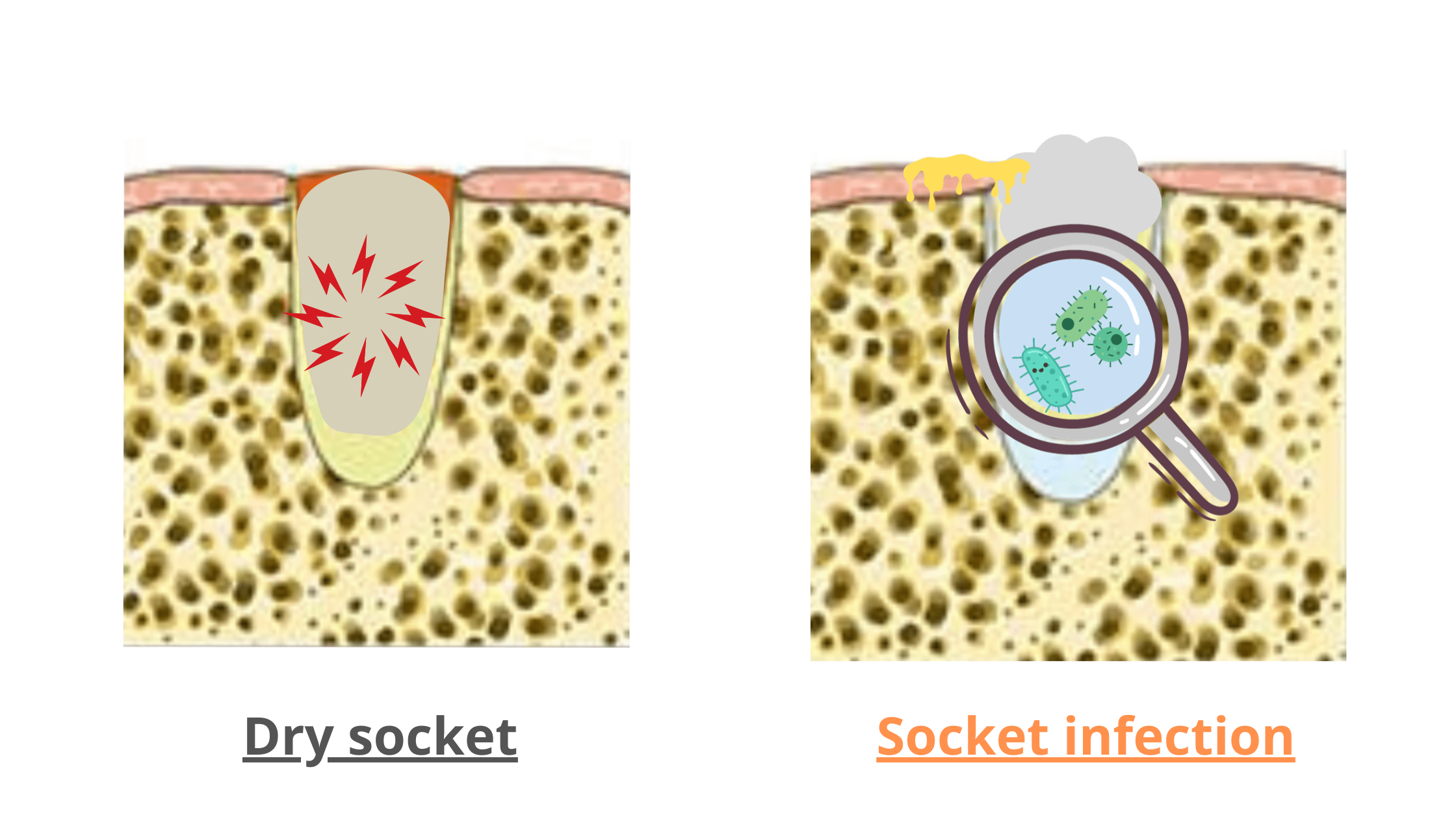
Dry socket is the most common post-extraction complication. It may seem like an infection, but it doesn't involve bacteria. Instead, it happens when the blood clot breaks down or is lost too soon, exposing the bone and nerves to the mouth, which can delay the healing process.
Dry socket typically starts 2 to 4 days after the procedure, causing severe throbbing pain that can spread to the jaw and face. Unlike infections, dry socket typically gets better on its own within 15 days.
Main Differences Between Dry Socket and Socket Infection:
- Dry Socket Appearance: Empty socket with noticeable whitish bone walls.
- Pus and Other Symptoms: Dry socket doesn’t cause pus, fever, or tiredness.
- Pain in Dry Socket: More intense, and doesn’t always need touching to get worse.
- Healing: Dry socket often resolves itself without treatment.
Treating Infection After Tooth Extraction
Dental infections of any kind should never be ignored. Don’t wait to see your dentist—an infected socket won’t heal on its own and will only get worse over time.The steps for treating infection after tooth extraction usually involve:
- Dental Examination: Your dentist will examine the area and may take X-rays to check for any debris or tooth fragments left inside the socket.
- Cleaning Procedure: The dentist will numb the area and clean the socket to remove food buildup and the infected blood clot. Then, they’ll flush the area with an antiseptic solution to kill bacteria and cover the socket with a soothing medicated dressing to help it heal.
- Medications: Your dentist may prescribe antibiotics and painkillers to eradicate the infection effectively.
What to Do at Home in the Meantime
While waiting for your dental appointment, there are things you can do at home to ease discomfort and prevent the infection from getting worse:- Over-the-counter painkillers: Take over-the-counter painkillers as directed. While they can relieve pain, that doesn’t mean they are a treatment on their own.
- Saltwater Rinse: Mix half a teaspoon of salt in a cup of lukewarm water and gently rinse your mouth several times.
- Diet: Avoid chewing on the infected side of your mouth and steer clear of hard, crunchy, and spicy foods to avoid irritating the wound and causing discomfort.
- Prevalence of Postoperative Infection after Tooth Extraction: A Retrospective Study - PMC (nih.gov)
- Alveolar Osteitis - StatPearls - NCBI Bookshelf (nih.gov)
- Essential Of Oral Pathology - Book by Swapan Kumar Purkait