Dry Socket: The Most Common Complication After Tooth Extraction
 After tooth extraction, especially in more complex procedures, experiencing some discomfort and swelling is expected. However, what happens when you find yourself on the road to recovery, and suddenly, a throbbing pain sets in? Well, that might be a sign of something called dry socket.
After tooth extraction, especially in more complex procedures, experiencing some discomfort and swelling is expected. However, what happens when you find yourself on the road to recovery, and suddenly, a throbbing pain sets in? Well, that might be a sign of something called dry socket.
In this article, we'll explore what dry socket is, how it happens, and most importantly, how to prevent and treat it.
In this article:
1. What is Dry Socket?
2. How Does Dry Socket Occur?
3. The Symptoms of Dry Sockets
4. How Does Dry Socket Show Up on X-Rays?
5. Is it Dry Socket or an Infection?
6. Does Dry Socket Require Prompt Treatment?
7. Dos After Tooth Extraction:
8. Don'ts After Tooth Extraction:
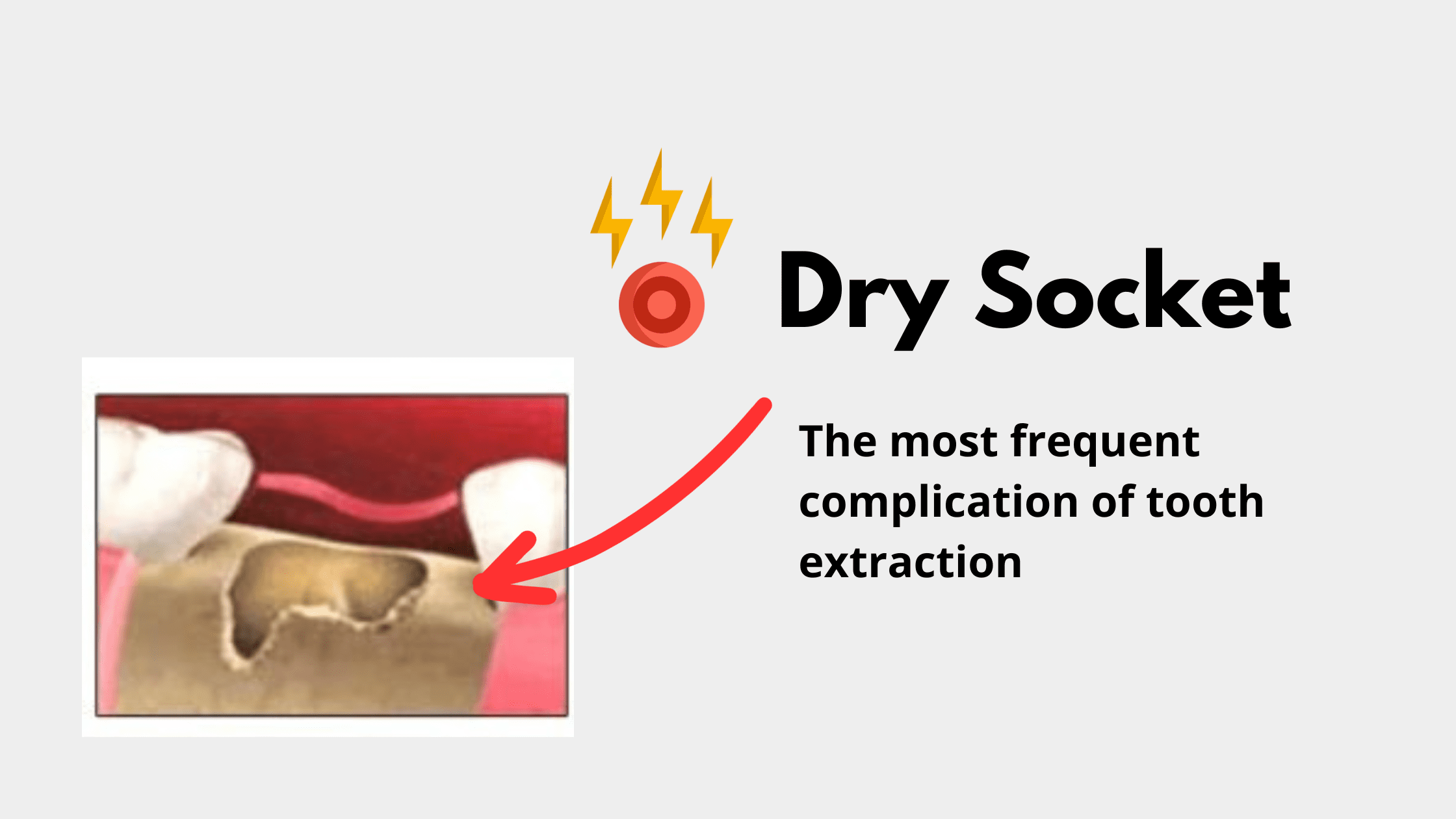
What is Dry Socket?
Dry socket or medically termed "alveolar osteitis" is the most common postoperative complication after tooth extraction. It refers to the inflammation of the socket, the bony cavity that holds the tooth in place.When your tooth is removed, a protective blood clot forms in that socket. This clot shields the wound, nerves, and bone underneath it. Sometimes this clot doesn't form properly or gets dislodged, exposing the bone and nerves to things like food, air, and saliva. This leads to intense inflammation and severe, constant pain.
How Does Dry Socket Occur?
Dry socket occurs when that protective blood clot is either lost too early or doesn't form at all. That blood mass is essential for a normal healing process. It stops bleeding, keeps infections away, and enhances cell migration and growth. So, losing it too soon means slower recovery and more pain.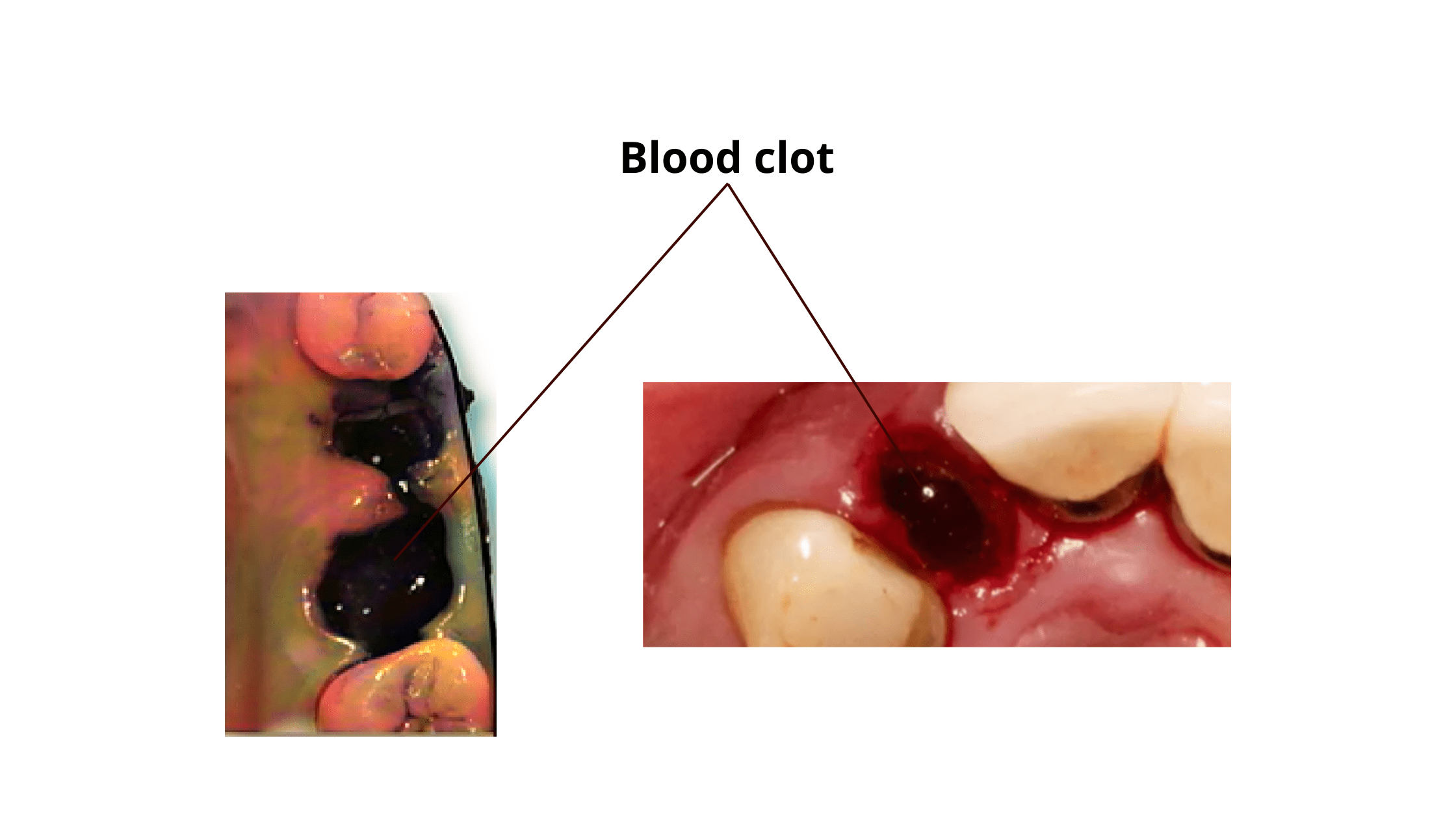
How does dry socket occur in the first place? Several factors are involved, some you can control while others you can't.
The first 48 hours after extraction are crucial. Be gentle with the wound – no smoking, no rinsing your mouth, and definitely no poking at the socket. Get plenty of rest and don't stress, as high cortisol levels can mess with your clotting process.
Factors you can't control include the complexity of the procedure and the tooth's location. The teeth of the lower jaw, especially the wisdom teeth are more prone to this complication due to less blood supply there.
Dry socket can also be due to a body process called fibrinolysis. There are different reasons for this. Some think that oral bacteria release enzymes that can break down the blood clot. That's why having a mouth infection, such as gum disease or abscess before the procedure increases your risk even more. Other things that can trigger fibrinolysis include smoking and using oral contraceptives.
The Symptoms of Dry Sockets
Like any surgical procedure, tooth extraction comes with some post-operative side effects. While mild, temporary discomfort is completely expected, the pain caused by dry socket is often something far more severe.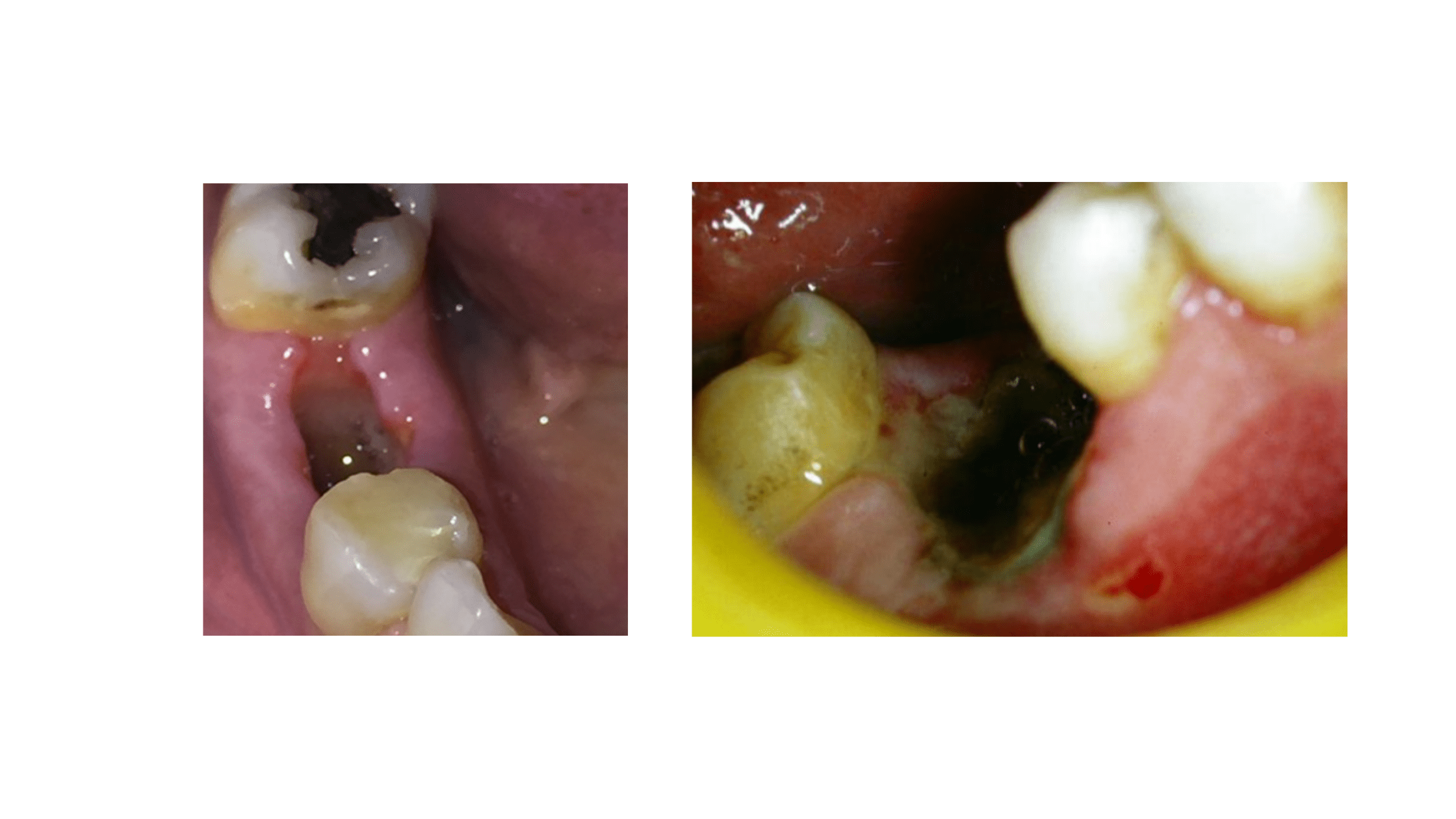
Here's what you need to know:
- When it Starts: Typically, dry socket kicks in on the second or third day after the procedure.
- Pain Intensity: While normal post-extraction pain should gradually decrease, dry socket pain is different. It hits suddenly and can be so intense that it might keep you up at night. Even over-the-counter painkillers might not do much.
- Duration: Dry socket can persist for about a week, but in some cases, the pain lingers for weeks.
- Socket Appearance: When you look at the socket, you'll notice the bone walls underneath. They appear greyish-white and are super sensitive to even the slightest touch.
- Gum Tissue: The surrounding gum tissue is often inflamed, tender, and swollen. Sometimes, it may even grow over the socket completely.
- Other Symptoms: Dry socket can come with bad breath. Less commonly, you might notice a swollen lymph node under your lower jaw or on your neck.
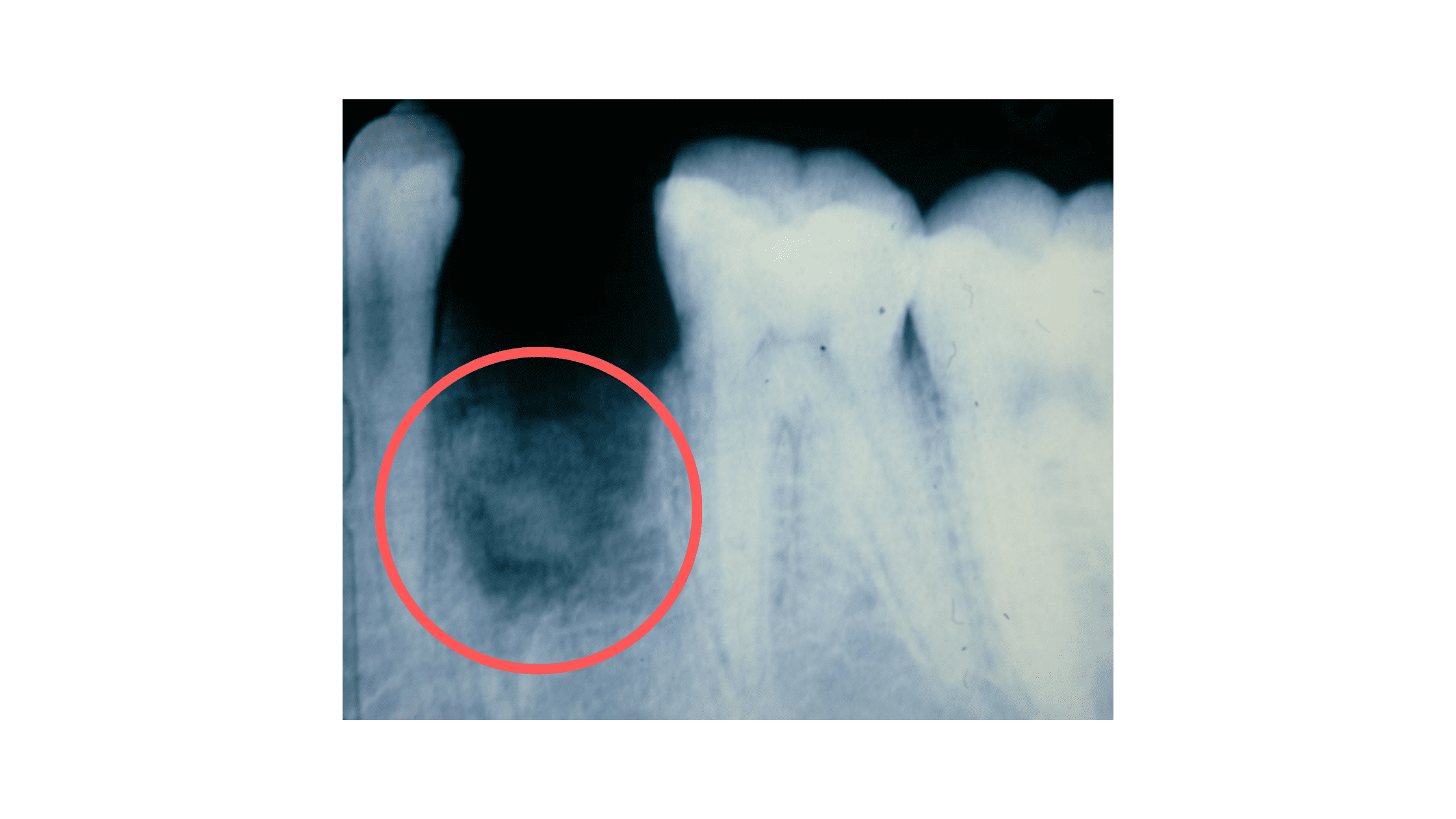
How Does Dry Socket Show Up on X-Rays?
There aren't any specific features that show up in X-rays. What we do notice is an empty socket that just doesn't seem to heal, even after weeks.On the X-ray below, you can see a dark area in the empty socket, indicating that the bone has not regenerated due to delayed healing.
Is it Dry Socket or an Infection?
Dry socket and infection are two different complications. Dry socket isn't a true infection; it's more like an intense inflammation that delays healing.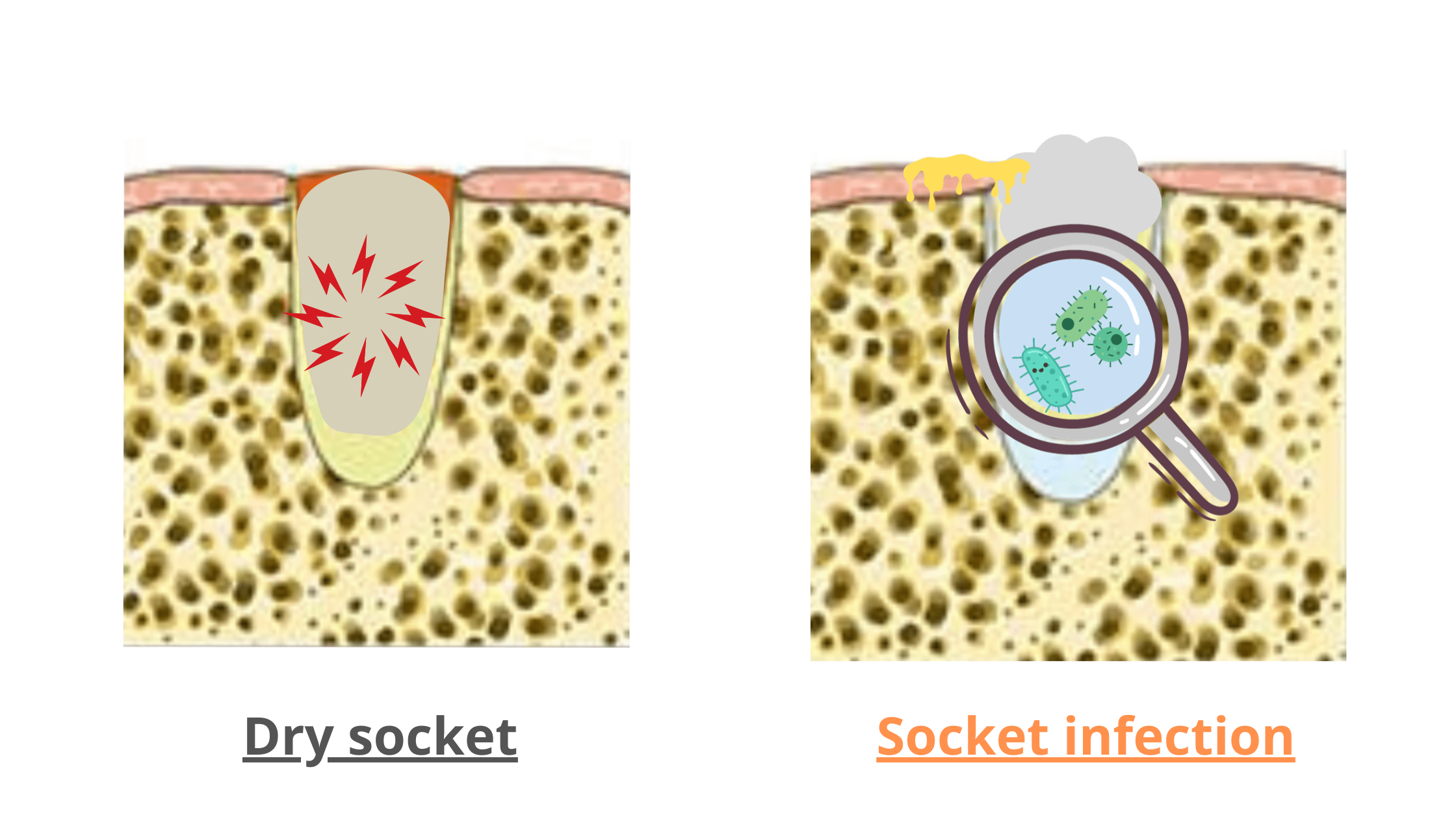
Socket infection, on the other hand, has its own causes and features. It happens when "BAD" bacteria invade the blood clot and underlying bone. This may be due to tartar or a food particle stuck in the wound.
Here's how to tell them apart:
- With infection, pain often shows up quickly from day one. It isn't as intense as dry socket pain.
- The socket might be filled with white stuff, a mix of dead tissue and food debris, with pus leakage.
- You might notice swelling, bad breath, foul taste, and even a fever with an infection.
- If not treated promptly, infection can lead to bone death (necrosis), which can result in a piece of bone coming out.
Does Dry Socket Require Prompt Treatment?
If left untreated, dry socket will eventually heal, but it'll be a slow and incredibly painful process. So it's best to treat it quickly to spare yourself any suffering.The goal of treatment is to reduce pain and restart the normal healing process.
Here's how your dentist can help:
- Under local anesthesia, your dentist will rinse the empty socket with an antiseptic, clean it up, and gently scrape it to promote fresh blood clot formation.
You must avoid anything that might disturb the clot to prevent dry socket from coming back. - Your dentist will apply a gauze or dressing with soothing medication to the clean socket. This dressing should be changed every 48 hours until you are healed.
- Your dentist may also prescribe painkillers and anti-inflammatory drugs. Antibiotics may be needed only if there's an infection.
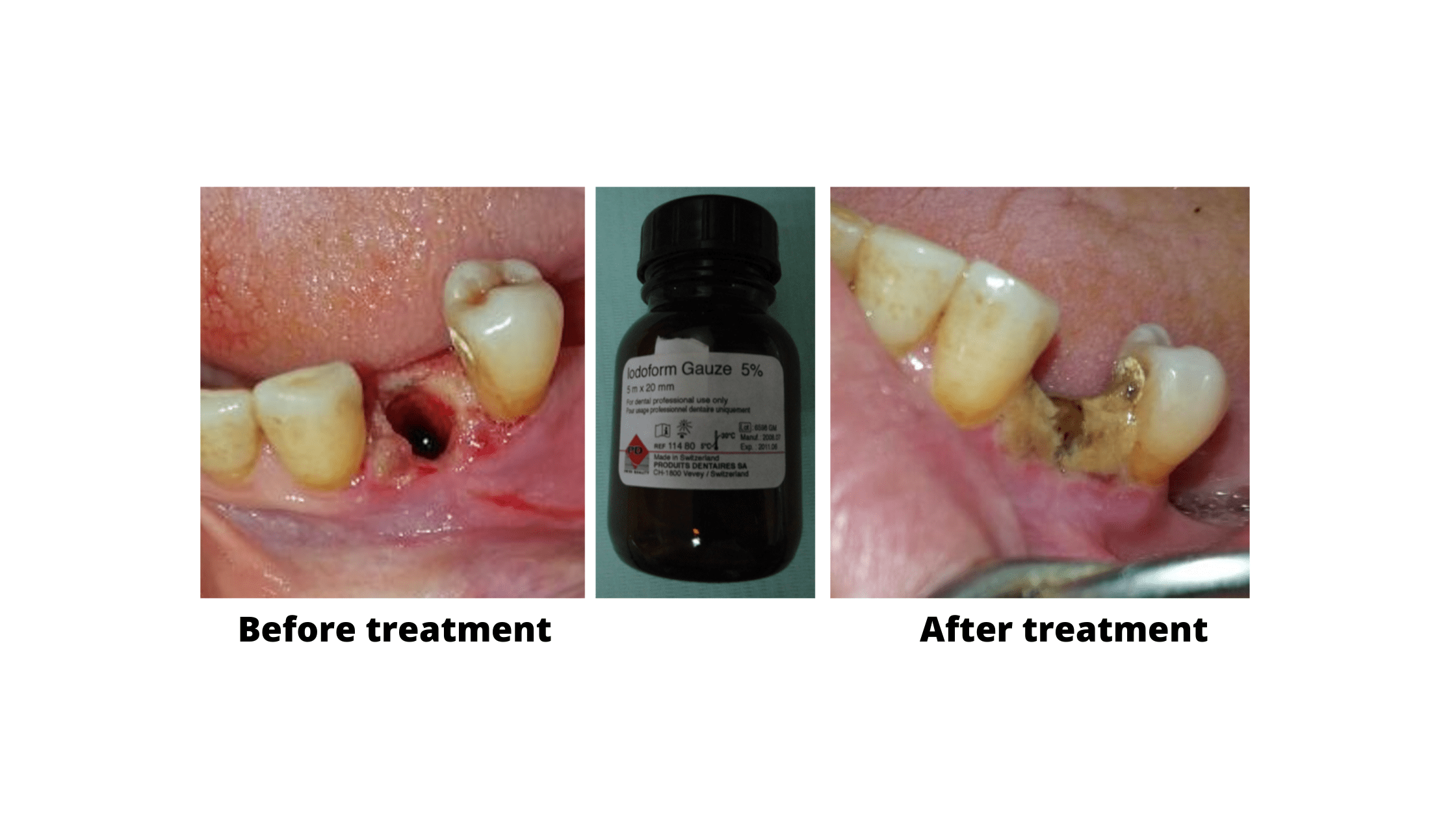
After treatment, you'll feel immediate relief. If the pain persists, see your dentist again. There could be a deep bone infection or something stuck in the socket that only an X-ray can reveal.
To make your treatment effective, you need to follow the post-operative instructions carefully. Below are the do's and don'ts after a tooth extraction.
Dos After Tooth Extraction:
- Take Prescribed Medications: Use pain relievers, antibiotics, or other medications as prescribed by your dentist.
- Maintain Gentle Oral Hygiene: Brush your teeth gently while avoiding the extraction area in the first two days.
- Rinse with Warm Saltwater: After 24 hours, rinse your mouth gently with warm saltwater.
- Eat Soft, Nutrient-Rich Foods: Consume foods like yogurt, mashed potatoes, and smoothies to promote healing and stay away from hot, spicy, and crunchy foods.
- Rest: Rest well and don't stress to support your body's healing process.
Don'ts After Tooth Extraction:
- Don't Smoke: Smoking narrows blood vessels and increases complications.
- Don't Use Straws: Suction from straws can dislodge the blood clot and lead to dry socket.
- Avoid Touching the Site: Leave the wound alone and don't try to touch it with your fingers or tongue, especially in the first 48 hours.
- Don't use alcohol-based or strong mouthwashes: These can irritate the wound. Salt water rinse is effective and safer.
- No Rinsing Vigorously: Avoid rinsing or spitting forcefully for 24 hours after extraction.
- Don't Strain Yourself: Avoid strenuous physical activities and heavy lifting to prevent bleeding.
- Essential Of Oral Pathology - Book by Swapan Kumar Purkait
- Alveolar Osteitis - StatPearls - NCBI Bookshelf (nih.gov)
- Complications post-opératoires des avulsions complexes: prévention et prise en charge (cnrs.fr)
- BUPHA_TD_2020_RAVEL_VALENTIN.pdf (univ-lorraine.fr)