My Sinus Is Perforated After a Tooth Extraction: Telltale Symptoms and Risks
One of the major complications following extraction of the back teeth of the upper jaw is perforation and exposure of the sinuses.
The close connection between these structures often leads to sinus issues following dental work on these teeth. The good news is that these problems are usually temporary, and there's a good chance they'll resolve on their own.
In this article, we'll delve into sinus perforation after tooth extraction, discussing its telltale symptoms, risks, complications, and treatment options.
The close connection between these structures often leads to sinus issues following dental work on these teeth. The good news is that these problems are usually temporary, and there's a good chance they'll resolve on their own.
In this article, we'll delve into sinus perforation after tooth extraction, discussing its telltale symptoms, risks, complications, and treatment options.
In this article:
1. Perforated Sinus After a Tooth Extraction: What Does It Mean?
2. The Telltale Symptoms of Sinus Perforation after Tooth Extraction
3. What Does a Sinus Perforation Look Like?
4. How Can the Dentist Tell if the Sinus is Perforated?
5. How Does a Perforated Sinus Look Like on X-rays?
6. Potential Complications of Perforated Sinus after Tooth Extraction
7. The Different Treatment Options for Sinus Perforation
8. Post-Surgical Care: Ensuring a Smooth Recovery
Perforated Sinus After a Tooth Extraction: What Does It Mean?
A sinus perforation is one of the most common complications after removing upper back teeth. It can occur in up to 11% of cases.This happens when an unintended opening (or hole) forms in the thin bone that separates your upper back teeth from the maxillary sinuses. But what exactly are the maxillary sinuses, and how are they connected to your upper teeth?
What Are the Maxillary Sinuses?
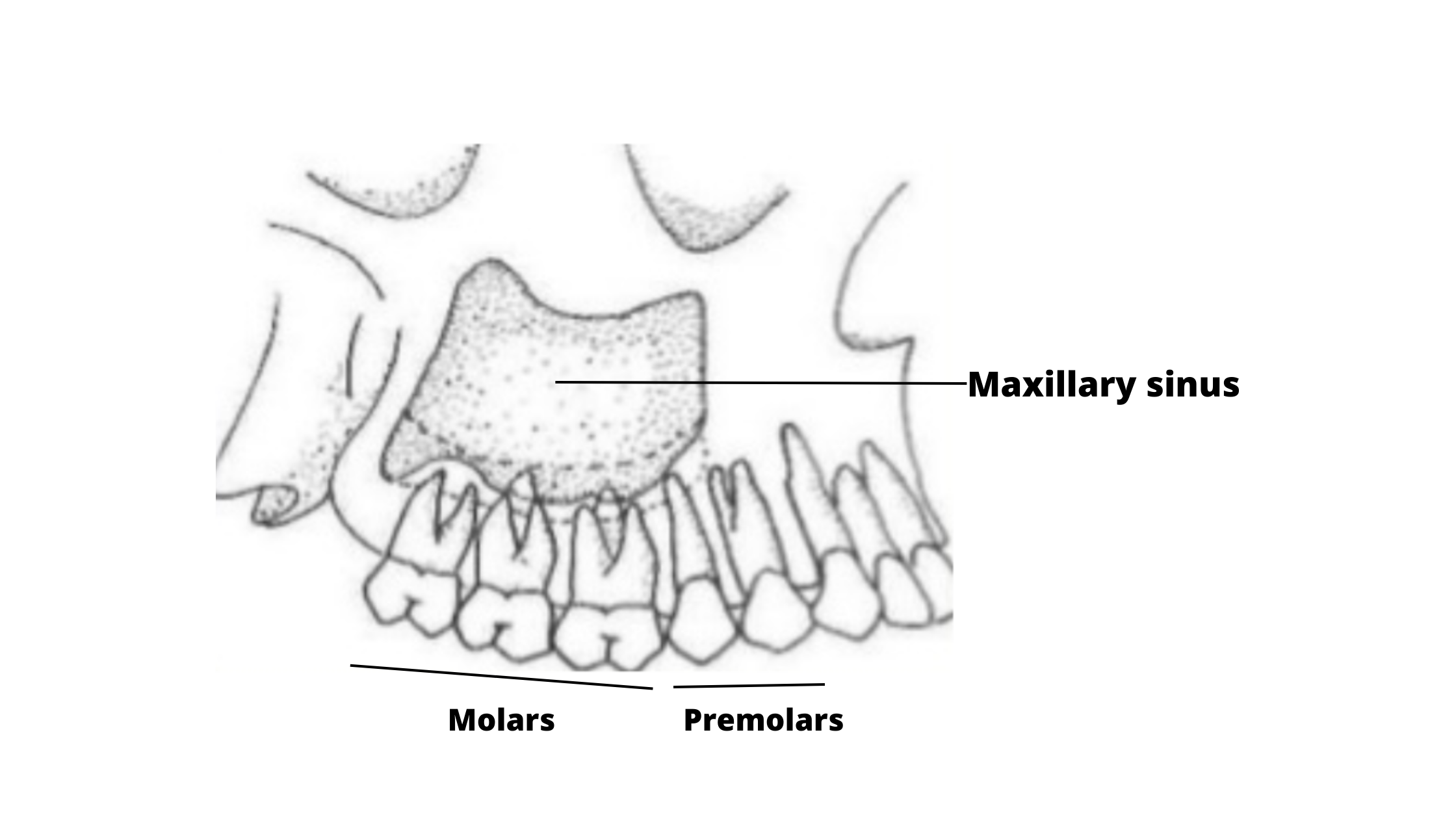
The maxillary sinuses are two air-filled spaces located in your cheekbones, on either side of your nose. They're named after the maxilla, which is the upper jawbone.
These sinuses are lined with soft tissue that produces mucus—a gel-like fluid that helps moisten and filter the air you breathe. When the lining of the sinus becomes inflamed or infected, it leads to a condition known as sinusitis.
How Are the Sinuses Connected to Your Upper Back Teeth?
The upper back teeth and the maxillary sinuses are like close neighbors. Sometimes, they’re separated by only a thin wall of bone.
When there’s a thick layer of bone between them, the risk of sinus damage during tooth extraction is low.
But in many people, this bone can be very thin or even missing. In these cases, the roots of the upper teeth can extend directly into the sinus cavity, making injuries more likely.
About 10% of sinus infections are caused by dental problems, and many of those come from dental procedures.
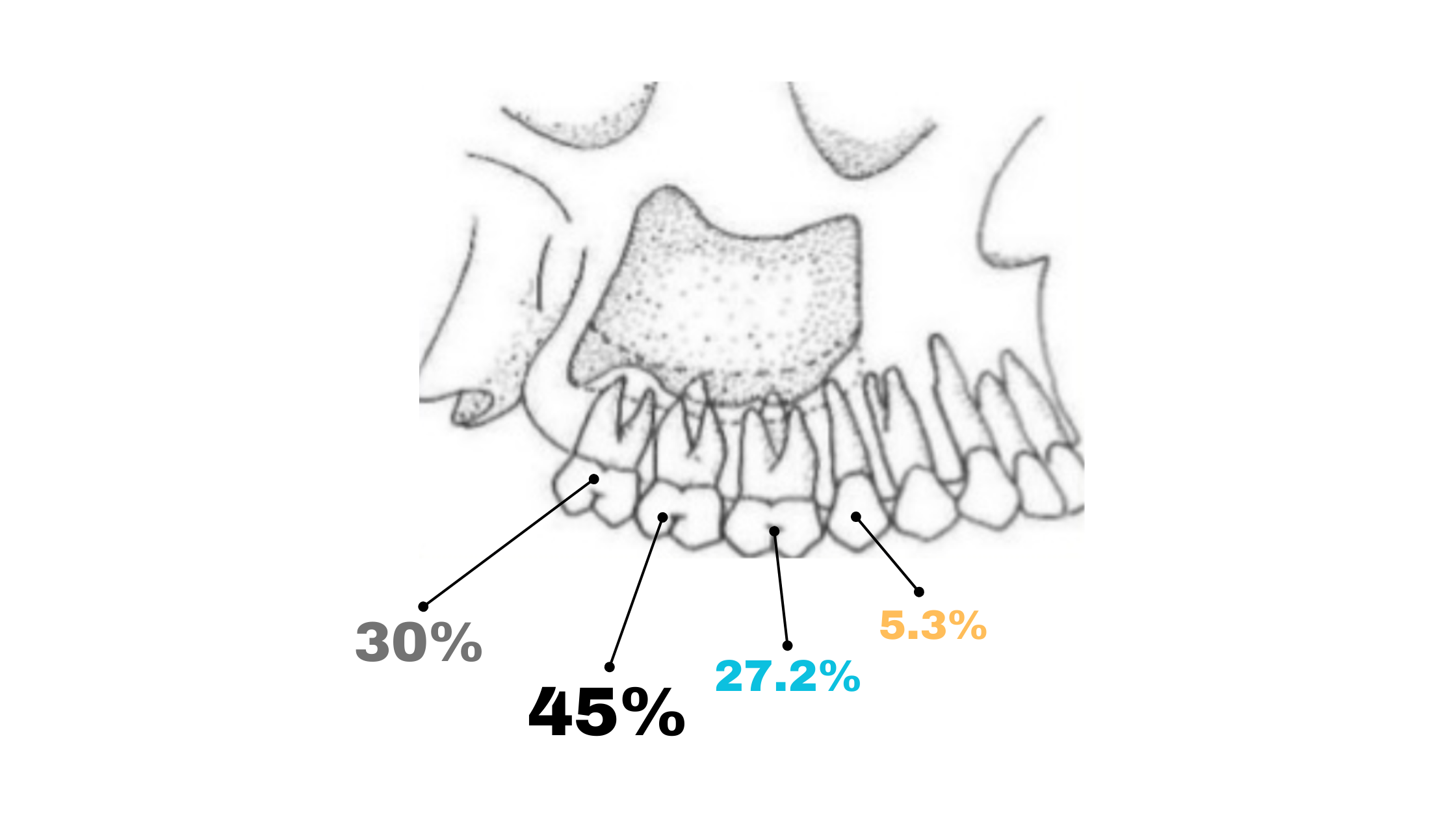
The second molars carry the highest risk for sinus complications, followed by wisdom teeth, first molars, and first premolars.
What Does It Mean When a Sinus Is Perforated?
Healthy sinuses are completely sealed off from the mouth. But when the bone or soft tissue lining is damaged, it can create a small opening. This is called an oro-antral communication, because the sinus can now communicate directly with the mouth.
The most common cause is the extraction of an upper back tooth. But trauma, infections, or even other dental procedures (like root canals) can also lead to this abnormal communication.
What happens when the sinus is perforated?
Most of the time, if the opening is small, it will heal and close on its own within a few days.
But if it’s larger, it might not heal properly, and that’s when problems start.
Saliva, food particles, and bacteria can pass into the sinus, resulting in sinusitis.
The Telltale Symptoms of Sinus Perforation after Tooth Extraction
The symptoms can vary depending on the size of the perforation, how much time has passed since the extraction, and whether there’s an infection.A small perforation may go completely unnoticed right after the extraction — and in most cases, it heals on its own without any issues.
But if the opening is larger, you might experience the following signs:
- Air escaping through the socket when you sneeze or apply pressure
- Bubbles of air or blood coming from the extraction site
- A change in your voice (in more severe cases)
These symptoms suggest that there’s a connection from the sinus down to the mouth.
But the communication can work the opposite way as well, from the mouth up into the sinus. You may notice:
Another telltale sign that the sinus issue is dental-related is that symptoms always appear on just one side of your face (the side where the tooth was removed).
That’s different from sinusitis caused by colds or allergies, which typically affects both sides of the nose and sinuses.
What Does a Sinus Perforation Look Like?
In the early stages, a sinus perforation and the surrounding gums may look completely normal and healthy.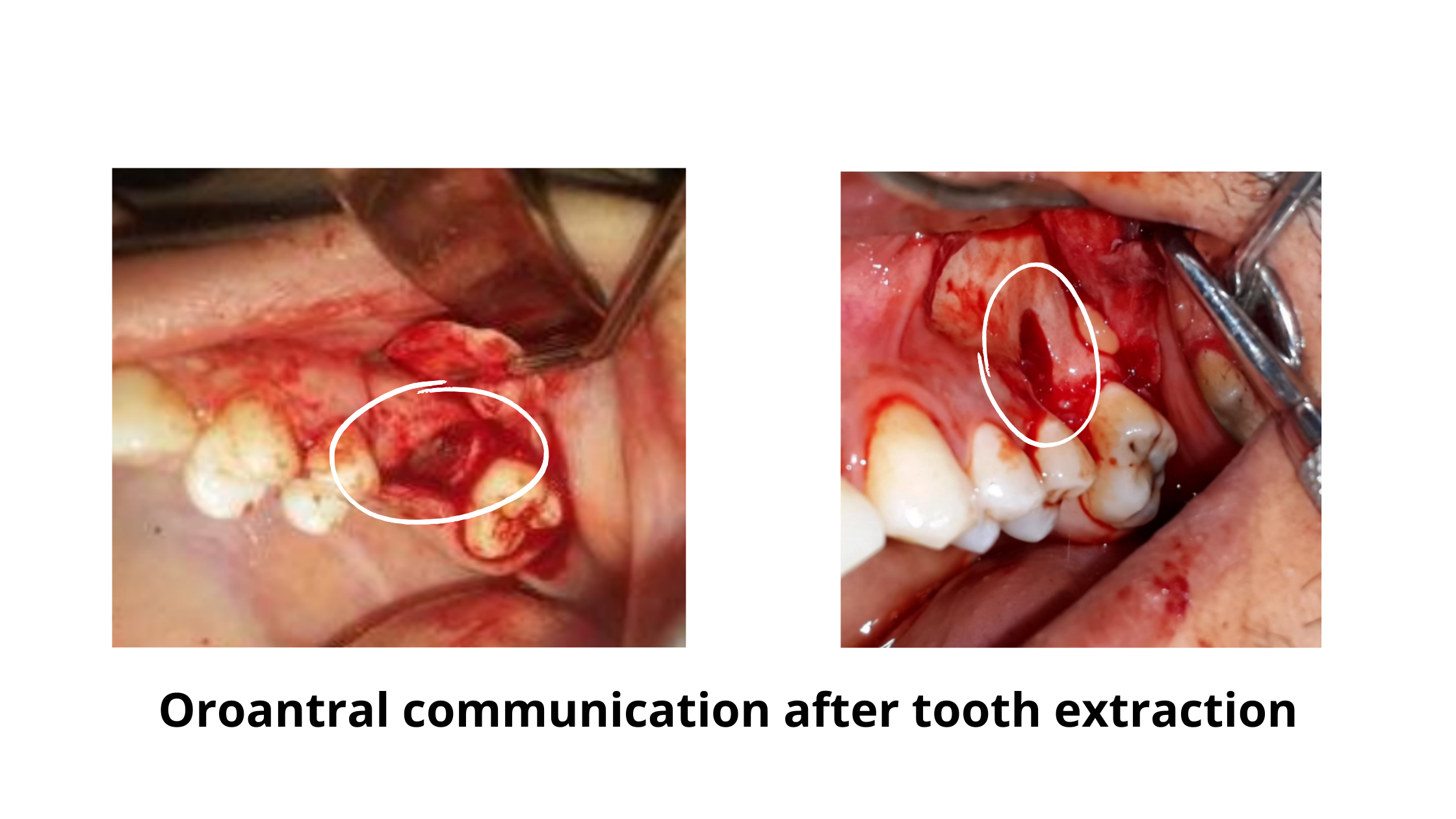
But if the opening doesn’t heal or isn’t treated, the risk of infection increases. It can develop very early, in about 50% of cases within the first 48 hours, and up to 90% within two weeks.
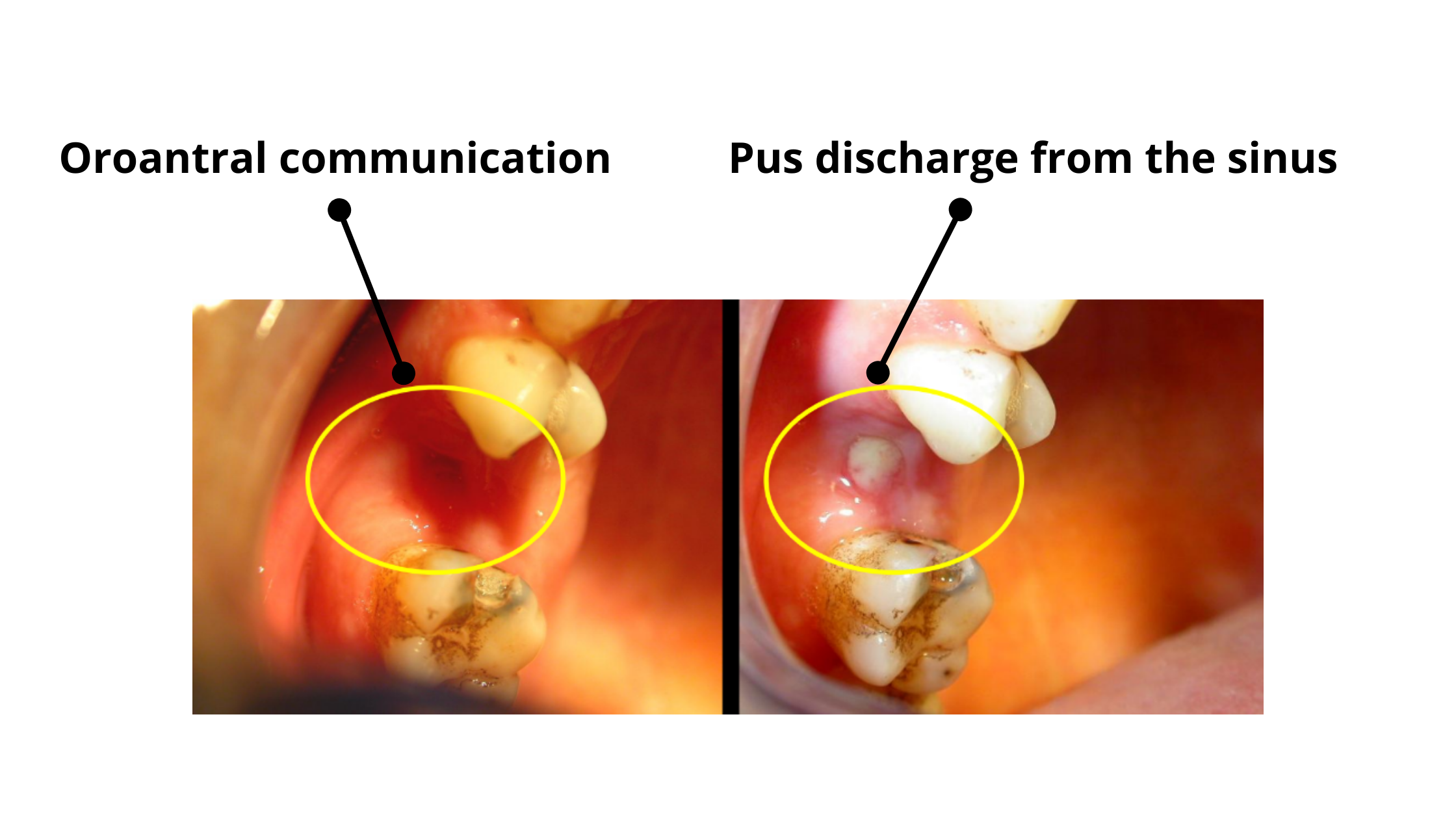
A sinus infection following a tooth extraction will lead to:
- Red, swollen, or inflamed gums around the perforation
- Pus or clear yellow fluid leaking from the site
- Pain and tenderness
- Bad smell or taste in your mouth
- Runny nose and post-nasal drip
Fever, fatigue, and other general symptoms are also common signs of an infection.
How Can the Dentist Tell if the Sinus is Perforated?
It’s important to detect and treat a sinus injury early because the sooner you get treatment, the better the chances of healing.Here's how your dentist can find out:
Detecting sinus perforation during the procedure
During the procedure, you might feel pressure pushing upward toward your sinus. You could also experience sudden pain and heavy bleeding.
Sometimes, the tooth may come out with a piece of bone. This may suggest a rupture of the sinus floor and thus an oroantral communication.
Detecting sinus perforation after the procedure
If the sinus is perforated, shining a light on the extraction site can sometimes show the soft tissue lining of the sinus.
One common test is to hold a mirror near the extraction site while you breathe through your nose. Tiny droplets on the mirror mean the sinus is leaking.
Your dentist might also ask you to blow while holding your nose closed. If air bubbles or blood come out of the wound, it’s a sign of sinus injury.
Don’t try these tests at home! Putting too much pressure on your sinuses can make the injury worse.
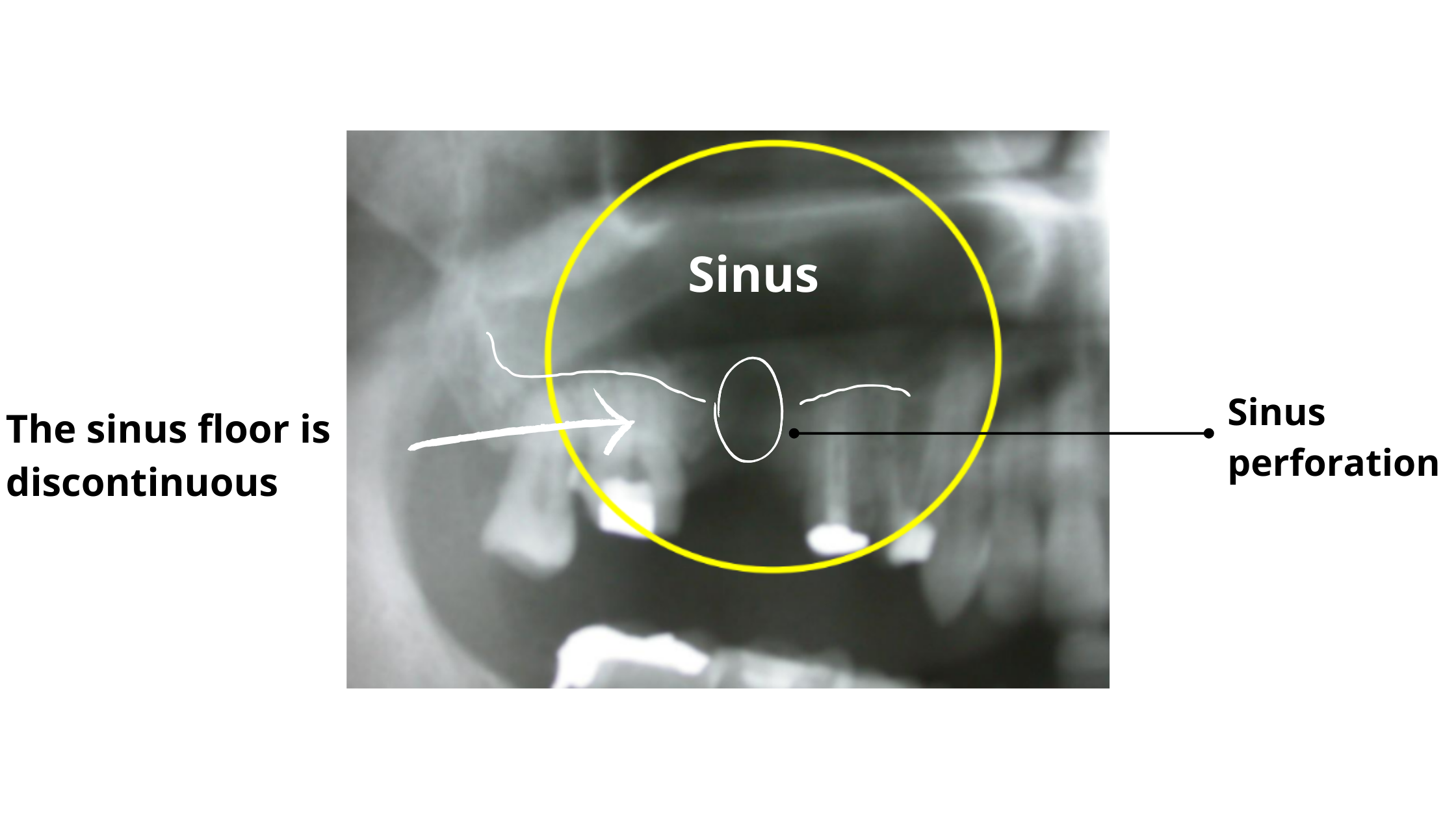
How Does a Perforated Sinus Look Like on X-rays?
A sinus perforation appears on X-rays as a break or gap in the sinus floor.You can see it on the X-ray below, taken after the extraction of a first molar. It shows that the sinus is directly connected to the mouth.
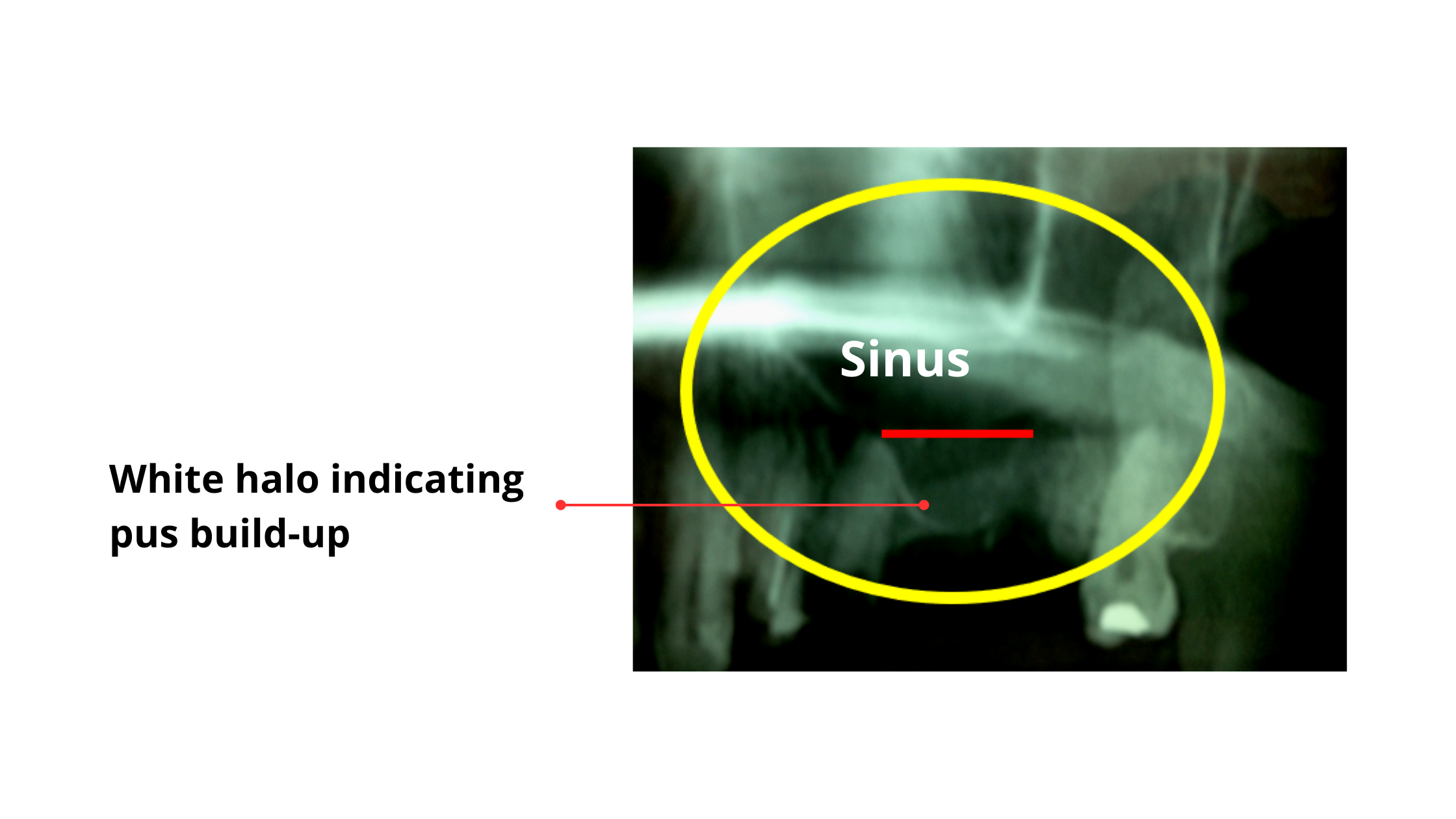
Sinus infections can also be detected on X-rays. In the panoramic images below, a dental infection shows up as a white halo filling the sinus cavity, indicating inflammation and pus buildup.
Potential Complications of Perforated Sinus after Tooth Extraction
The primary concern of sinus perforation following tooth extraction is fistulization.Fistulization:
When a perforation fails to close naturally, a canal forms, establishing a permanent connection between the sinus and the mouth—this is known as a fistula.
Fistulas typically develop in cases of larger and persistent perforations, often after 48-72 hours have passed without spontaneous healing. If left untreated, a fistula becomes a gateway for food, saliva, and oral bacteria to enter the sinus. When these accumulate, the result is infection and the onset of sinusitis.
The Different Treatment Options for Sinus Perforation
Your dentist will first consider the size of the exposure and the presence of any infection.Depending on your specific situation, one of the following treatment options may be recommended:
If the Perforation is Small without Sinus Infection:
For minor perforations, typically less than 2mm, no immediate treatment may be required, as these small openings often close spontaneously during the natural healing process. However, if the defect fails to heal on its own, a fistula may form, requiring surgical closure to prevent potential infection.
If the Perforation is Large without Sinus Infection:
When the perforation exceeds 2mm, spontaneous recovery becomes less likely. Surgical intervention may be required to close the communication. For moderate-sized openings, the technique involves cutting the gum, pulling it to cover the defect, and suturing it in position. In cases of larger defects, soft tissue grafting may be considered.
If the Perforation is Large with Sinus Infection:
When the perforation has led to infection, the initial step is to treat sinusitis with the help of an ENT specialist. The goal is to establish a healthy, bacteria-free environment before considering surgical closure.
Once the infection is under control, the next step involves surgical closure of the oroantral communication.
Post-Surgical Care: Ensuring a Smooth Recovery
After surgical closure of a sinus perforation, proper post-surgical care is crucial to promote healing and prevent complications. Here are a few tips:Things to Avoid:
- Putting Pressure or Suction on Your Mouth:
- Don’t blow your nose hard while your mouth is closed.
- Avoid smoking or drinking through a straw.
- Hard Foods:
- Stay away from hard foods that may irritate the surgical site.
- Chewing on the Treated Side:
- Don't chew on the area where the surgery was done.
- Strenuous Physical Activity:
- Avoid strenuous physical activities during the initial recovery phase.
- Touching the Wound:
- Don’t touch the stitches or surgical area with your tongue or fingers for at least 7 days after surgery.
Things to Do:
- Liquid Diet:
- Stick to a liquid diet for the first few days after surgery.
- Chew on the Opposite Side:
- When eating, chew on the opposite side of your mouth.
- Managing Coughs and Sneezes:
- Keep your mouth open if you need to cough or sneeze to minimize pressure on the surgical site.
- Maintaining Oral Hygiene:
- Keep the wound clean by rinsing with warm saline mouth rinses, starting gently from the second day following surgery.
- Medications:
- Take your medication exactly as prescribed.
- Oroantral communication, its causes, complications, treatments and radiographic features: A pictorial review - PMC (nih.gov)
- Management of Oro-antral Communication and Fistula: Various Surgical Options - PMC (nih.gov)
- Odontogenic sinusitis: A review of the current literature - PMC (nih.gov)
- Management of oro-antral fistula: Two case reports and review - PMC (nih.gov)
- OroAntral Communications and OroAntral Fistula | SpringerLink