Why Can Extracting Rotten Teeth be Challenging?
When a tooth is so badly damaged that it can’t be repaired or restored, extraction is often the only option left.
In most cases, the procedure is quick and straightforward. However, it can become more challenging when the tooth is severely decayed, broken, or when only the roots remain.
In this article, we’ll walk you through the process of removing badly damaged or rotten teeth, potential difficulties and complications, what to expect during the procedure, and how recovery typically goes.
In most cases, the procedure is quick and straightforward. However, it can become more challenging when the tooth is severely decayed, broken, or when only the roots remain.
In this article, we’ll walk you through the process of removing badly damaged or rotten teeth, potential difficulties and complications, what to expect during the procedure, and how recovery typically goes.
In this article:
1. Extracting a Rotten Tooth Can Sometimes be Challenging
2. Rotten Teeth May Need Special Techniques
3. Risks and complications of extracting rotten teeth
4. Why Should a Rotten Tooth be Removed in the First Place?
5. Recovery After Tooth Extraction
6. Takeaway
Extracting a Rotten Tooth Can Sometimes be Challenging
Rotten teeth are teeth that have been severely damaged by decay or infection. It could also be a tooth with a large, old filling where decay has returned underneath.The biggest challenge when extracting rotten teeth is their fragile and brittle nature. During the procedure, these teeth are more likely to crack or break when grasped with forceps to loosen and remove them.
So, instead of coming out as a single intact tooth, they may fracture into several pieces (as shown below).
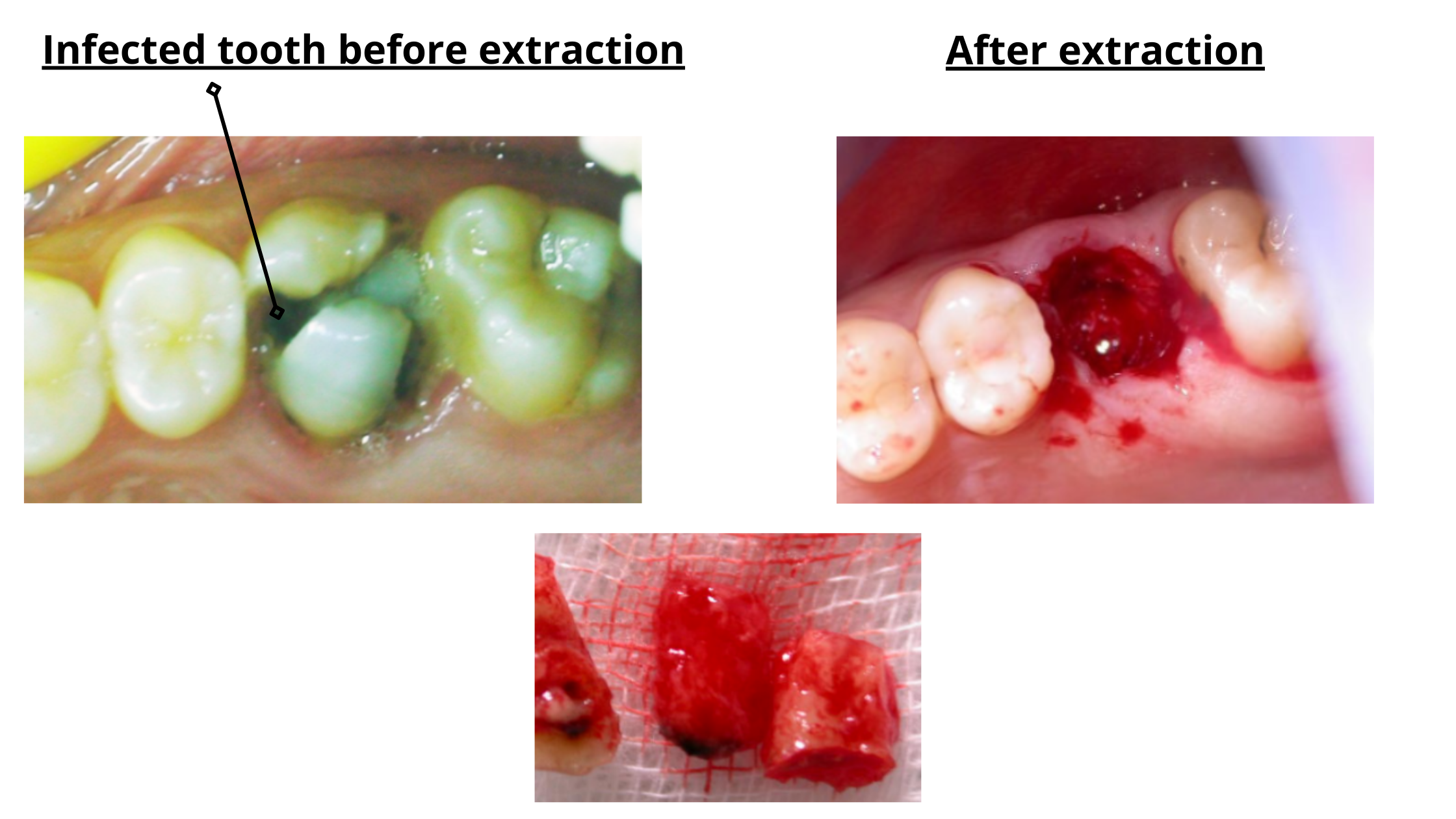
The tooth breaking during extraction isn’t necessarily a bad thing, but it can make the procedure more challenging.
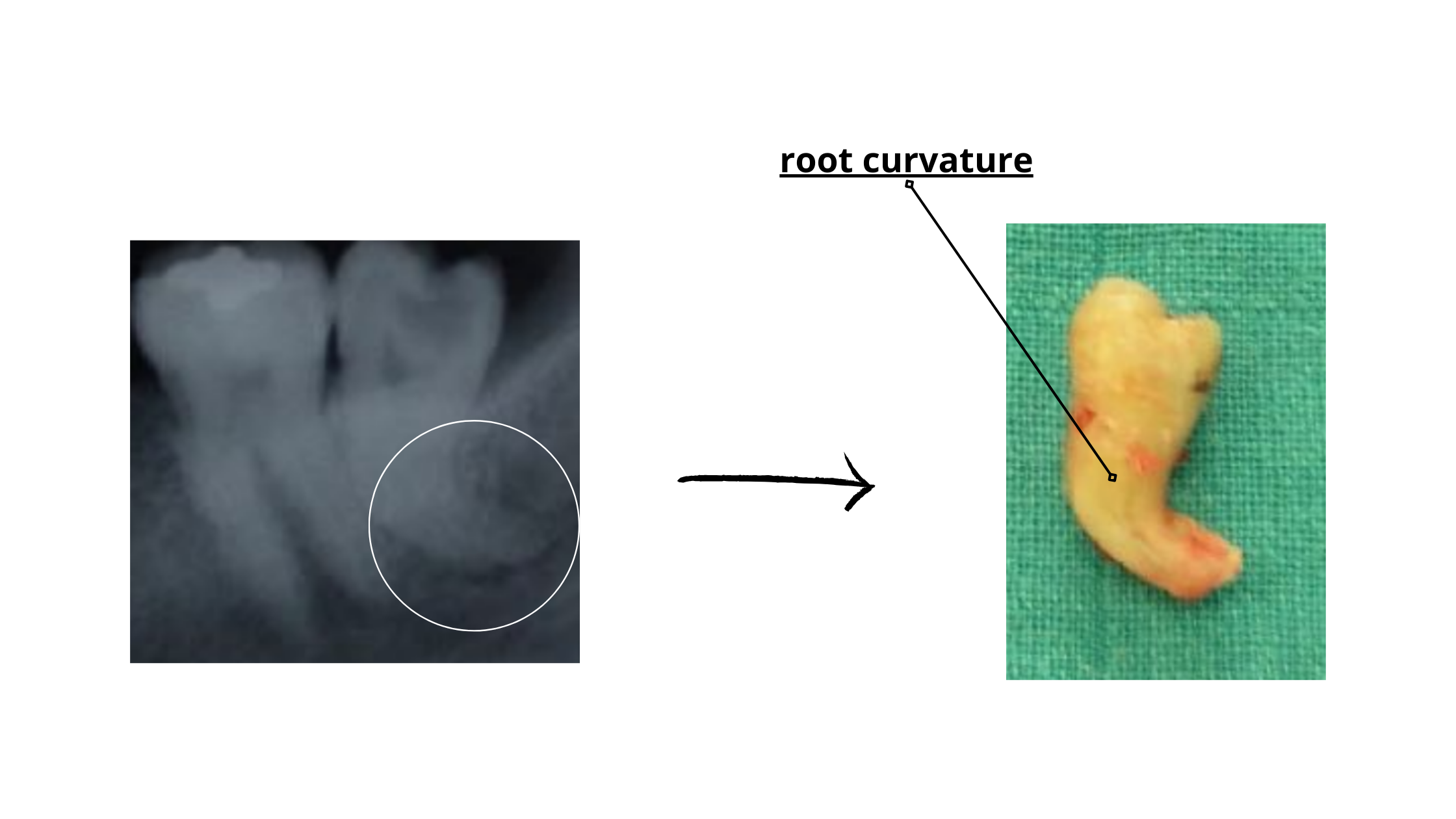
It's even worse when only the roots remain. While root removal is usually safe and straightforward, the following factors can make the process more complex and time-consuming:
- Roots with unusual shapes
- Curved or divergent roots (as shown below)
- Roots that are tightly fused with the surrounding bone
Rotten Teeth May Need Special Techniques
For teeth that are too damaged or brittle, and when your dentist expects potential difficulties during extraction, special techniques may be needed for a safer procedure.One of the most commonly used is called alveolectomy. In this technique, your dentist raises a small gum flap and removes a bit of the surrounding bone to loosen the tooth and make it easier to extract.
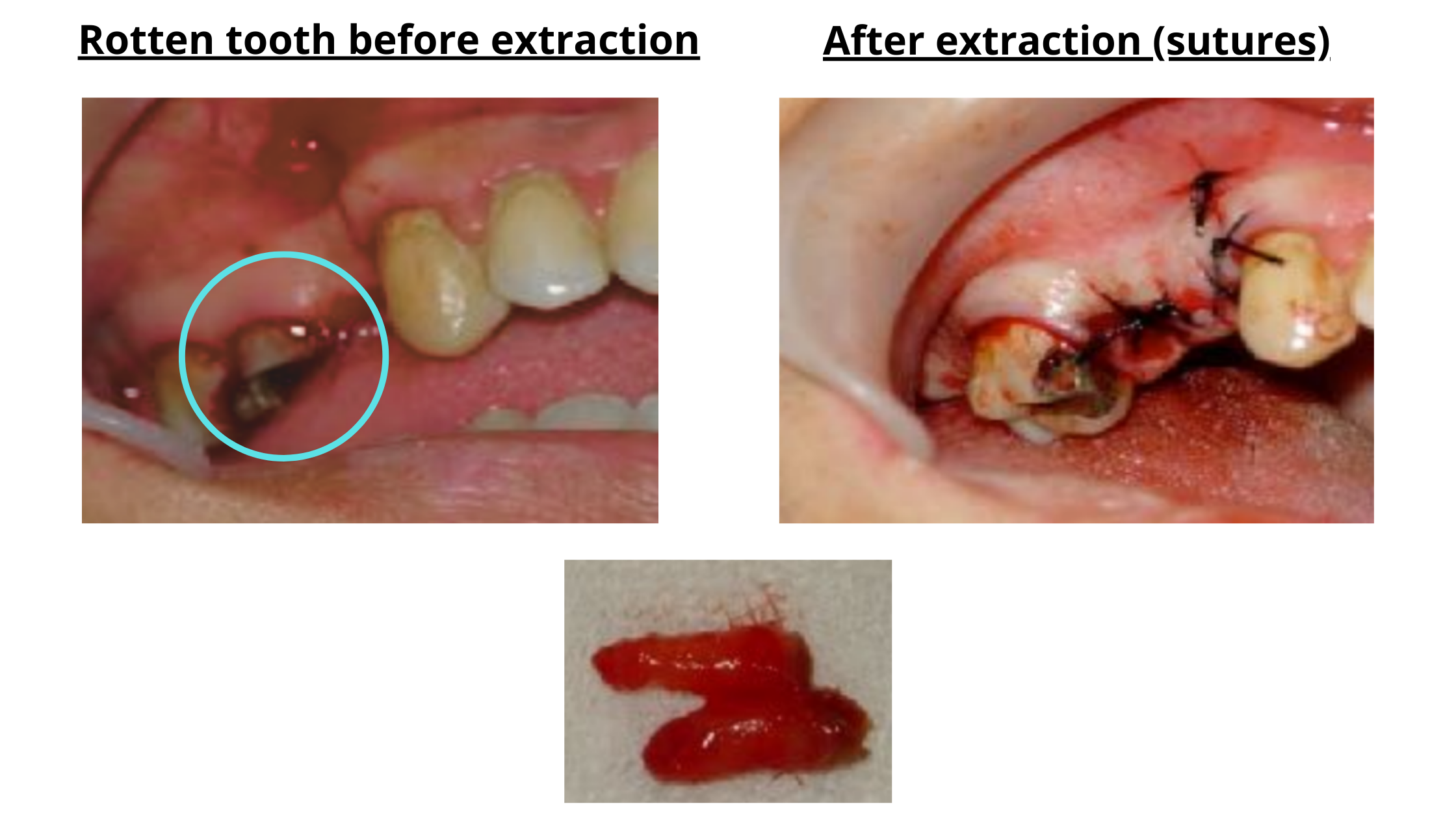
Alveolectomy for Extracting a Brittle Tooth
For back teeth with multiple roots, a technique known as tooth sectioning may be used. This involves dividing the tooth into smaller pieces so each part can be removed individually.
These methods make the extraction much more straightforward. However, since they involve trimming some of the bone, they are slightly more invasive and may require a longer healing period, with a bit more swelling and discomfort afterward.
Risks and complications of extracting rotten teeth
Complications are more often associated with complex and lengthy procedures.For example, the longer it takes the dentist to extract the tooth, and the deeper it is embedded in the bone, the greater the risk of post-operative complications.
Here are some of the potential risks associated with extracting rotten or brittle teeth:
Dry Socket
Dry socket is one of the most common post-operative complications after tooth extraction. It occurs in 0.5% to 5.6% of cases, and can reach up to 35% when removing lower wisdom teeth that are trapped in the jawbone.
The main risk factors include a long, complex extraction and a pre-existing tooth infection.
So, what exactly is dry socket?
It’s an extremely painful condition that happens when the blood clot inside the socket is lost too early or doesn’t form at all. This exposes the underlying bone and nerves.
Symptoms usually appear around the third or fourth day after extraction and include intense throbbing pain, bone exposure, and a bad taste or breath in the mouth.
Dry socket typically resolves on its own, but it delays healing, making recovery take much longer without proper treatment.
Bone Damage during Tooth Extraction
Sometimes, a small portion of the bone that supports the tooth may break off or come out along with the tooth during extraction.
This can happen for several reasons:
- Excessive force is applied while removing the tooth.
- The surrounding bone is already weak, often due to gum disease or a pre-existing infection.
- The tooth roots are fused with the bone, making extraction more difficult.
- The roots have curved or unusual shapes that complicate removal.
In most cases, this is a minor issue and nothing to worry about. However, if a small bone fragment is accidentally left inside the socket, it may lead to post-operative infection.
Sinus Complications
The sinuses are air-filled cavities located on either side of the cheeks. They are positioned just above the back teeth of the upper jaw.
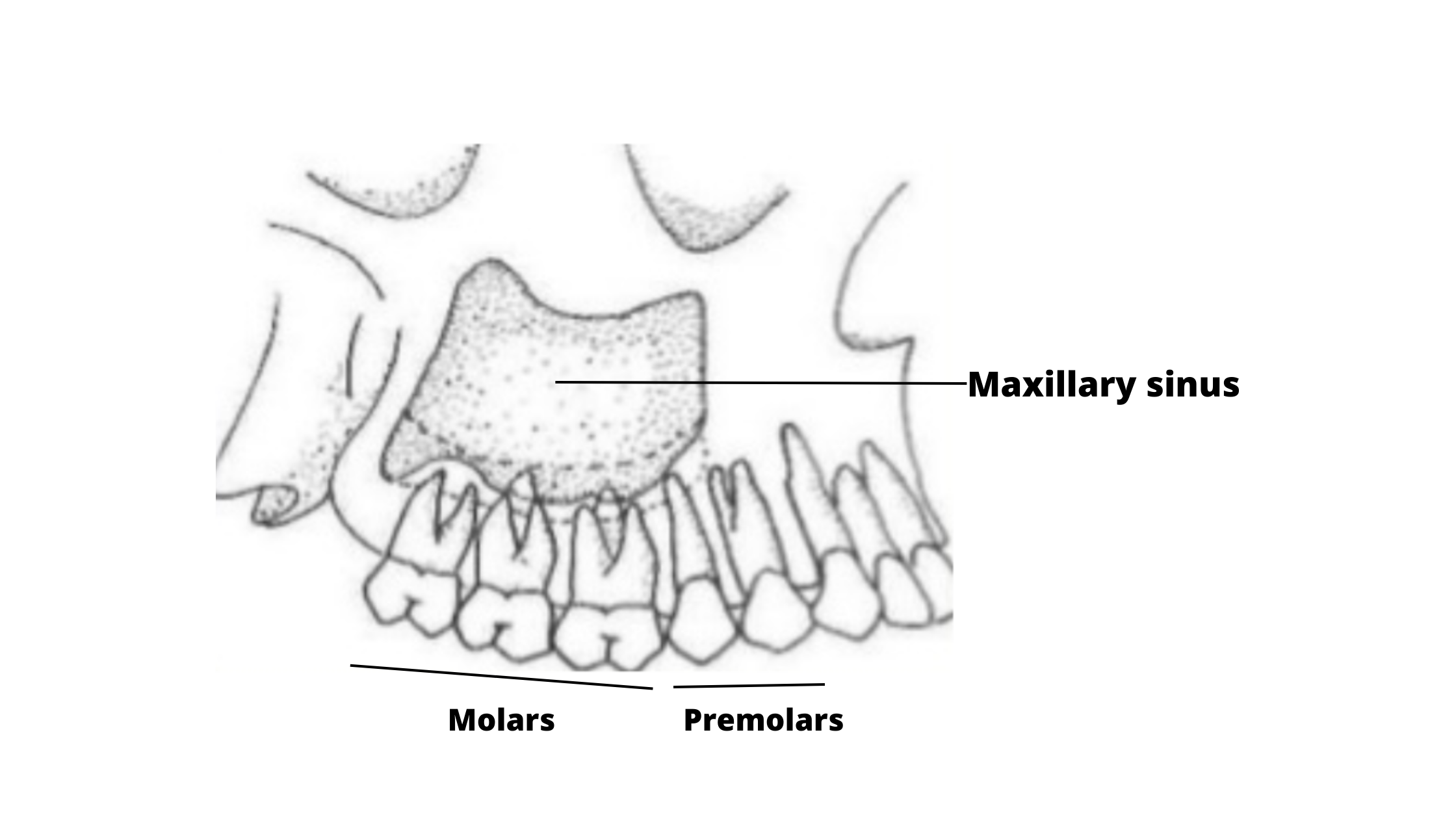
During the extraction of the upper back teeth, the overlying sinuses can be accidentally damaged or perforated.
This is more likely, and sometimes even unavoidable, when the tooth roots extend directly into the sinuses.
If the sinus is accidentally damaged during extraction, it can lead to a sinus infection, known as sinusitis.
Infections After The Procedure
Post-operative infection, also called socket infection, occurs when bacteria enter and multiply inside the extraction wound.
It can happen if a foreign object — such as food debris or a piece of tartar — gets trapped in the socket, or if a pre-existing infection wasn’t fully cleared.
Signs of post-operative infection include:
- Pus leaking from the wound
- A socket that appears filled with a dark substance
- Pain and swelling that are getting worse instead of better
- Bad breath and a foul taste in the mouth
- Fever
Bone Spur
This occurs when a small root or bone fragment becomes trapped inside the socket.
The body treats it as a foreign object and works to expel it. During this process, the fragment may emerge through the gum, gradually pierce the gums, and eventually be completely expelled from the mouth.
The bone spur may cause some irritation, especially if it has sharp edges.
Why Should a Rotten Tooth be Removed in the First Place?
Tooth extraction, although a common and routine procedure, is the last resort when the tooth cannot be saved.This is typically the case when a tooth is severely decayed, has a deep, irreversible crack or fracture, or has become excessively loose due to bone loss. Trying to repair or restore such teeth often leads to early restoration failure, making extraction the most reasonable option.
Another reason for removal is a persistent or stubborn dental infection that fails to resolve despite treatment efforts. Leaving the tooth in place can allow the infection to spread, causing far more damage than simply removing the tooth.
Recovery After Tooth Extraction
The recovery process is usually smooth and without problems. During the first few days, some side effects are completely normal. Like any surgical procedure, these are temporary and improve as healing progresses.Here’s what you can expect during the recovery period:
Day 1-3: Blood Clot Formation and Inflammation
- What Happens? Immediately after the procedure, the socket is filled with a blood clot, protecting the wound, stopping bleeding, and promoting healing. Inflammation kicks in early to help clean the wound, which results in the common side effects such as pain, swelling, and redness.
- What does it look like? The socket appears filled with a shiny red blood clot. It's normal to experience some pain and swelling. The discomfort peaks on the first day and then gradually decreases over the following days.
Day 4-5: Granulation Tissue Formation
- What Happens? The blood clot turns into firmer, pale pink granulation tissue.
- What does it look like? Pain and swelling decrease as inflammation subsides. The socket is now filled with granulation tissue.
Week 1-2: Early Bone Formation
- What Happens? New bone begins filling the socket. It is fragile at first but gradually strengthens over the following weeks.
- What does it look like? Pain and swelling should be gone, and the socket will be closed with new gum tissue.
Week 4-16: Complete Bone Formation and Maturation
Takeaway
Extracting rotten teeth is usually quick and straightforward, much like removing regular teeth.However, if a tooth is deeply embedded in the bone, too brittle, or has an unusual shape, your dentist may use extra techniques to make the extraction safer and easier.
Regardless of the method, it’s important to follow your dentist’s instructions. Doing so helps ensure a smooth recovery and reduces the risk of common complications, such as dry socket.