When root canal fails: Tooth extraction as a last resort
 Root canal treatment is a highly successful procedure that can save teeth from extraction for many years. According to studies, the survival rate of root canal teeth can be as high as 97% within 8 years.
Root canal treatment is a highly successful procedure that can save teeth from extraction for many years. According to studies, the survival rate of root canal teeth can be as high as 97% within 8 years.
The not-so-great news is that teeth treated with a root canal still carry a small risk of needing extraction later on — about 1–2% more each year.
In this article, we’ll explain when and why a tooth that had a root canal might still need to be extracted — and what makes extracting a root canal-treated tooth different from a regular one.
In this article...
- How Do I Know if a Root Canal has Failed?
- When Tooth Extraction Becomes the Last Resort After a Failed Root Canal
- How Is Extracting a Root Canal Tooth Different from a Regular Extraction?
- Healing After Extracting a Tooth with a Failed Root Canal
- Complications After Removing a Root Canal-Treated Tooth
How Do I Know if a Root Canal has Failed?
A root canal is considered a failure when the tooth doesn’t heal properly after treatment, or when the infection persists—or comes back later.Pain is usually one of the first and most common signs that something’s wrong. If you suddenly feel pain again or the tooth continues to hurt even months after treatment, it could be a sign of root canal failure.
But not all failed root canals cause obvious symptoms.
Sometimes, an infection can silently develop around the tooth without any pain or discomfort. Only a dental X-ray can reveal such chronic conditions.
That’s why it’s so important to have regular check-ups with your dentist after a root canal. It’s always better to catch dental infections early before they turn into more serious problems.
When Tooth Extraction Becomes the Last Resort After a Failed Root Canal
When root canal treatment fails, we always try to save the tooth by giving it a second chance through retreatment or surgery. However, there are situations where the tooth cannot be saved, and extraction becomes the only option.Unlike what you might think, it’s not always the fault of the root canal treatment itself. The most common reasons we may need to extract the tooth are:
1. Lack of restoration:
Many studies have shown that teeth without proper restoration after root canal treatment are more likely to be extracted than those that do.
One study showed that teeth without restoration after root canal treatment are three times more likely to be extracted later than restored teeth.
Another study showed that delaying restoration for more than 60 days after treatment significantly increases the risk of extraction by 73%.
Why is it so important to restore the tooth as soon as possible? Because placing a crown or filling right after a root canal helps seal the tooth, preventing bacteria and saliva from getting back into the root canals.
The longer the tooth is left unrestored, the greater the risk of infection—and the higher the chance of treatment failure.
2. The tooth is severly damaged:
When the tooth is too damaged to support a crown or filling, extraction may be the only option. This can be due to extensive decay, fracture, or advanced gum disease with severe bone loss.
3. Root fracture:
During the drilling and shaping process of a root canal, some of the tooth’s natural structure is removed.
This can weaken the tooth and make the roots more brittle, increasing the risk of fractures.
Unfortunately, when a root cracks, it’s often difficult—or even impossible—to repair, which can make extraction the only option.
4. Tooth decay:
According to one study, subgingival decay (a type of tooth decay that spreads beneath the gum line) is the most common reason for extracting molars that have had root canal treatment.
Root canal-treated teeth aren’t immune to decay. That’s why maintaining excellent oral hygiene is even more important to save your tooth as long as possible.
5. Persistent infection:
If the infection persists or keeps returning even after retreatment or surgery, extraction might be the only option left.
How Is Extracting a Root Canal Tooth Different from a Regular Extraction?
For a tooth that has had a root canal, the extraction is often straightforward. However, sometimes a surgical removal is necessary, especially when the tooth is too weak and likely to break with a standard extraction technique.If the tooth is strong enough to be securely held by extraction tools without breaking, the procedure can be quick and simple, much like a regular tooth extraction, with minimal risk of complications.
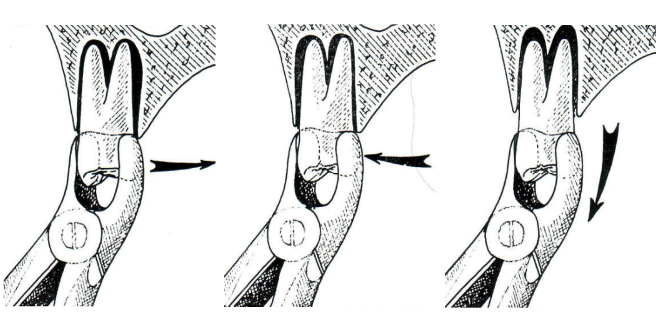
Simple extraction technique
However, if the tooth is crowned, too weak, or has a post (an artificial root placed inside the root canals), the chances of breaking the tooth or roots during extraction are higher.
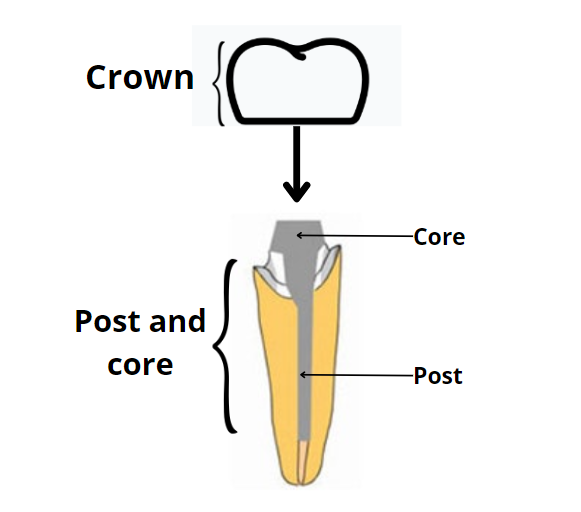
In these cases, your dentist may prefer the surgical approach. The typical steps include:
- Numbing the area
- Making a small cut and lifting the gums to expose the bone
- Drilling a bit of bone
- Loosening the tooth
- Removing the tooth
Your dentist might also use a technique called “sectioning,” where the tooth is divided into two or more pieces before removal.
These surgical methods are more complex and may cause more post-operative discomfort. However, they help make extracting brittle teeth safer and reduce the risk of complications like tooth or root fractures—which could make the procedure even more difficult.
Healing After Extracting a Tooth with a Failed Root Canal
Whatever extraction technique is used, the healing process is the same.The first step is the formation of a blood clot—a mass of blood that fills the socket and stays there for the first two days.
This blood clot then turns into granulation tissue, which supports the regeneration of bone and gum tissue.
Over the next few weeks, bone starts filling the empty socket while the gum tissue gradually covers the wound.
After about 2 to 3 months of healing and tissue maturation, you’ll be ready to receive your dental implant.
Here are some things to consider if you have chosen the implant solution:
- It’s important not to delay treatment. Without the tooth to stimulate the jawbone, bone loss can happen quickly—especially within the first year. That’s why early implant placement is key.
- If your bone was weak or thin before the extraction, you might need a bone graft either during the extraction or later before getting an implant.
- An alternative to waiting for months of healing is immediate implant placement.
With this technique, the implant is placed right after the tooth is extracted. It can save you time and help prevent bone loss, which often occurs after a tooth is removed.
Complications After Removing a Root Canal-Treated Tooth
Complications after extracting a root canal-treated tooth are rare, especially if the procedure goes smoothly and you follow your dentist’s aftercare instructions.Still, it’s good to be aware of what could happen so you can catch any issues early. Here are some possible complications:
Dry Socket:
Dry socket is the most common complication that happens when the blood clot that normally forms in the extraction site is disturbed or dislodged too early, leaving the bone exposed.
It usually sets in 2 to 3 days after the procedure, causes severe pain, and slows down the healing process.
To prevent dry socket, avoid smoking, rinsing forcefully, using a straw, or doing anything that creates suction in your mouth during the first two days after the extraction.
Infection:
The socket can become infected if some infected tissue is left behind during the procedure, or more commonly, if bacteria enter the wound during healing.
You can prevent this by avoiding things that irritate the area, like crunchy or spicy foods. Also, start rinsing your mouth with salt water several times a day, starting on day 2.
Signs of infection include fever, constant throbbing pain, a gray-colored substance in the socket, or pus coming from the area. If you notice any of these, contact your dentist right away.
Bleeding:
Some bleeding is normal after an extraction, but if it persists or becomes heavy, contact your dentist immediately.
Bone loss:
Bone loss is one of the biggest challenges after tooth extraction. If the tooth has been missing for some time, the bone underneath will begin to shrink—especially during the first year. This can make placing an implant difficult or even impossible.
The best way to prevent this is to get a dental implant as soon as possible.
If the bone has already collapsed, a bone graft may be needed before an implant can be placed.
- Tooth survival after endodontic treatment https://onlinelibrary.wiley.com/doi/full/10.1111/iej.13835
- The 5-Year Survival Rate of Nonsurgical Endodontic Treatment: A Population-based Cohort Study in Korea https://pubmed.ncbi.nlm.nih.gov/31439355/
- Tooth survival following non-surgical root canal treatment: a systematic review of the literature https://onlinelibrary.wiley.com/doi/10.1111/j.1365-2591.2009.01671.x
- Failure of endodontic treatment: The usual suspects https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4784145/
- Survival Rates of Endodontically Treated Teeth After Placement of Definitive Coronal Restoration: 8-Year Retrospective Study https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7041432/
- Factors Associated with Extraction following Root Canal Filling in Adults https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8138334/
- Assessment of extracting molars and premolars after root canal treatment: A retrospective study https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6823745/