The telltale signs of failed root canal with X-ray pictures
 A root canal is a highly successful procedure that can save your tooth for many years, or even decades. Studies consistently show that root canal–treated teeth have a survival rate of up to 97%, even after eight years of follow-up!
A root canal is a highly successful procedure that can save your tooth for many years, or even decades. Studies consistently show that root canal–treated teeth have a survival rate of up to 97%, even after eight years of follow-up!
However, these teeth are not immune to future problems. Cavities, infections, or other complications can still occur and may cause the root canal to fail prematurely.
In this article, we’ll explore the common causes and telltale signs of root canal failure. We’ll also show you how it looks on X-rays, so you can better understand when things are healing properly—and when something might be going wrong.
In this article...
- Telltale signs of root canal failure (with X-ray pictures):
- Persistent pain after the procedure:
- Swelling after root canal:
- Gum abscess or boil near the treated tooth:
- How do you know if the tooth has healed properly?
- Can a tooth with a failed root canal be saved?
- When is extraction the last option?
Telltale signs of root canal failure:
Recognizing the early warning signs of root canal failure will help you catch issues early and get the right treatment before things get worse. Here are the telltale signs to watch out for:1. Persistent pain after the procedure:
After a root canal treatment, it is common to experience slight to mild pain, but it should gradually subside within 5 to 7 days.
However, persistent pain that lasts longer than expected or suddenly comes back isn’t normal. It’s a sign you should get it checked out as soon as possible.
Possible causes of persistant pain include:
1. Infection:
A tooth with root canal treatment is not immune to infection. It can occur even several months or years later.
This can happen if the root canal filling wasn’t done properly or if the tooth wasn’t restored or crowned soon enough after treatment. In that case, bacteria from saliva can sneak in, grow silently, and eventually cause an infection.
An infection that occurs right or a few days after the procedure is called a flare-up. It’s a very painful complication that requires immediate treatment to prevent further issues.
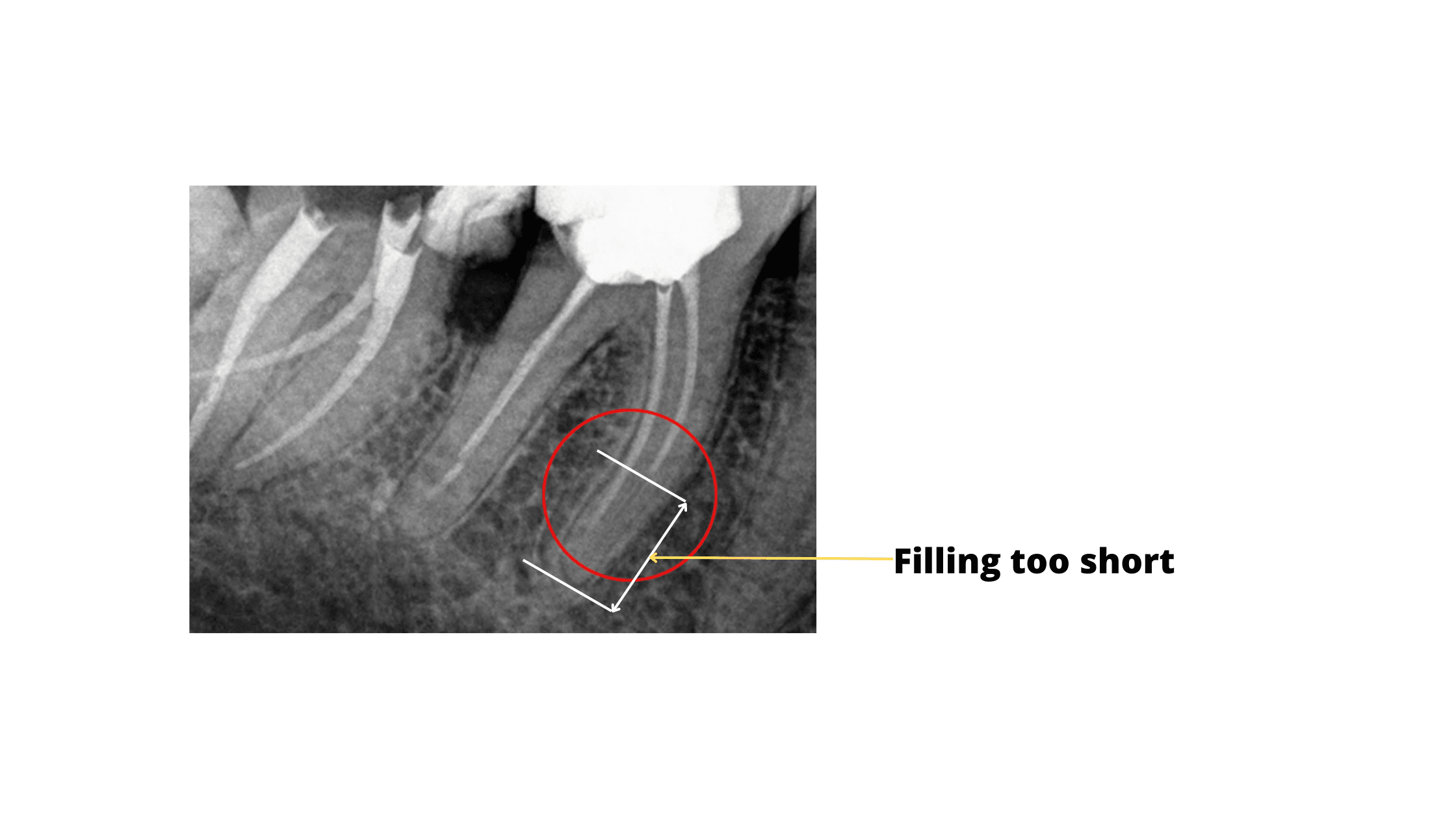
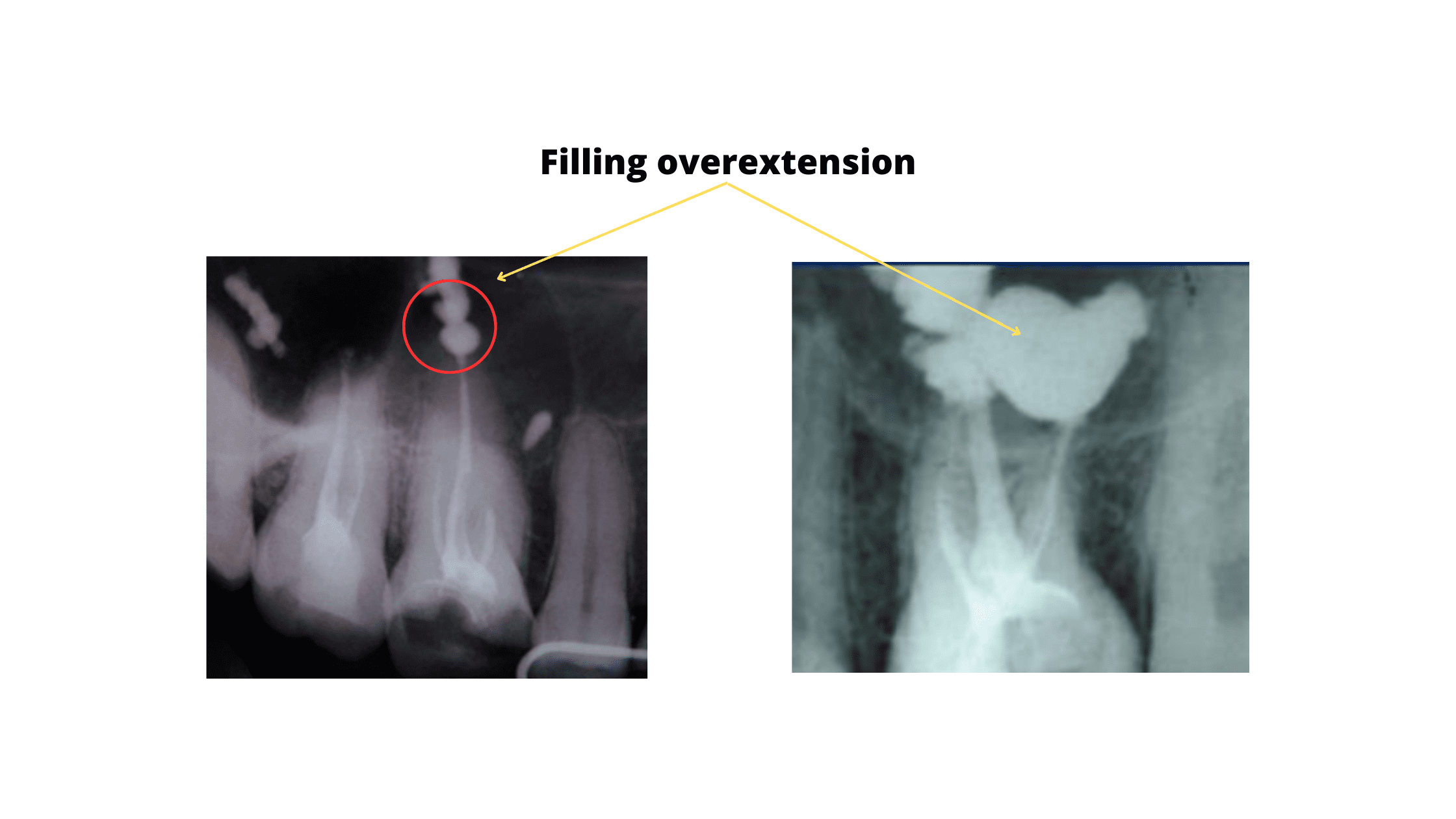
2. Poor root canal filling:
A poor root canal filling can either fall short (leaving a gap) or extend beyond the root tip. Both situations can cause persistent pain and interfere with healing, eventually leading to treatment failure.
If the filling is too short, you might not feel pain right away. However, over time, bacteria can grow in the empty space left behind, eventually causing an infection.
On the other hand, if the filling material extends beyond the root tip, it can cause immediate pain—often starting on the first day of treatment. That’s because the material is seen as a foreign body. When it overflows into the surrounding tissue, it can trigger irritation, inflammation, and pain.
Below is a picture showing a short root canal filling:
The following X-ray shows the filling material extending beyond the root tip:
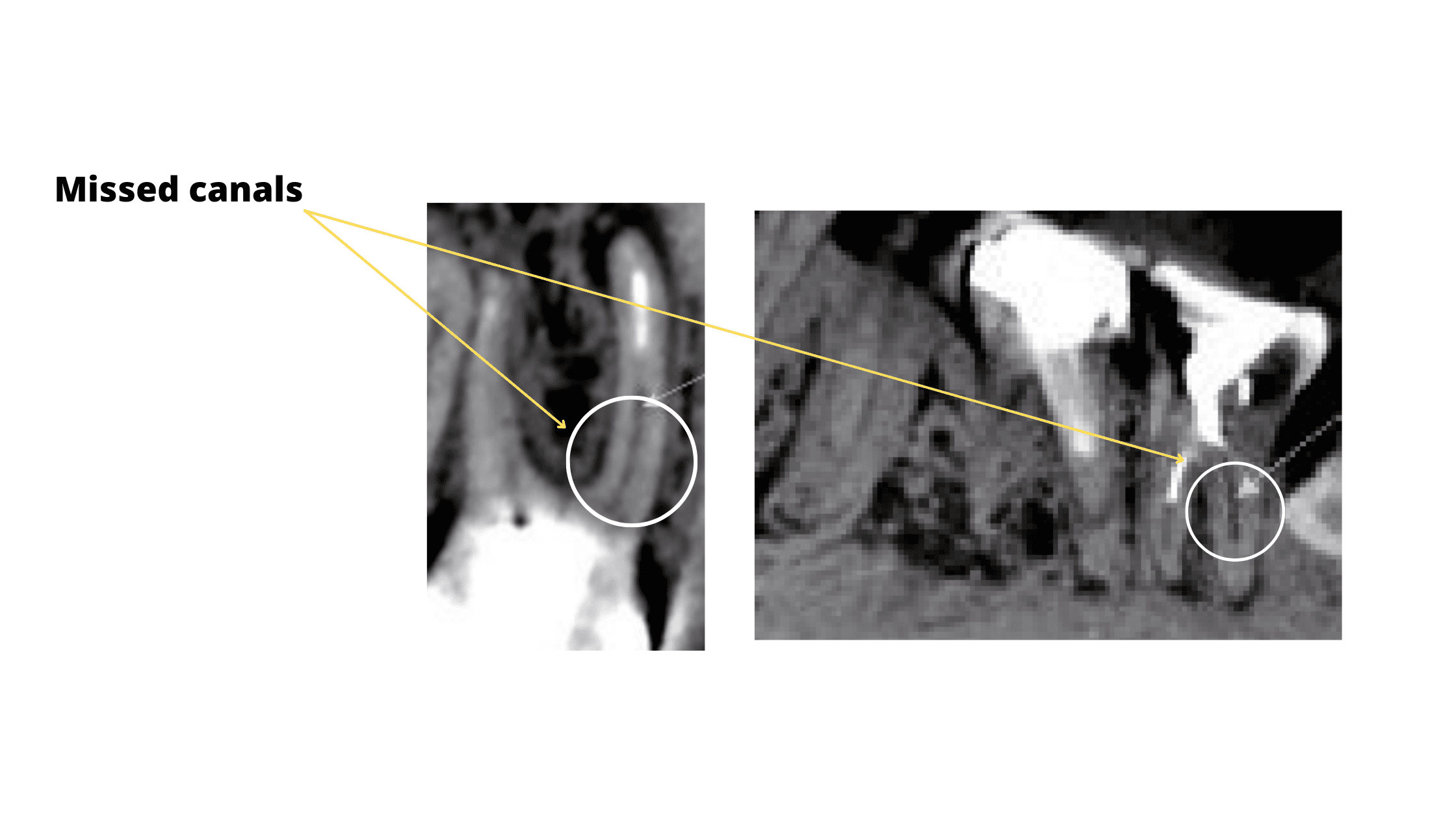
3. Missed canal:
A common cause of root canal failure is when a canal is missed during the cleaning and shaping process. If even one canal is left untreated, the infection can remain inside the tooth, causing persistent pain and eventual treatment failure.
This issue is more common in molars, which often have multiple roots and complex canal systems that can be difficult to locate.
Missed canals may not be obvious on standard X-rays, but they can sometimes appear as a thin dark line along the root, indicating an unfilled space.
Here's what it looks like:
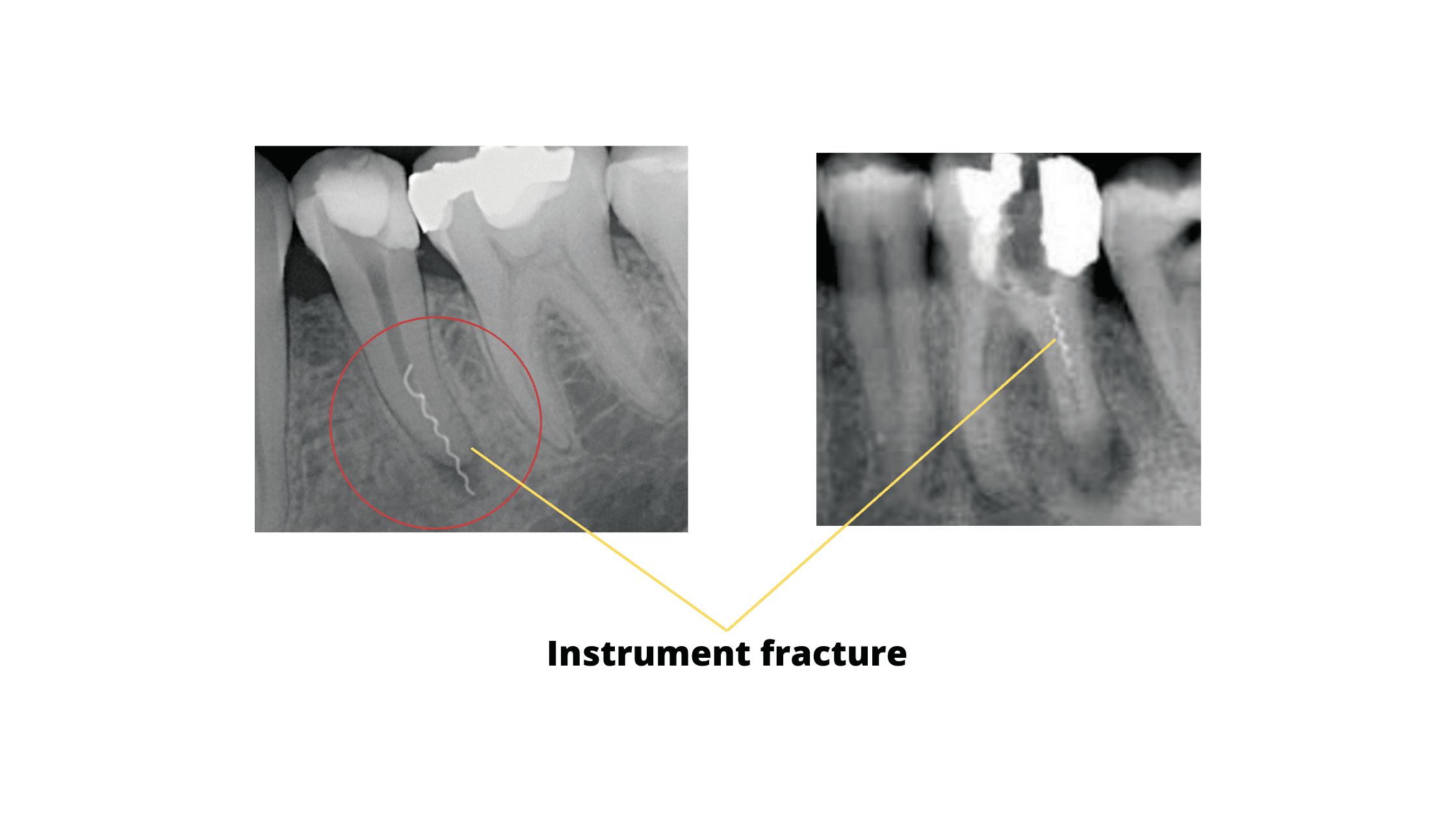
4. Instrument fracture:
Endodontic files are thin, sharp instruments used to shape and clean infected root canals. Sometimes, one of these files can break inside a canal during the procedure, preventing complete access and cleaning.
This happens quite often, but it’s usually not a serious problem. In most cases, the broken piece can be removed, and the treatment can be safely completed by repeating the procedure.
X-ray of an instrument fracture:
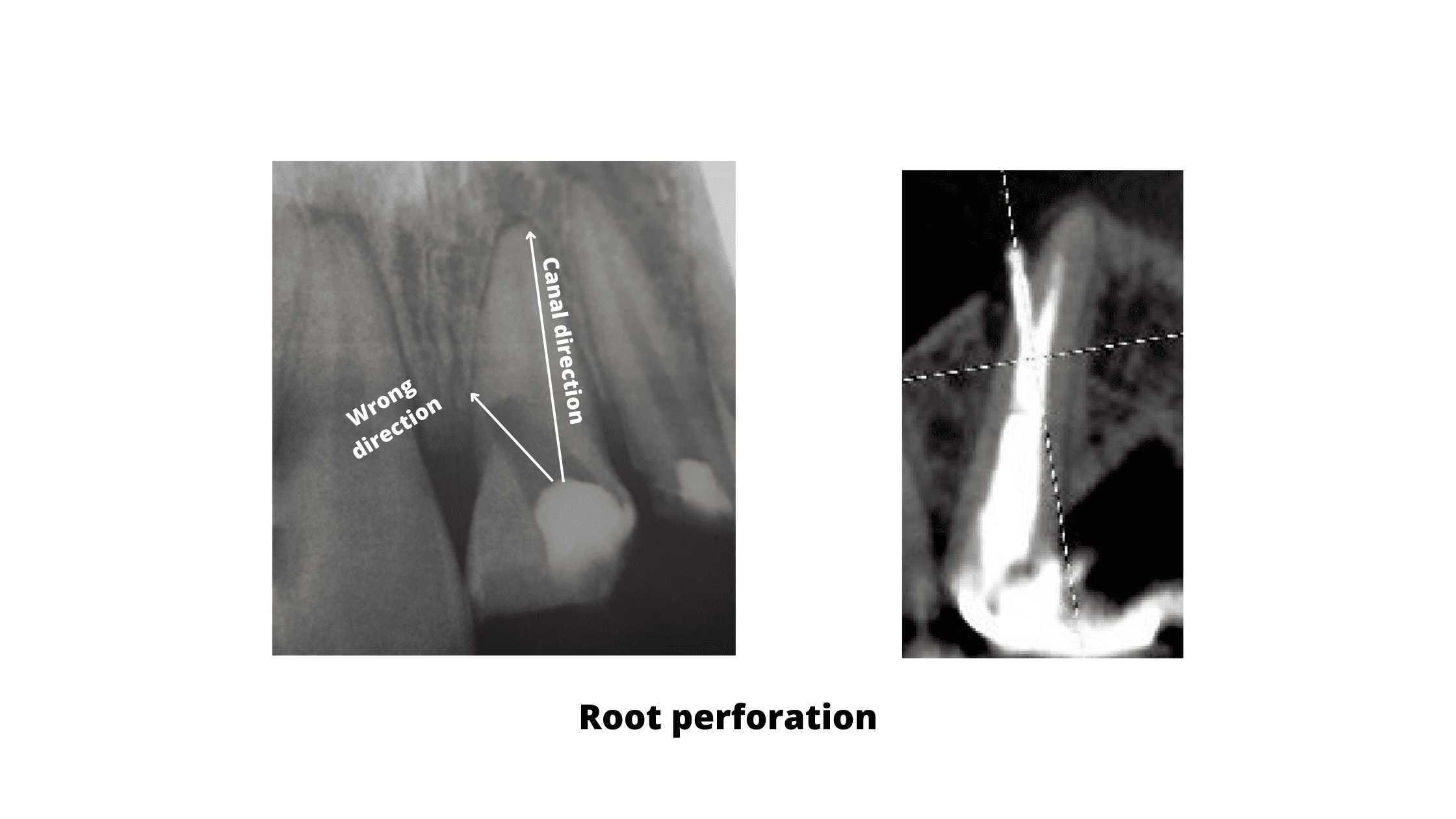
5. Root perforation:
Root perforation happens when a dental instrument is accidentally pushed in the wrong direction, going outside the natural canal. This can cause the tool to drill into healthy tissue, creating an unwanted hole in the root.
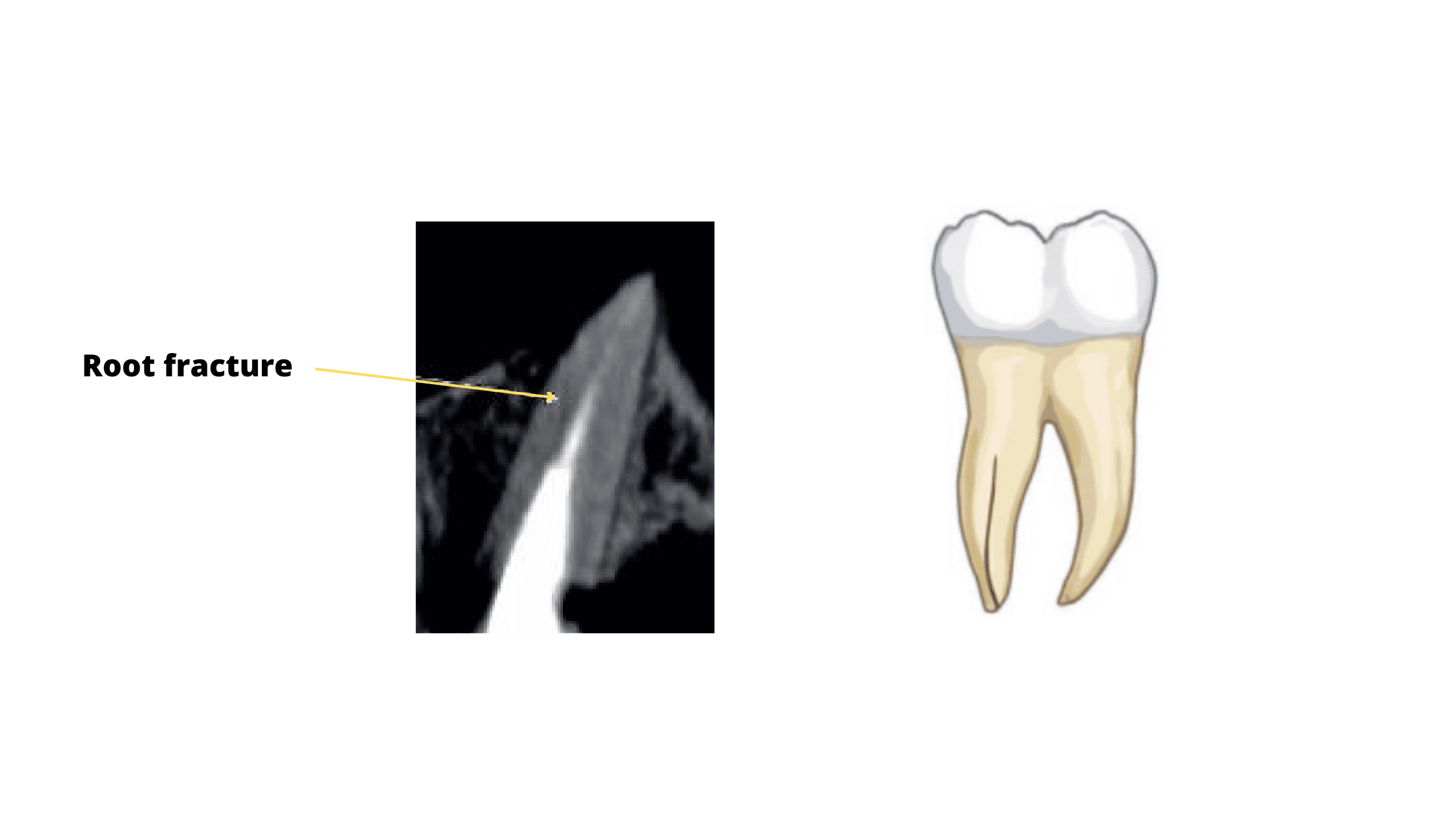
6. Root fracture:
Root canal treatment can weaken the tooth and make it brittle and susceptible to breakage. One of the most common injuries to endodontically treated teeth is root fracture.
If you feel pain when biting or chewing, or notice an abscess near the tooth, it could be a sign of a root fracture that needs further treatment.s
2. Swelling after root canal:
It's not uncommon to experience some swelling following a root canal treatment.
It's a normal part of the healing process as your body works to fight off any remaining infection and repair the damaged tissues.
However, if the swelling doesn't improve or is accompanied by other symptoms such as severe pain, pus leakage, or fever, it may be a sign of an infection.
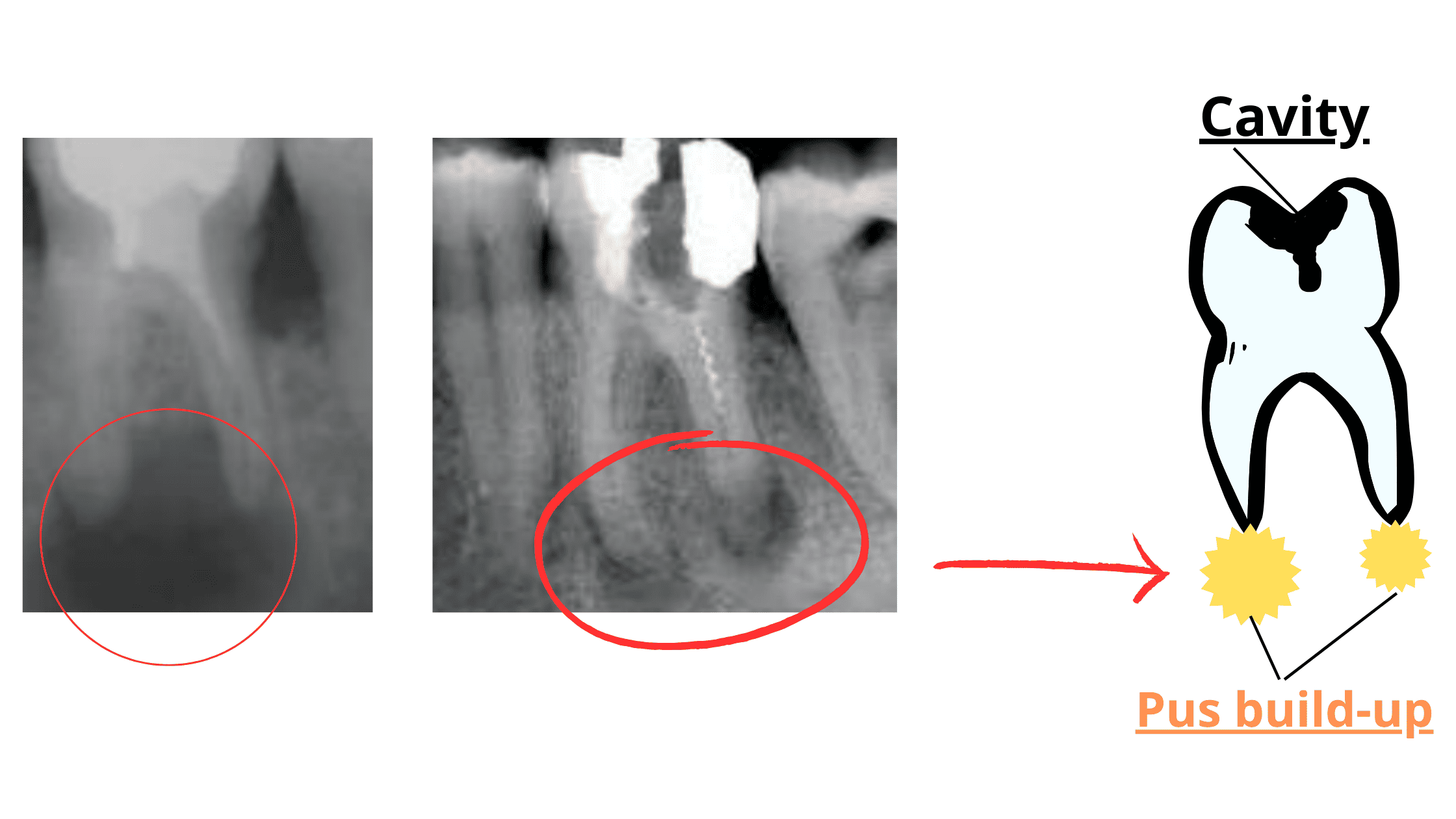
3. Gum abscess or boil near the treated tooth:
A gum abscess, often called a gum boil, is a well-localized swelling that appears when either a tooth or the surrounding gums become infected.
If it develops near a tooth that has undergone a root canal, there's a high chance that the infection has returned.
Common symptoms include pain, swelling, redness, bad breath, and sometimes pus discharge.
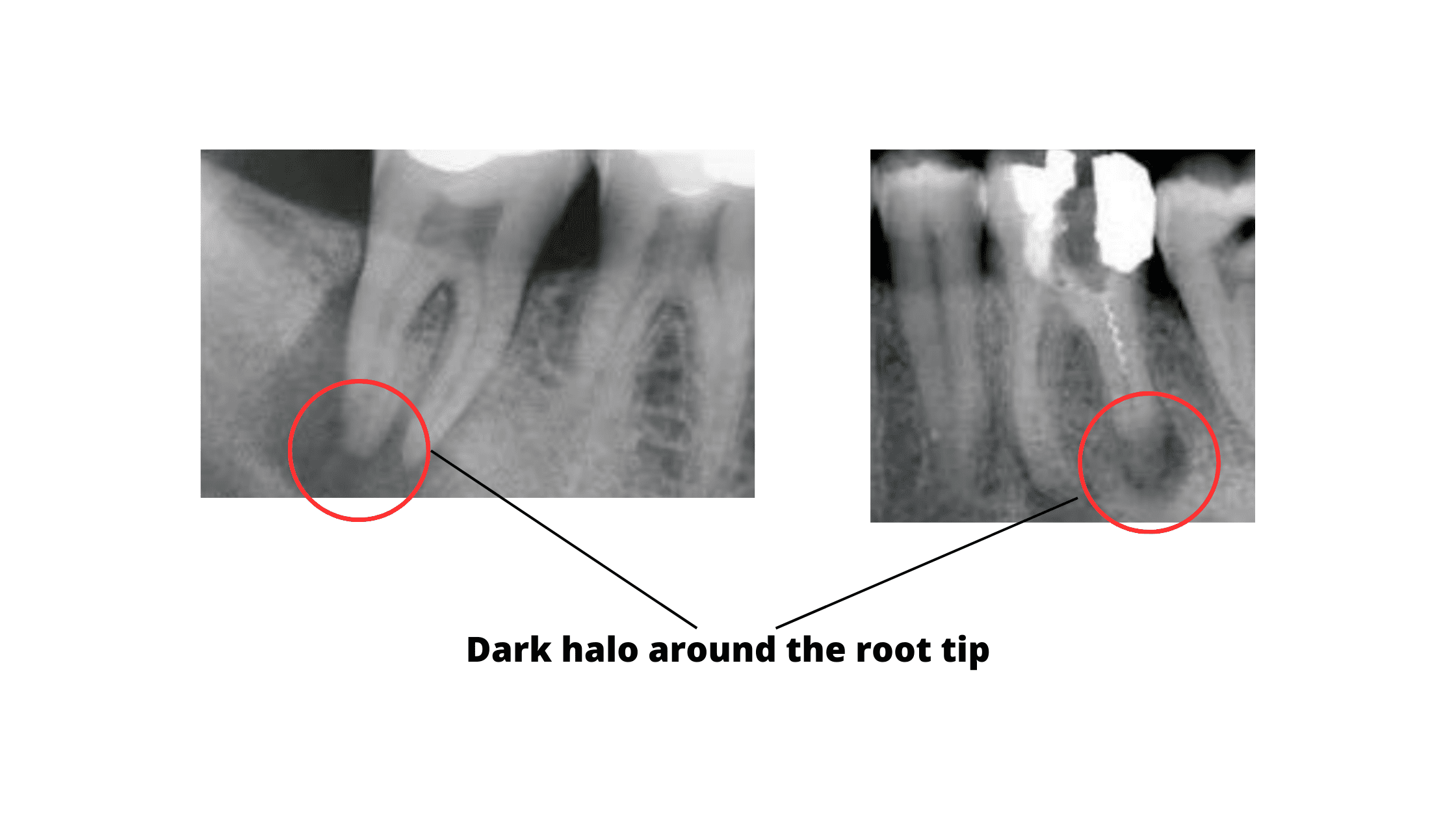
On X-ray, the abscess appears as a dark halo around the root tip.
How do you know if the tooth has healed properly?
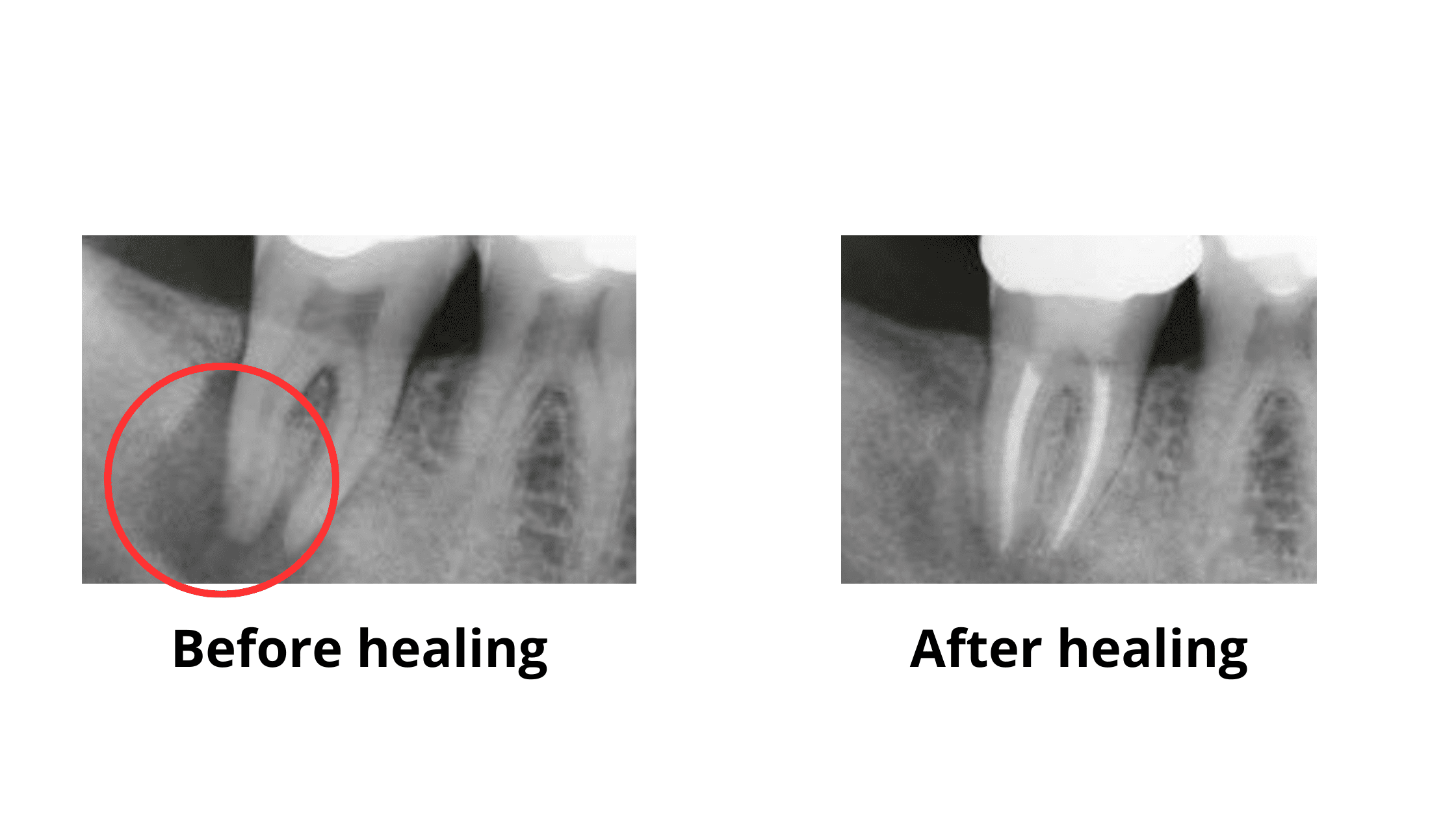
When checking if your root canal treatment was successful, there are two main things to look for:- No pain or discomfort – Your tooth should feel normal, with no signs of pain, swelling, or sensitivity.
- Healing on X-rays – The dark area around the root tip (often seen before treatment) should shrink or disappear over time. This means the bone is healing and the infection is clearing up.
 Just because you’re not feeling any pain doesn’t always mean your root canal was successful.
Just because you’re not feeling any pain doesn’t always mean your root canal was successful.
Sometimes, an infection can silently develop around the root tip without any symptoms — and the only way to catch it is with an X-ray.
If this hidden infection goes unnoticed, it can flare up later and cause serious pain.
That’s why follow-up appointments are so important.
They’re usually scheduled every six months after the treatment to monitor the healing process and spot any problems early.
Can a tooth with a failed root canal be saved?
If you’ve had a root canal in the past and your symptoms return, it could be a sign that the treatment has failed. But don’t worry — there are still ways to save your tooth.1. Root Canal Retreatment
This is the most common first step. The dentist will remove the old filling material, clean the canals again, and refill them properly. It gives your tooth a second chance to heal, especially if something was missed the first time.
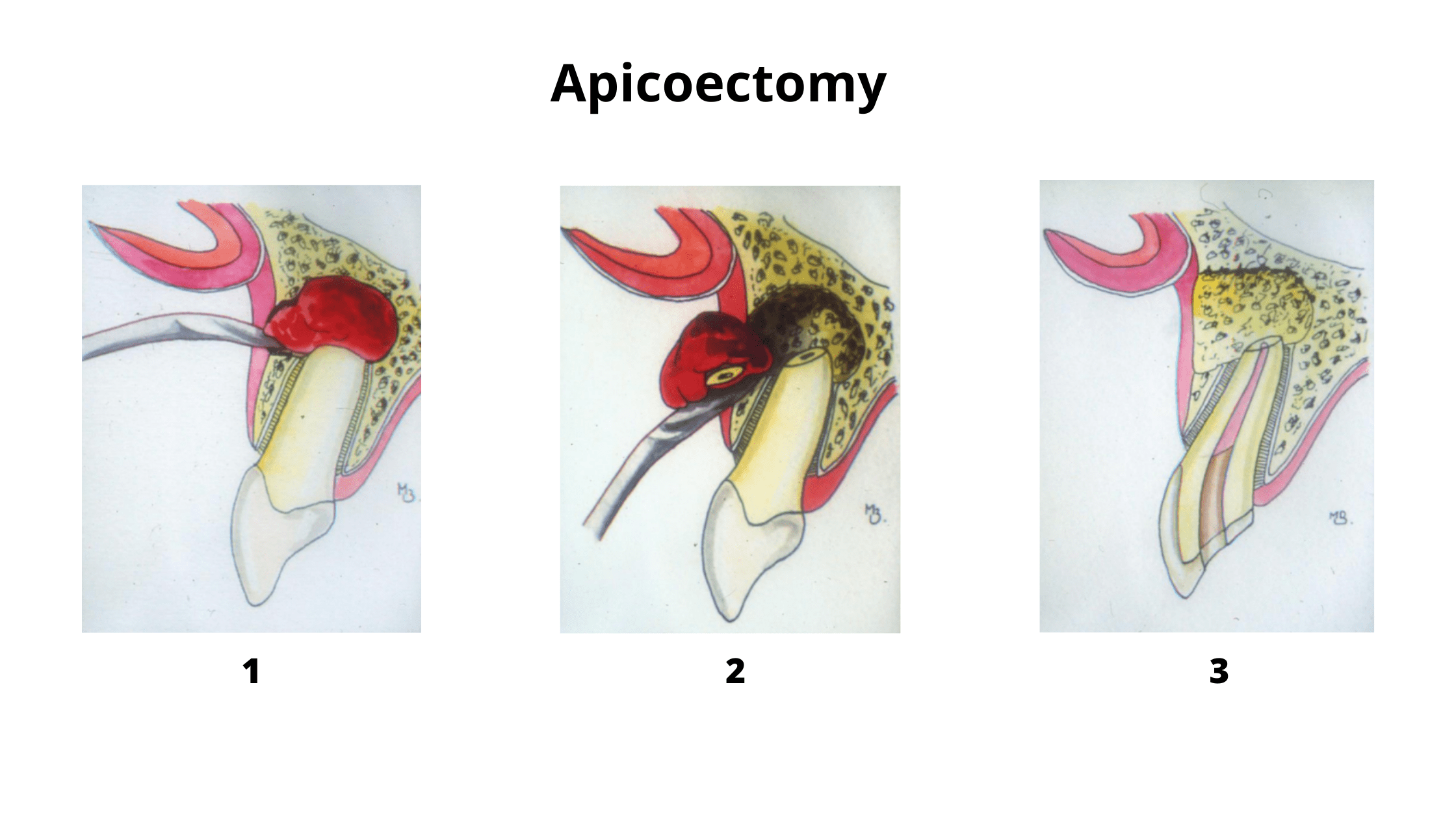
2. Apicoectomy (Surgical Root Repair)
If retreatment isn’t enough, your dentist might recommend an apicoectomy. This minor surgery removes the tip of the root and any nearby infected tissue. The end of the root is then sealed. Though it’s more invasive, it can be very effective in saving a tooth that would otherwise need to be extracted.
When is extraction the last option?
We always strive to preserve natural teeth whenever possible. However, in some cases, extraction may be necessary. This can happen if the tooth is severely damaged or if retreatment was not able to save the tooth. The most common situations include:- The tooth cannot be restored properly: If the tooth is too damaged or weakened, it may not be able to support a crown or filling. In this case, extraction may be the best option to prevent further damage to the surrounding teeth and gums.
- Root fracture: This injury can occur during or after root canal treatment, and unfortunately, it can be difficult to repair. If the fracture is severe, extraction may be the only option to prevent infection and further complications.
- Advanced gum disease: Gum or periodontal disease can also lead to tooth extraction. As gum disease progresses, it can cause the bone that supports the tooth to resorb. This can cause several complications, such as loosening, tooth loss, and abscesses.
- What is endodontic success? How successful is endodontic therapy? https://www.aegisdentalnetwork.com/cced/2017/03/
- Failure of endodontic treatment: The usual suspects https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4784145/
- Clinical and pharmacological management of endodontic flare-up https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3467928/
- New Approach in the Management of Vertical Root Fracture with the Help of Biodentine and CBCT https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7509562/