Abscess under Root Canal: Don't Ignore It!
When your tooth is infected, a common solution is root canal treatment. It helps save your natural tooth by removing damaged parts. Otherwise, it would have to be removed, which isn't the best option as nothing can replace your natural teeth (not even implants).
But what if the infection comes back or an abscess forms after a root canal? That's what we're exploring in this article.
But what if the infection comes back or an abscess forms after a root canal? That's what we're exploring in this article.
In this article:
1. The Main Goal of Root Canal Treatment
2. Why are Root Canal Teeth Not Immune to Infections or Abscesses?
3. The Different Types of Infections After Root Canal Treatment
4. The First Signs of an Abscess Under a Root Canal Tooth
5. What Does an Abscess Under a Root Canal Look Like on X-ray?
6. What's the Next Step?
The Main Goal of Root Canal Treatment
The main goal of a root canal treatment is to save a tooth that's been infected. We want to remove all those bacteria that have invaded your tooth, causing you pain and discomfort.But it's not just about providing relief. By clearing the infection, your tooth can be saved and can continue to do its job for years to come.
The root canal treatment should also protect the tooth from future problems. By cleaning, filling, and restoring it, we make sure there are no open gaps where bacteria can sneak in.
Ultimately, once the treatment is done, we want your tooth to be symptom-free. It shouldn't give you any discomfort and must function properly like any other healthy teeth.
Why are Root Canal Teeth Not Immune to Infections or Abscesses?
When we think of dental infections, we often associate them with the nerve's response to a deep cavity. However, that's not always the case, as even teeth without nerves can get infected.A perfect example is root canal-treated teeth. They lack nerves, yet can still be targets for bacteria, leading to abscesses.
The good news is that the risk of this happening is too low. When the root canal is well-executed, there is a good chance that the tooth will stay healthy for decades.
Even if treatment fails, it's typically not the fault of the root canal procedure itself. Other factors, such as cavities, gum disease, or fractures, are more likely culprits leading to the need for tooth removal.
Some of the causes of a tooth abscess under a root canal include:
- The initial infection isn't completely resolved: If the infection is too severe, bacteria can sometimes remain inside the root canals even after treatment. They can grow and spread to nearby tissues, causing ongoing pain and infection that may develop into an abscess.
- The root canal filling is leaking: The root canal filling must tightly seal the tooth, leaving no space for saliva and bacteria. Otherwise, the tooth can become infected and symptomatic again.
- The tooth is not properly restored: One of the major factors leading to complications after root canal treatment is not restoring the tooth in time. Placing a crown or filling as early as possible is essential to prevent fractures and protect the tooth from the bacteria-rich mouth.
- The tooth broke off: Cracks or fractures in a tooth give bacteria an easy way to reach the tissues around it. This can cause deep infections, which can lead to treatment failure. Teeth that have had a root canal are even more at risk of breaking because they’ve already lost much of their natural structure.
- Cavities and gum disease: Neglecting brushing and flossing regularly leads to more plaque buildup—the main culprit behind cavities and gum disease. Root canal-treated teeth are more vulnerable to cavities, and as bacteria progress, they can cause issues such as infection and even tooth loss.
Tooth decay and gum disease are more likely to cause a root canal to fail than problems with the treatment itself.
The Different Types of Infections After Root Canal Treatment
When a root-canal-treated tooth develops an infection, it usually happens in the area around the root tip (periapical area). This condition is termed periapical periodontitis.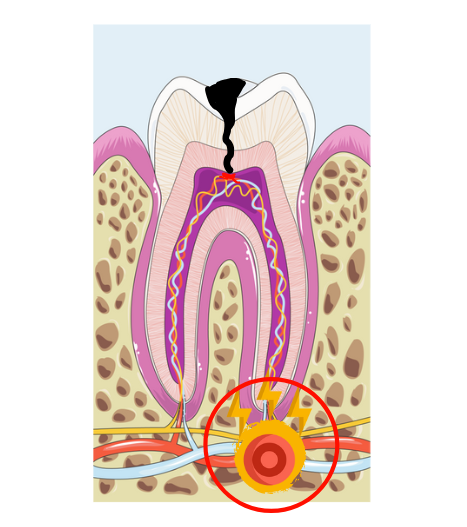
As pus accumulates around the root tip, it can travel to the gum tissue, leading to a visible swelling known as a gum abscess or gum boil.
The time it takes for an infection to show up after a root canal can vary from a few hours to several years. It depends on factors like the quality of the treatment, whether the restoration was delayed, the condition of the tooth before the procedure, and your body’s response to bacteria.
Overall, there are three possible scenarios:
- New Infection: This occurs when the root canal creates a pathway for bacteria to enter deep into the tooth, forming a new lesion that wasn’t there before. This is often due to a technical mistake made during the procedure. Pain is usually felt immediately, soon after the numbness wears off.
- Persistent Infection: This happens when the initial infection doesn’t fully heal or persists after treatment. It’s more likely in teeth with complex root canal anatomies (especially those with multiple roots) or when a canal is accidentally missed. A common sign is pain that continues longer than expected.
- Relapsing Infection: In this case, the tooth initially begins to heal, but bacteria later find a way back in, causing recurring symptoms. This type of infection is usually chronic, developing slowly over months or even years. It is more likely if the tooth isn’t restored in time.
The First Signs of an Abscess Under a Root Canal Tooth
The first symptom is often severe pain that gets worse with pressure, like when you bite down or touch the tooth.But mild to moderate pain right after treatment is completely normal and expected. It should gradually improve over the first week as healing progresses.
What’s abnormal is if the pain worsens or suddenly reappears after it has initially improved.
Patients also often notice that their tooth feels different when biting, even weeks or months later. This can be normal, as the underlying bone takes longer to heal. However, it’s important to follow up with your dentist every six months to monitor healing and rule out complications.
Here are some common signs and what they may indicate:
- Pimple or swollen gums with severe pain: Classic signs of an abscessed tooth.
- Pain that increases only when releasing the bite: Could indicate a root fracture, a common complication after a root canal.
- Pain only with cold or acidic foods and drinks: The infection may actually be coming from a nearby tooth, not the treated one.
- Mild pain that gets worse when biting down: Can be normal, especially during the first week after the procedure. It should gradually fade over this period.
The infection can be silent:
Pain isn't always the sole indicator. In cases of chronic infection, you may not feel anything abnormal. Only a dental X-ray can reveal a hidden infection.
Signs of advanced abscess:
When the infection flares up and an abscess forms beneath the tooth, the pain can become intense, throbbing, and unbearable. It may even prevent you from sleeping or eating. Other signs include an unpleasant taste, bad breath, pus leakage, a sensation that the tooth feels “too long,” swelling, and sometimes fever.
Never delay treating a tooth infection. It won’t heal on its own and will only get worse. The sooner you get treatment, the better the chance of saving the tooth and preventing serious complications.
What Does an Abscess Under a Root Canal Look Like on X-ray?
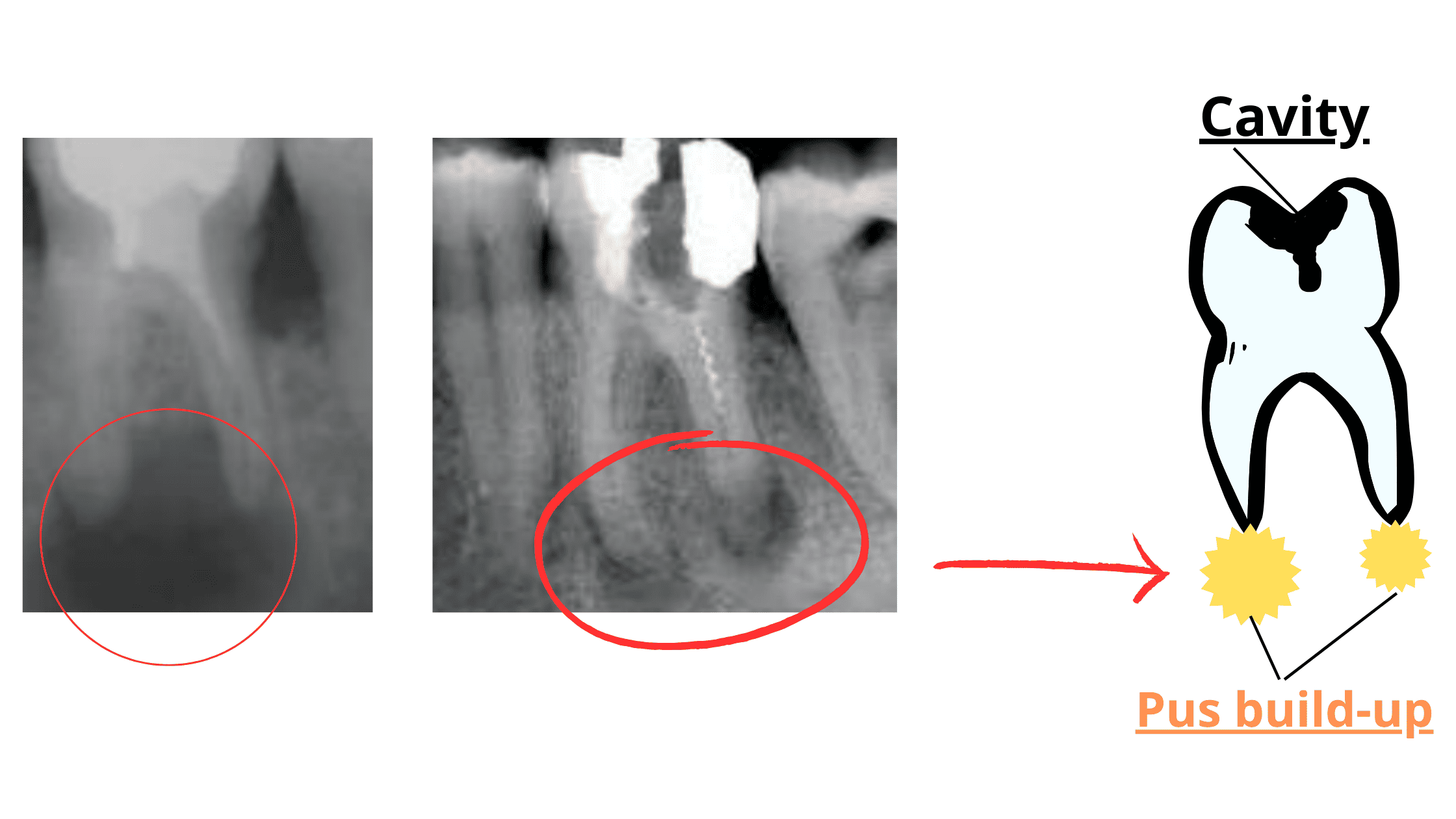 On the X-rays above, you can see a dark halo around the root tips. This halo indicates pus buildup and bone loss in the area around the root tip.
On the X-rays above, you can see a dark halo around the root tips. This halo indicates pus buildup and bone loss in the area around the root tip.
This is only the first stage of the abscess. If left untreated, it can spread further, destroy more bone, and may eventually lead to tooth loss.
What's the Next Step?
Never delay treating a dental infection or abscess. Get treatment as soon as possible to stop it from getting worse.The infection can spread to the jawbone or other areas of the face and neck, causing swelling, difficulty breathing, fever, pus buildup, and swollen lymph nodes.
Like other infections, bacteria can enter the bloodstream and affect vital organs such as the heart, brain, or lungs. In rare cases, it can lead to sepsis—a life-threatening condition that can cause a sudden drop in blood pressure and organ failure.
The best course of action is to treat the infection early, before it becomes life-threatening.
Here’s how your dentist can manage an abscessed tooth:
How is an abscess under a root canal managed?
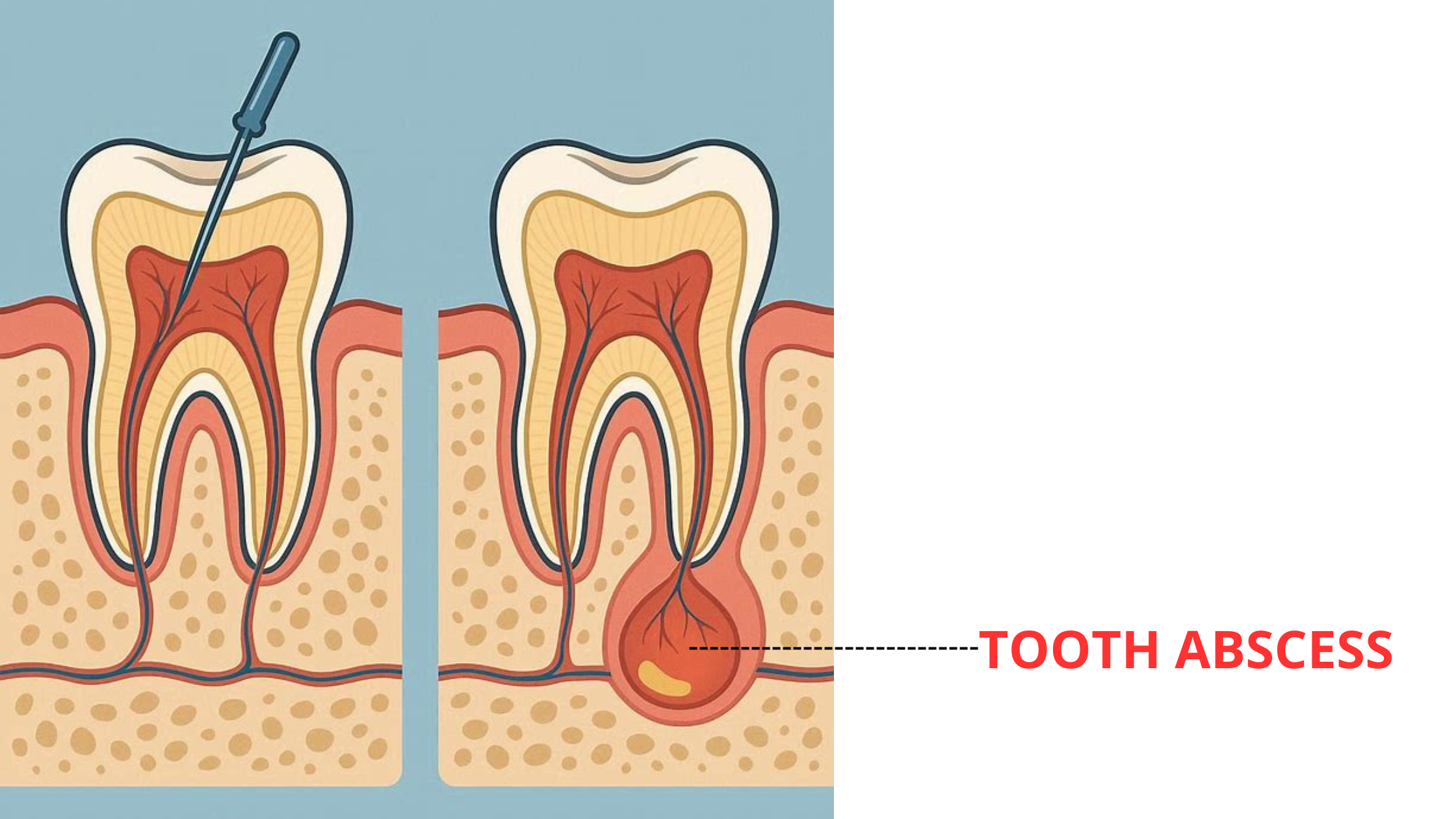
Your dentist will first evaluate the tooth's condition and take X-rays to determine if a root canal retreatment is possible.
If the tooth can be saved, the old filling will be removed to drain the abscess. A new root canal treatment (retreatment) will be done to clean, reshape, and fix the tooth.
What if root canal retreatment isn't possible?
Sometimes, root canal retreatment is impossible or insufficient to get rid of all the infection. In such cases, a minor surgery called apicoectomy or root-end surgery may be needed. This procedure, conducted by an endodontist, involves cutting the gum and drilling through the bone to expose the root tip for direct visual access to the infection.
Extraction as a Last Resort
When a tooth is severely infected or damaged, removing it may be the last option. After extraction, you can think about options like a dental bridge or implant to replace the missing tooth.