Apicoectomy: The Tooth-Saving Procedure You Need to Know About
 Root canal treatment is highly successful and can save your tooth for many years. Studies show that root-canal-treated teeth have a long-term survival rate of up to 97%.
Root canal treatment is highly successful and can save your tooth for many years. Studies show that root-canal-treated teeth have a long-term survival rate of up to 97%.
But what if a root canal fails? Does that mean you’ll lose your tooth? Not necessarily—this is where an apicoectomy can offer your tooth a second chance.
Also known as root-end surgery, apicoectomy is a type of endodontic surgery that has greatly improved over the years thanks to modern techniques and tools.
In this article, we’ll cover when an apicoectomy is needed, how the procedure works, and what the healing process looks like—so you’ll know exactly what to expect.
In this article:
1. What is Apicoectomy?
2. When do I need an apicoectomy?
3. How the apicoectomy procedure works
4. Healing and recovery:
5. How successful apicoectomy is?
6. What if apicoectomy fails to heal the tooth?
7. Risks and complications of apicoectomy:
What is Apicoectomy?
Apicoectomy, also known as endodontic surgery or root end surgery, is a surgical approach often used to treat a tooth infection. It's typically the last resort to save a damaged tooth from being extracted.Apicoectomy gets its name because it involves removing a small portion of the tooth’s apex—the very tip of the root.
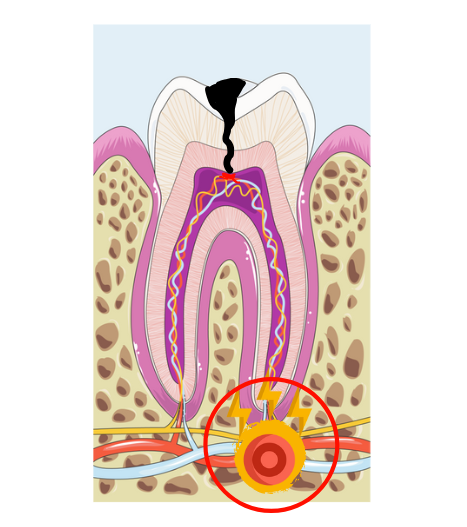
This procedure is usually needed when an infection has reached the root tip and isn’t healing, even after a regular root canal. The infection becomes persistent and too deep in that area, and the only way to resolve it may be to remove the infected root tip along with the surrounding tissue.
When do I need an apicoectomy?
Apicoectomy has long been considered the last resort to save the tooth. This is because, in the past, surgery with its traditional techniques had a lower success rate. In most cases, non-surgical root canal retreatment was the best option, as it had greater chances of saving the tooth.However, that’s no longer the case today. Thanks to modern techniques and the rise of endodontic microsurgery, apicoectomy is now considered a first-line option in certain cases. In fact, some studies have shown that its success rates can even exceed those of conventional retreatment (2).
Here are the most common situations where an apicoectomy may be needed:
1. Root canal retreatment has failed:
If a tooth doesn’t heal despite a well-performed root canal, it usually means the infection is deep, persistent, and can’t be reached through conventional methods. In such cases, surgery allows the dentist to access the root tip directly, remove the entire infection, and know what prevented healing in the first place.
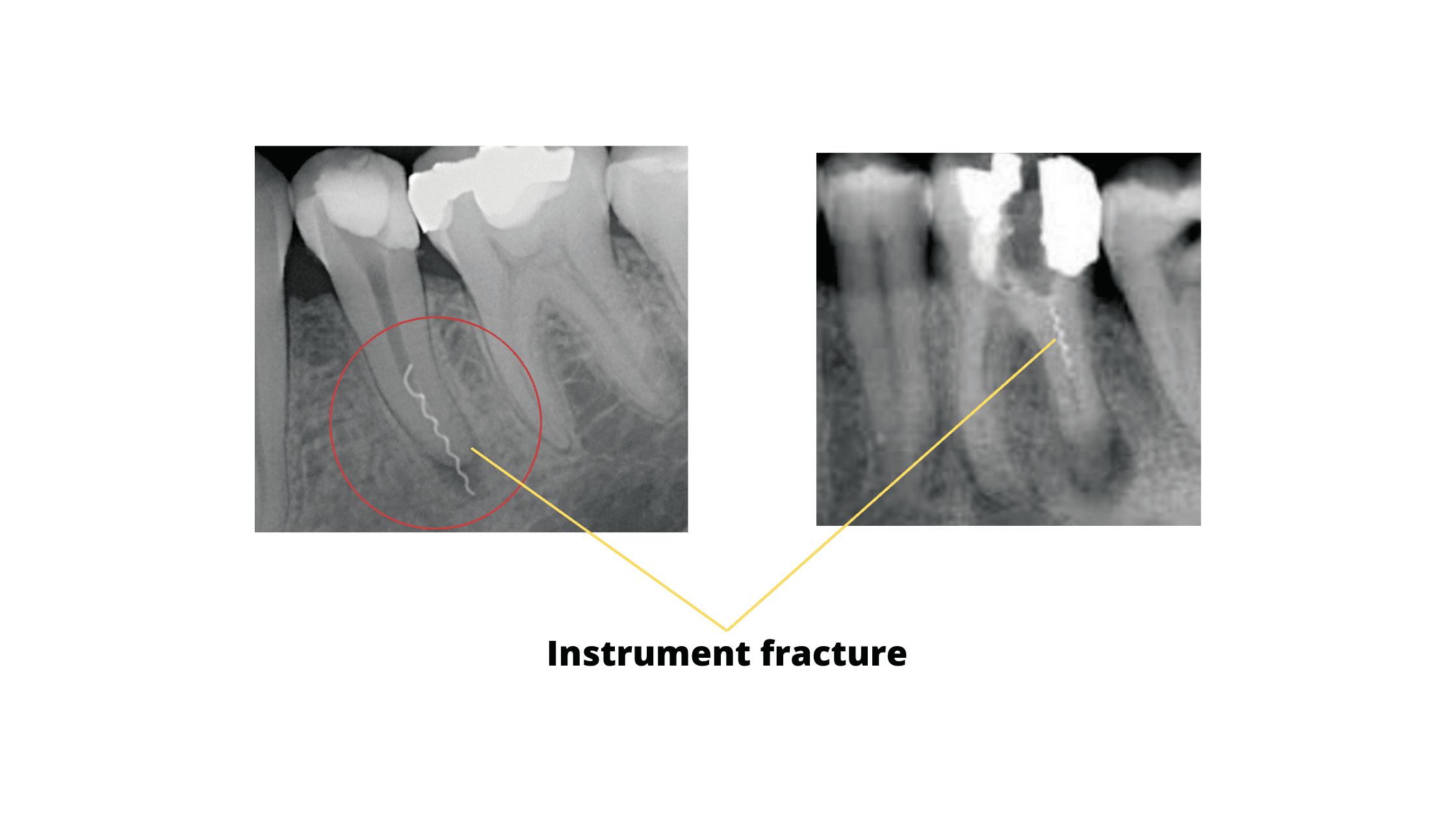
2. Technical errors during root canal treatment:
Some professional mistakes can block the tooth's canal, preventing its complete cleaning and shaping.
These errors include the fracture of an instrument inside the root canals (see X-rays below), perforation of the root, or overextension of filling material beyond the root tip.
All of these factors can lead to treatment failure and the need for an apicoectomy.
3. For anatomical reasons:
Sometimes the tooth canal is too curved or has calcifications - a pulp degeneration process - that makes it difficult to use endodontic tools properly. This can make the surgical approach the only way to access these hard-to-reach areas to clean and shape the entire canal system.
4. The tooth carries a well-fitting post or crown:
The first drawback of traditional root canal retreatment is that it first requires removing the existing restoration, such as a crown or post.
If your current restoration fits well and you're happy with it, retreating the root canal could damage or weaken the tooth further.
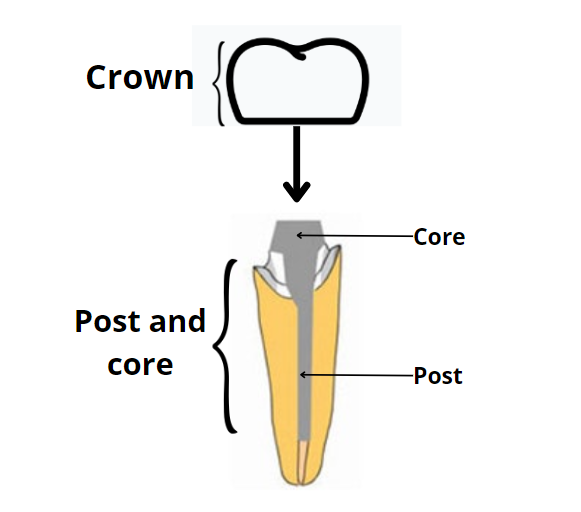 Apicoectomy allows the root canal to be retreated without damaging or even removing your dental crown. This can save you time and money, and it also reduces the risk of weakening the tooth.
Apicoectomy allows the root canal to be retreated without damaging or even removing your dental crown. This can save you time and money, and it also reduces the risk of weakening the tooth.
5. Cyst:
A cyst is a fluid-filled cavity that forms at the root tip due to a chronic infection. Sometimes it persists or reappears after root canal therapy. In this case, an apicoectomy may be needed to remove it and prevent it from coming back.How the apicoectomy procedure works
Modern tools like dental microscopes, advanced biomaterials and lighting have made apicoectomy simpler and more effective. These have also increased the procedure's success rates over the years.The procedure can be performed by an endodontist, oral surgeon, or a trained general dentist.
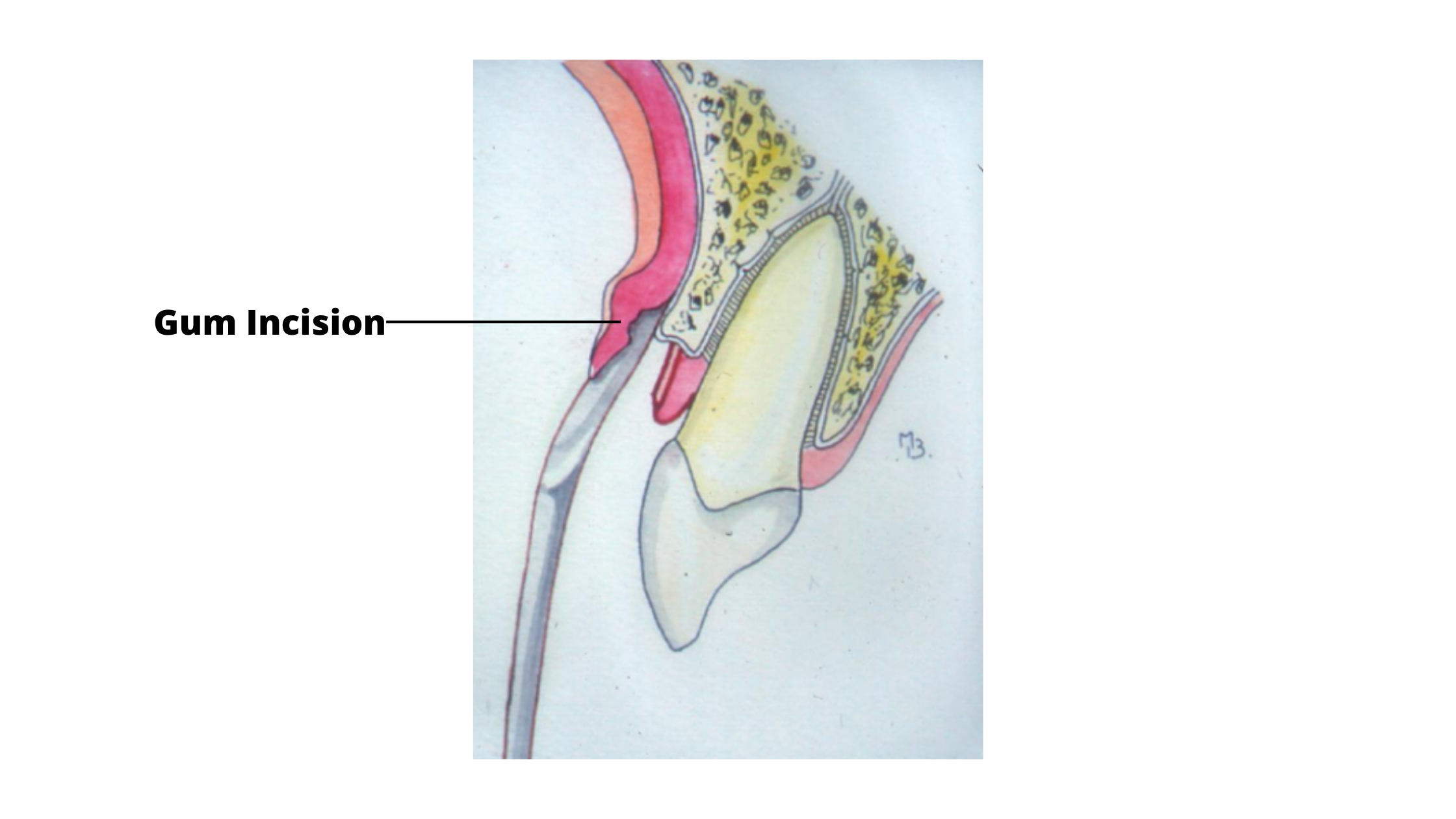
It starts with numbing the area around the tooth using local anesthesia. Once the area is fully numb, the procedure is typically done in three main steps:
- Soft tissue step
- Hard tissue step
- Root tip step
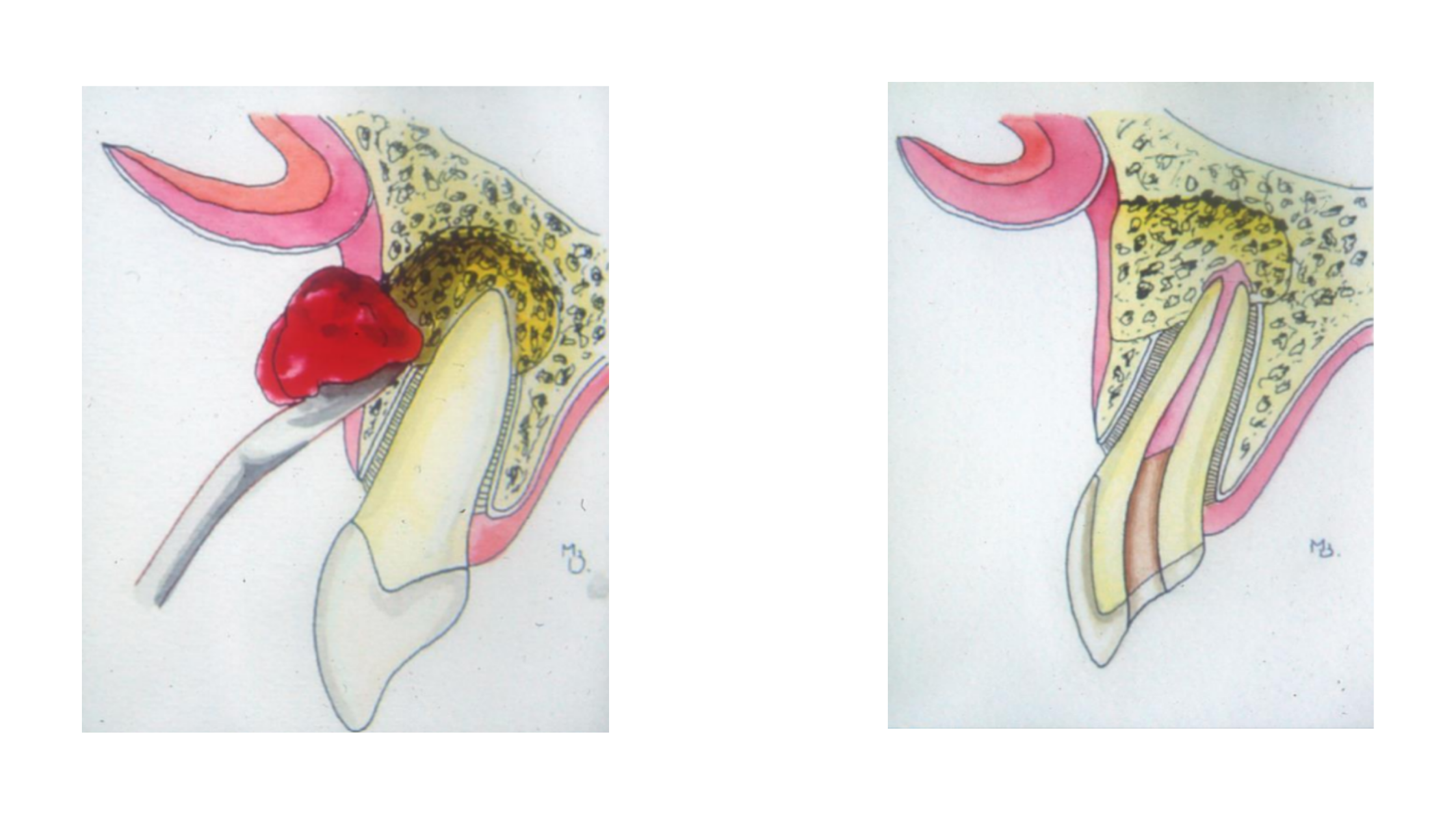
- Soft tissue step: This step involves cutting the gum tissue and gently moving it aside to expose the bone surrounding the tooth that needs treatment.
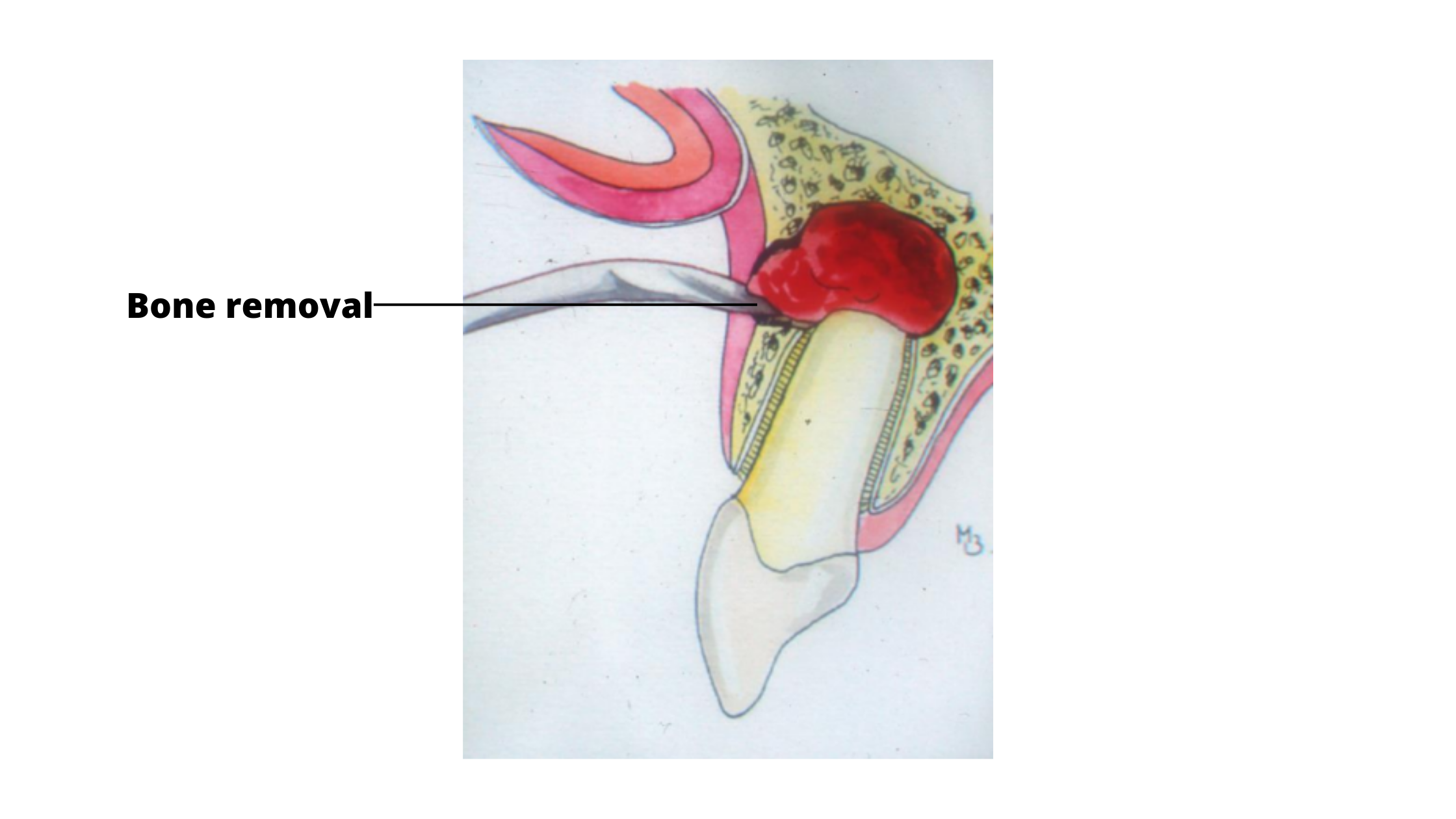
- Hard tissue step: A small portion of the bone covering the tooth is drilled away to expose the root tip (apex). This gives the dentist direct access to remove all infected and inflamed tissue while preserving as much healthy bone as possible.
- Root tip (apex) step: A small portion of the tooth’s apex is removed. The dentist then uses specialized tools—such as high-frequency vibration instruments—to clean and prepare the root canal from the tip.
Afterward, the root tip is sealed with a biomaterial. Filling the canal from this end helps prevent further infection and promotes healing and tissue repair.
It’s now possible to treat the entire root canal system through the apex, which means you no longer need to remove a well-fitting crown for retreatment.
Healing and recovery:
Apicoectomy is a minor surgical procedure and doesn’t lead to a difficult recovery period.However, some post-operative effects are normal and expected, such as temporary swelling, minor bleeding, and mild discomfort—especially during the first few days.
Here are some helpful tips to ease these symptoms and support your healing process.
- For the first 24 hours, apply ice to the affected area with gentle pressure. Use ice packs for 20 minutes, then take a 10-minute break, and repeat. This helps reduce pain and swelling.
- If you experience bleeding, gently press a gauze pad against the area for 15 minutes. If the bleeding doesn’t stop, contact your dentist for help.
- Don't touch the wound with your tongue or finger during the first few days to prevent tearing the stitches.
- After the first 24 hours, rinse your mouth several times a day with warm salt water to keep the area clean.
- Stick to soft foods for a few days and chew on the opposite side.
- Don't smoke for at least the first one or two weeks.
- Take the medication as directed. Visit your dentist to have the sutures removed, typically within 5 to 7 days.
The healing process
Your gums usually heal quickly and return to their normal appearance within the first week.
The underlying bone takes longer to heal and may require several months to fully repair.
Don't miss your follow-up appointments with your dentist. These visits are important to monitor your healing and check for any potential complications.
If you notice any unusual symptoms—such as fever, pus leaking from the gums, or heavy bleeding—contact your dentist right away.
Mild swelling and discomfort are normal during the first few days. After the first week, healing usually progresses smoothly, and complications are rare.
How successful apicoectomy is?
The success of apicoectomy depends on several factors, including the condition of your tooth, your age and overall health, and your dentist’s experience.Overall, apicoectomy is very effective and can save your tooth for many years—much like a regular root canal treatment.
However, predicting the exact outcome can sometimes be challenging, especially if the tooth is severely damaged.
Despite this, the procedure is often worth trying because nothing can truly replace your natural teeth.
Many studies have shown that when performed correctly with modern tools, apicoectomy success rates are very high—comparable to, and sometimes even better than, traditional root canal retreatment.
Here’s what some research reports:
- 91.2% success rate with follow-up periods up to 4 years (4).
- 95.3% success rate after one year (7).
- Tooth survival rates after root-end surgery were 93.7% at 2 years, 90.5% at 4 years, and 88% at 6 years (6).
What if apicoectomy fails to heal the tooth?
According to one study, technical errors during surgery—such as incomplete removal of the root tip, poor filling, or leaving infected tissue behind—are among the most common causes of failure.That’s why this procedure should preferably be performed by a specialist with extensive experience in apicoectomy.
However, if the tooth is badly damaged, with fractures, deep decay, or is otherwise beyond repair, an apicoectomy may not be enough to save it. In such cases, extraction might be the last option.
After extraction, you can replace the missing tooth with a dental implant or a bridge to restore function and appearance.
Risks and complications of apicoectomy:
Apicoectomy is a safe and effective procedure, but like any surgery, it carries some risks.Common side effects include mild and temporary swelling, pain, and bruising at the surgical site. Again, these are normal and temporary.
Rare but possible complications include excessive bleeding and infection.
Watch out for signs such as increasing swelling or pain, bad breath or bad taste, pus discharge, and fever.
Certain medical conditions and factors that weaken the immune system, such as diabetes, smoking, and chronic illnesses, can increase these risks. In some cases, these factors may even make you ineligible for the surgery.
During the procedure, there is a small risk of damage to nearby structures like nerves, sinuses, or blood vessels. Fortunately, these complications are rare, and when they do occur, they are usually manageable.
- What is endodontic success? How successful is endodontic therapy? https://www.aegisdentalnetwork.com/cced/2017/03/
- Is Retreatment Always Necessary Before Endodontic Surgery? https://www.aae.org/specialty/is-retreatment-always-necessary-before-endodontic-surgery/
- Possible Causes for Failure of Endodontic Surgery – A Retrospective Series of 20 Resurgery Cases https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8461483
- Prognosis in periradicular surgery: a clinical prospective study https://pubmed.ncbi.nlm.nih.gov/11307456/
- Prognostic Factors in Endodontic Surgery Using an Endoscope: A 1 Year Retrospective Cohort Study https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8461483
- Root-end Surgery or Nonsurgical Retreatment: Are There Differences in Long-term Outcome? https://pubmed.ncbi.nlm.nih.gov/33961913/
- Prognostic Factors in Endodontic Surgery Using an Endoscope: A 1 Year Retrospective Cohort Study https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9103390/
- Endodontic Microsurgery: The Significance of Soft Tissue Management in Overall Success https://www.aae.org/specialty/management-of-soft-tissue-in-microsurgical-endodontics/
- Tissue conservation in endodontic microsurgery https://www.sop.asso.fr/admin/documents/ros/ROS0000226/2072.pdf