Periodontal Bone Grafting: A Regenerative Approach for Gum Disease
Periodontal disease can have disastrous effects on the bone and gums that support your teeth.
For a while, it was believed that once periodontitis caused bone loss, the damage was permanent. But thanks to advancements in regenerative dentistry—especially bone grafting—that’s no longer true.
Bone grafting offers a way to reverse some of the bone lost to gum disease. However, it’s not the right solution for everyone.
If you’re wondering how a bone graft could help in your case—and when is the right time for it—we’ll walk you through everything you need to know.
In this article:
1. How Can Periodontal Disease Damage Your Bone?
2. How Can Periodontal Bone Grafting Help with Gum Disease?
3. What Is the Best Time for Bone Grafting in Gum Disease?
4. Who Is the Most Suitable Candidate for Periodontal Bone Grafting?
5. The Types of Periodontal Bone Grafting
6. What Can You Expect After the Procedure?
7. Alternatives to Bone Grafting
8. Aftercare: Tips for a Smooth Recovery
How Can Periodontal Disease Damage Your Bone?

Periodontal disease is the leading cause of tooth loss in adults.
It begins when harmful bacteria overwhelm your immune system and start attacking the deep tissues that support your teeth—including the ligaments and the bone. This condition is known as periodontitis.
While periodontitis usually develops slowly over time, in some cases it can be aggressive, causing severe and rapid bone loss.
As the disease breaks down the supporting structures, your teeth may gradually loosen—and if left untreated, they can eventually fall out.
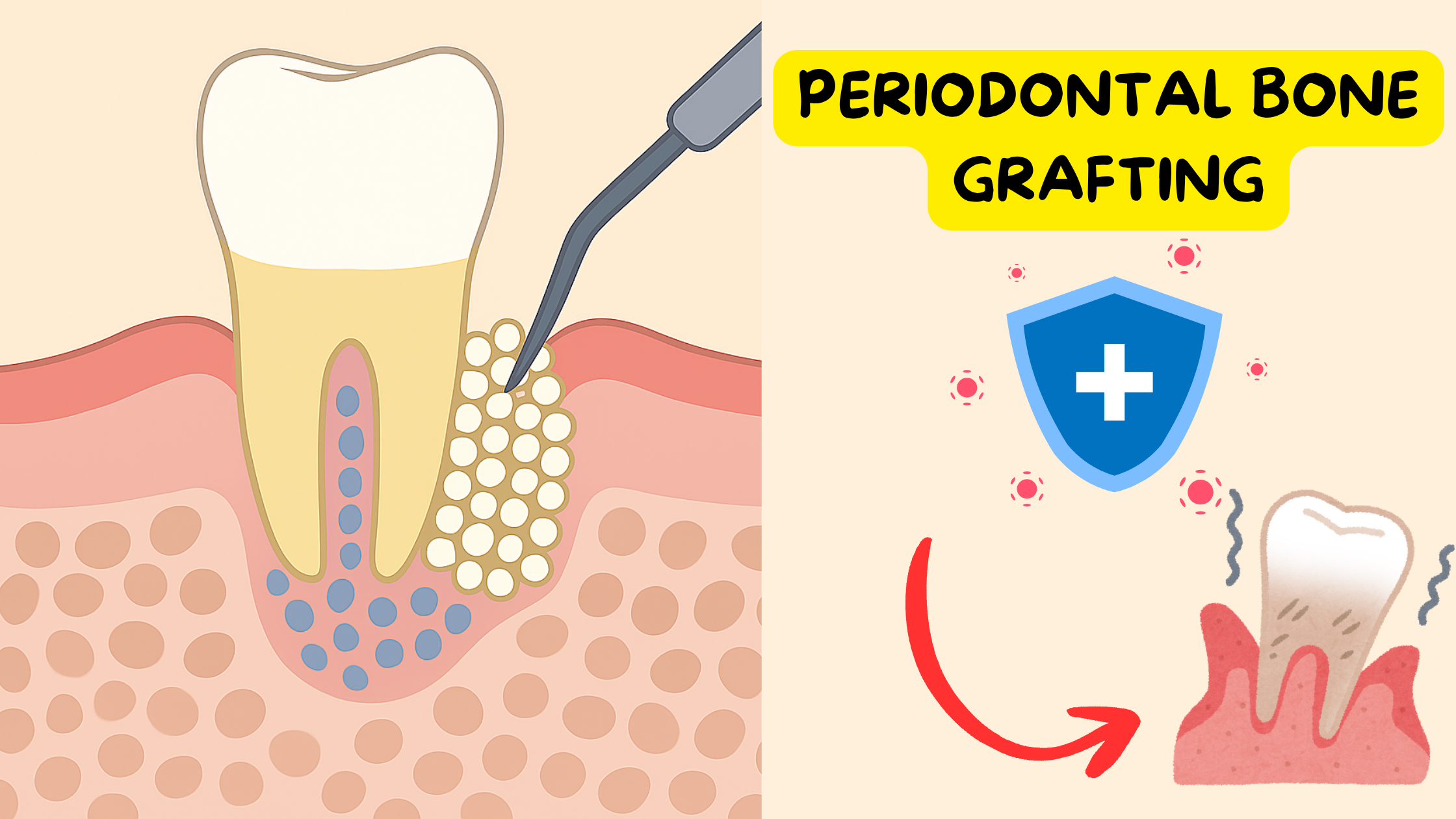
How Can Periodontal Bone Grafting Help with Gum Disease?
Periodontal bone grafting is a regenerative treatment for gum disease. In other words, it helps reverse some of the damage caused by supporting new bone and ligament formation.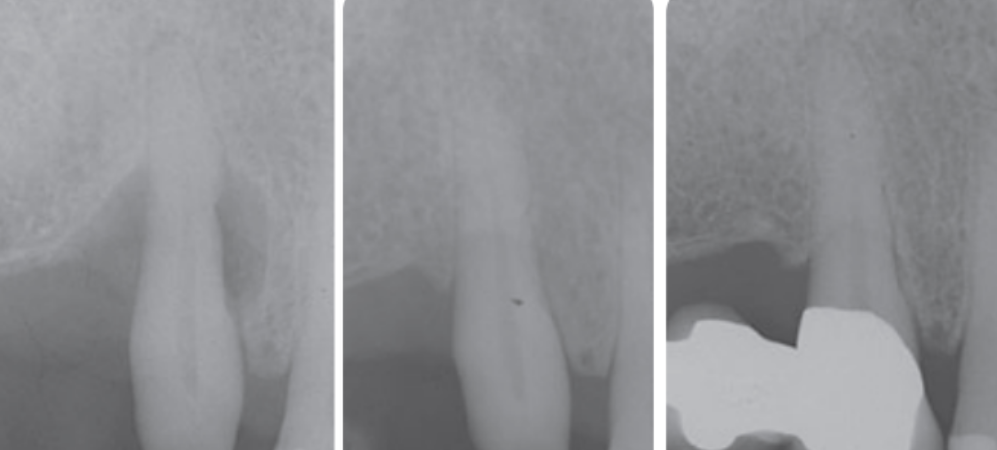
Periodontal bone graft before and after
Here’s what bone grafting can do:
- Improve the height and thickness of the damaged bone
- Promote the formation of new ligaments to better hold your teeth
- Help the gums reattach to the teeth and prevent them from receding
- Reduce periodontal pocket depths
- Stabilize loose teeth and help prevent tooth loss
However, bone grafting isn’t a stand-alone treatment for gum disease. It always follows non-surgical therapy—commonly known as deep cleaning (scaling and root planing). Deep cleaning is the standard treatment for most cases of gum disease.
This initial non-surgical step is crucial because it targets the root cause of the disease: bacteria and plaque buildup.
Bone grafting can be (but not always) considered next as a corrective step to repair the damage. This assumes that the infection is under control and the disease has been stabilized.
What Is the Best Time for Bone Grafting in Gum Disease?
Bone grafting—and other surgical treatments for gum disease—are not first-line therapies. They are complements to the initial non-surgical approach.So, bone grafting can only be considered once all the following goals have been achieved:
- Good oral hygiene habits
- Good plaque control
- Healthy, inflammation-free gums
- Stabilized periodontitis
- Infected tissue removed
In some cases, if your gums respond well to non-surgical therapy, you may not even need surgery.
Either way, non-surgical treatment must be successful before you can move on to periodontal bone grafting.
If the root cause hasn’t been addressed—or if the disease is still active—proceeding to surgery can lead to treatment failure.
Who Is the Most Suitable Candidate for Periodontal Bone Grafting?
Any tooth that has lost a significant amount of bone—but still has a good chance of survival—can benefit from a bone graft to extend its lifespan. The only exception is when the tooth is beyond repair or likely to be removed soon anyway.Depending on the shape of the bone defect, some cases are better candidates for bone grafting and have much higher success rates.
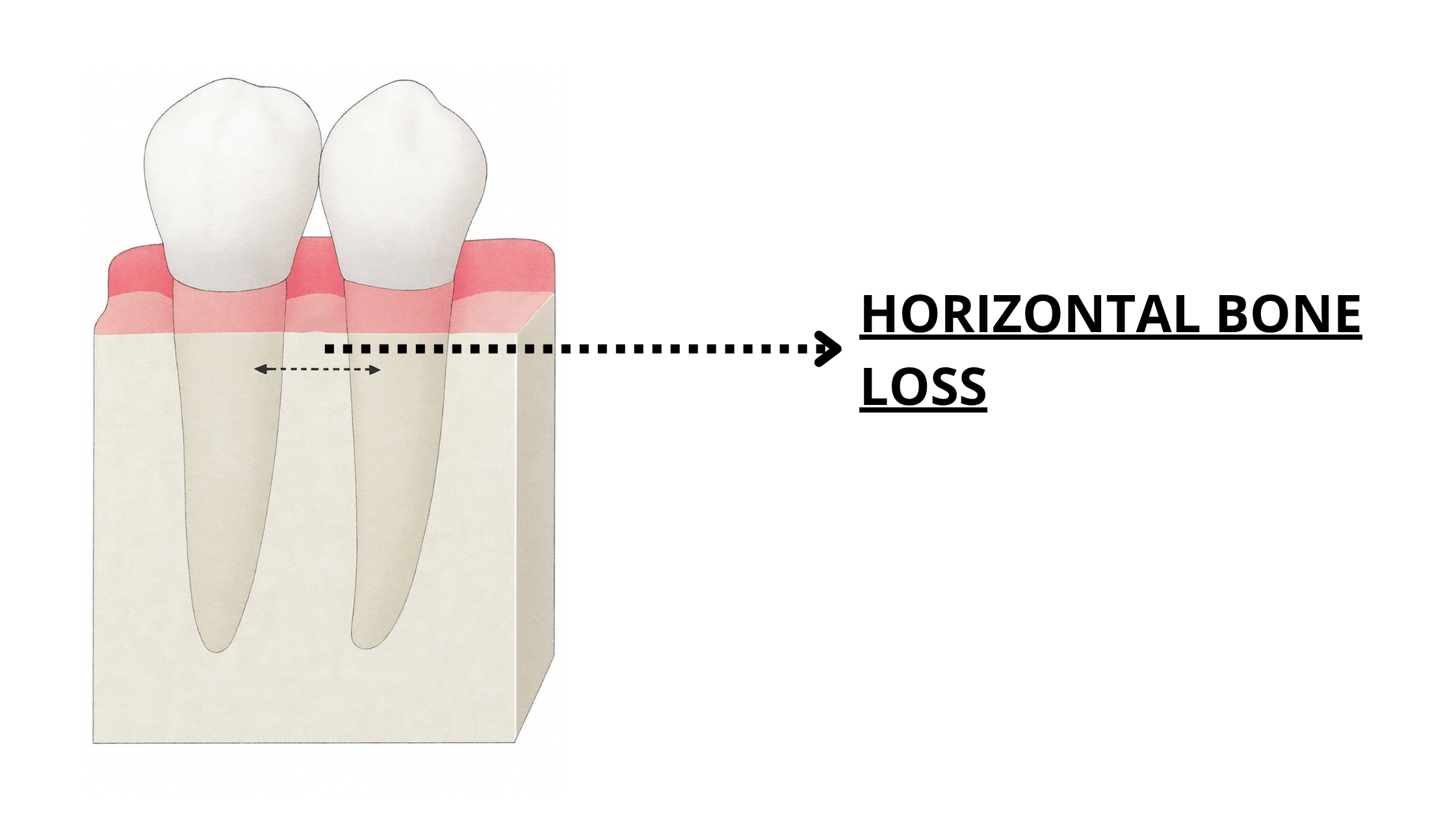
Bone loss from gum disease typically follows one of two patterns: horizontal or angular (as shown in the X-rays below).
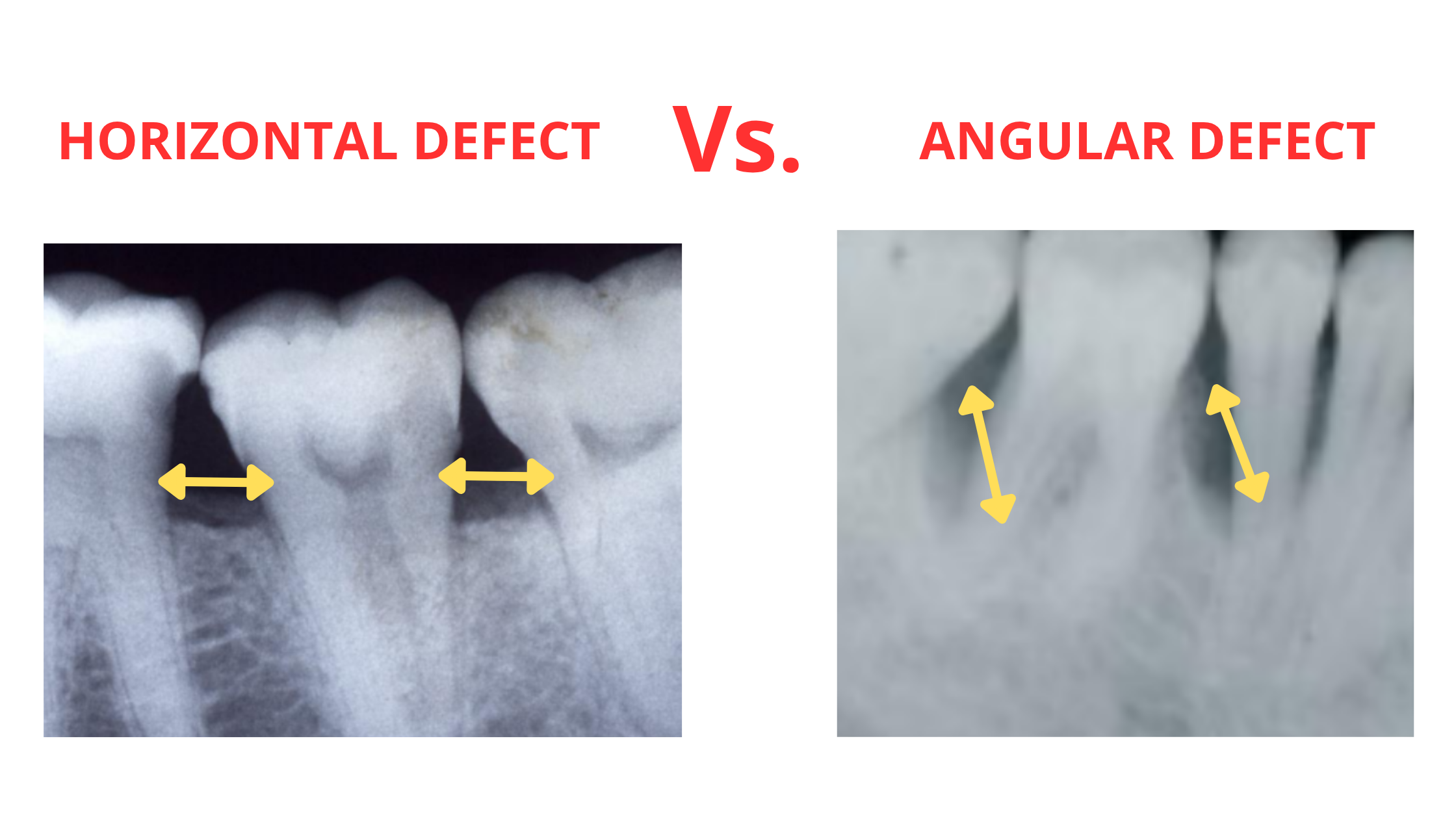
- Horizontal bone loss happens when the damage is flat and runs parallel to a line connecting two neighboring teeth.
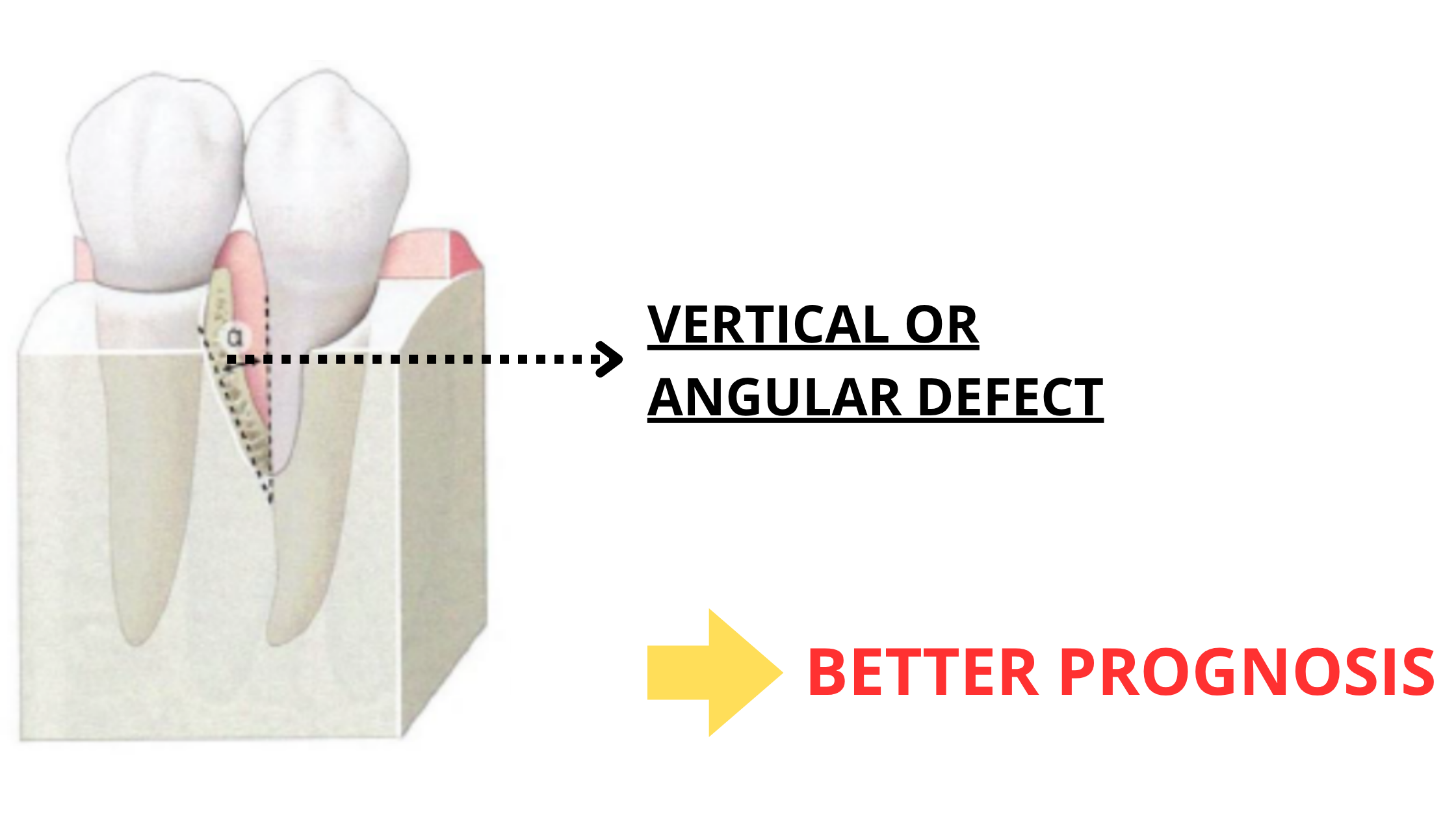
- Angular (or vertical) bone defects occur when the bone loss is uneven and angled toward one tooth. This means more bone is lost in one spot than in the other.
Periodontal bone grafting tends to work much better in angular defects than in horizontal ones.
Why? Because angular defects create natural bony walls that help contain and support the graft. It acts like a pocket that stabilizes the graft and helps it heal. The more bone walls there are, the better the chances of successful integration.
Horizontal defects, however, have only one flat surface at the top, which doesn’t provide enough support to hold the graft in place. As a result, grafting outcomes in these cases tend to be less predictable and less successful.
The Types of Periodontal Bone Grafting
Several types of bone graft materials can be used to fill bone defects and promote regeneration. These include:1. Autogenous bone graft:
 This is considered the gold standard because the bone comes from your own body—usually from your jaw—and contains living cells. This gives it the highest potential for periodontal regeneration.
This is considered the gold standard because the bone comes from your own body—usually from your jaw—and contains living cells. This gives it the highest potential for periodontal regeneration.
However, it requires a second surgical site or donor site, which may lead to a longer healing time and some discomfort.
2. Allograft:
 The bone is taken from another human donor (typically a cadaver) and sourced from bone banks. Before use, the bone is carefully processed and sterilized to eliminate any risk of rejection or infection.
The bone is taken from another human donor (typically a cadaver) and sourced from bone banks. Before use, the bone is carefully processed and sterilized to eliminate any risk of rejection or infection.
Although it doesn’t contain living cells, studies show that allografts can stimulate local cells to produce new bone, providing results comparable to autogenous grafts.
The biggest advantage is that no second surgical site is needed, which makes allografts more commonly used today.
3. Xenograft:
 These grafts come from another animal species (usually bovine or porcine). Like allografts, xenografts are thoroughly processed before use.
These grafts come from another animal species (usually bovine or porcine). Like allografts, xenografts are thoroughly processed before use.
They don’t stimulate new bone formation like autografts or allografts; instead, they act mainly as a filler or space maintainer. Over time, the body gradually breaks down the xenograft and replaces it with new bone.
4. Alloplast:
 These are synthetic materials such as bioglass, hydroxyapatite, and tricalcium phosphate. They are designed to look like natural bone.
These are synthetic materials such as bioglass, hydroxyapatite, and tricalcium phosphate. They are designed to look like natural bone.
Similar to xenografts, they promote bone regeneration by maintaining space but do not contain living cells or actively stimulate new bone growth.
Autografts and allografts have the highest potential for bone regeneration and are therefore the most commonly used. In contrast, alloplasts and xenografts mainly act as space maintainers and do not actively stimulate new bone growth.
What Can You Expect After the Procedure?
After periodontal bone grafting, it’s normal to experience some post-operative effects such as swelling, pain, bleeding, and redness around the surgical site. These symptoms typically improve gradually during the first week.Within that first week, your gums usually start to look and feel more normal. Sutures are generally removed after 7 to 10 days.
However, the healing of the bone itself takes longer. The process of the graft integrating and maturing can take several months.
Here’s a quick overview of the healing stages:
- Inflammatory response (first 3 days): This is your body’s natural reaction to surgery, causing swelling, redness, and some discomfort. These symptoms improve over the first week.
- Vascularization (starting from the first week): New blood vessels begin to form around and inside the graft, bringing oxygen and nutrients essential for healing.
- Resorption: Regardless of the graft type, your body needs to break it down to replace it with new bone. This phase can last several months.
- Maturation: The newly formed bone becomes stronger and fully integrates with your existing jawbone.
Alternatives to Bone Grafting
There are some interesting alternatives, although they are often used alongside bone grafting to enhance results. These include:- Guided Tissue Regeneration: This technique uses a barrier membrane to separate the gum tissue from the bone defect. It prevents fast-growing gum tissue from invading the slower-healing bone area, giving the bone and periodontal ligament cells time to regenerate properly.
- Enamel Matrix Proteins (Emdogain): These proteins help stimulate the regeneration of the tissues that support the tooth, including bone, cementum, and the periodontal ligament.
- Growth Factors: These are natural substances your body uses for tissue healing and regeneration. Applying specific growth factors to the affected areas can further boost the healing process.
- Platelet Rich Plasma (PRP): PRP is a concentrated mix of platelets derived from your own blood. It can help speed up and improve healing and tissue regeneration.
Aftercare: Tips for a Smooth Recovery
Here are some tips to ensure a successful recovery:- Prevent bleeding: Right after the procedure, keep the dressing on the surgical site for a few minutes. If bleeding happens later, gently apply clean gauze with light pressure for about 15 minutes.
- Apply cold for the first 24 hours: Use an ice pack or cold compress on your cheek near the surgical area. This helps reduce swelling and discomfort. Apply for 10 to 15 minutes at a time, several times throughout the day.
- Avoid rinsing or spitting forcefully for the first 48 hours: During the first day, a blood clot forms at the site, which is the foundation for the next healing stages. Rinsing or spitting forcefully can damage it, causing bleeding and slowing down recovery.
- Be gentle around the wound for 2 weeks: Avoid putting pressure on the area by brushing or flossing too hard. The bone graft needs time to settle and stabilize, so be gentle for the first two weeks.
- Stick to soft foods: Eat soft, easy-to-chew foods for the first week that won’t irritate or damage the surgical site.
- Saltwater rinses: Starting from day two, gently rinse your mouth several times a day with warm water mixed with a teaspoon of salt. This helps keep the area clean and lowers the risk of infection.
- Maintain good oral hygiene: You can start gently brushing your teeth from the second day, but avoid flossing or touching the wound. After two weeks, you can begin cleaning the graft site gently with a soft toothbrush.
- Avoid smoking: Smoking slows healing and reduces bone regrowth and regeneration after grafting. It harms the clotting process, narrows blood vessels, and worsens gum disease. So it's important to rethink smoking for a better long-term outcome.
- Avoid strenuous activities: Take it easy for the first few days and avoid anything that raises blood pressure or strains the surgical site.
- Take prescribed medication: Follow your dentist’s instructions carefully regarding any medications.
- Periodontal infrabony defects: Systematic review of healing by defect morphology following regenerative surgery – Nibali – 2021 – Journal of Clinical Periodontology – Wiley Online Library
- Assessment of Autogenous Cortical Bone Grafting Combined with Guided Tissue Regeneration for Managing Intraosseous Periodontal Defects – PMC
- A Comparison of Freeze–Dried Bone Allograft and Demineralized Freeze–Dried Bone Allograft in Human Periodontal Osseous Defects – Rummelhart – 1989 – Journal of Periodontology – Wiley Online Library
- The Efficacy of Bone Replacement Grafts in the Treatment of Periodontal Osseous Defects. A Systematic Review – Reynolds – 2003 – Annals of Periodontology – Wiley Online Library
- Periodontal regeneration of infrabony defects (V). Effect of oral hygiene on long‐term stability – Cortellini – 1994 – Journal of Clinical Periodontology – Wiley Online Library
- Bone grafts in dentistry – PMC
- 17i-1230.indd – SciELO
- Effect of cigarette smoking on periodontal healing following GTR in infrabony defects. A preliminary retrospective study | https://pubmed.ncbi.nlm.nih.gov/7790529/