Gingivitis vs. Periodontitis: What’s the Real Difference?
 Gingivitis and periodontitis are both types of gum disease—but they’re definitely not the same.
Gingivitis and periodontitis are both types of gum disease—but they’re definitely not the same.
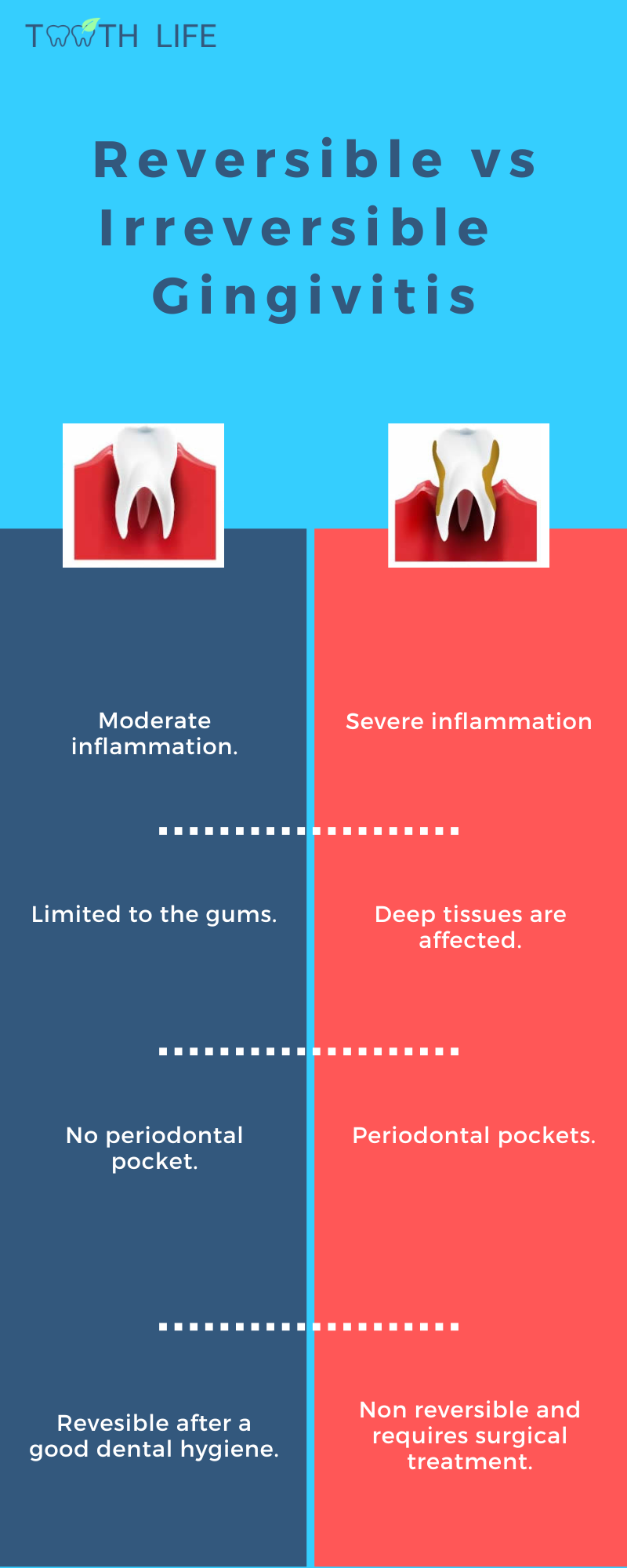
Gingivitis is the earliest and mildest form. It simply means inflammation of the gums.
Periodontitis, on the other hand, is much more serious. It affects the deeper structures that support your teeth—like the bone, ligaments, and cementum.
While gingivitis is common and completely reversible, periodontitis isn’t. It requires professional treatment and can never be cured at home.
In this article, we’ll break down the key differences between these two conditions, how gingivitis can progress into periodontitis, and what really causes them in the first place.
In this article:
1. The Difference Between Gingivitis and Periodontitis
2. Does Gingivitis Always Lead to Periodontitis?
3. What Causes Gingivitis to Turn Into Periodontitis?
4. What Happens If Periodontitis Is Left Untreated?
5. Takeaway
The Difference Between Gingivitis and Periodontitis
Gingivitis
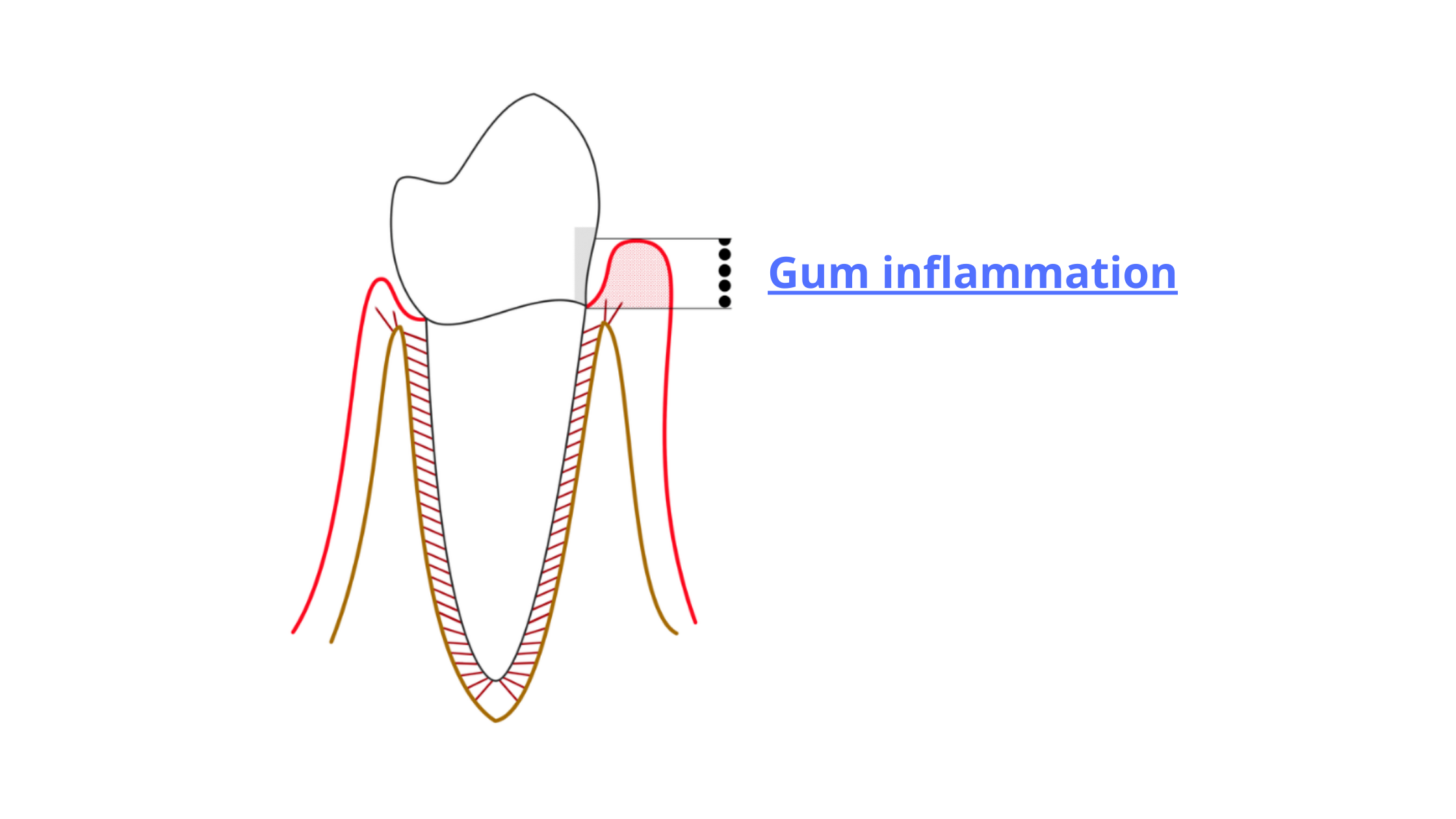
Gingivitis is when inflammation is limited to the gum tissue. It doesn’t affect the deeper structures like the bone or ligaments and is completely reversible.
It’s so common—some studies suggest that over 90% of adults experience chronic gingivitis at some point. Unlike periodontitis, it’s mild and not serious. You can think of it as the body’s natural response to plaque buildup on the teeth and gums.
When plaque accumulates, bacteria can slip under the gum line and trigger a mild, localized inflammation. This leads to red, swollen gums that may bleed when you brush or floss.
Periodontitis
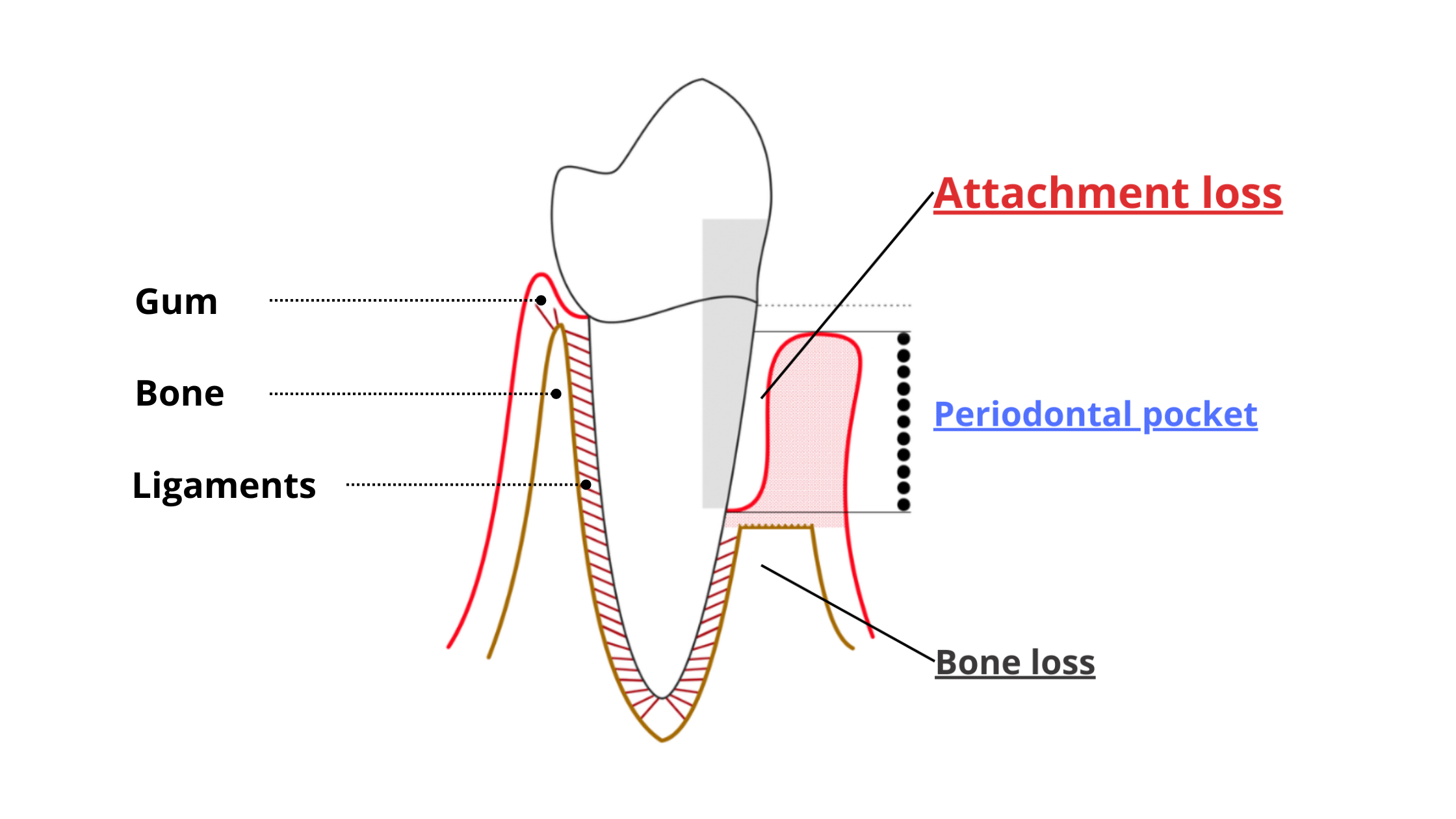
Periodontitis is a more advanced and damaging form of gum disease. In this case, the inflammation goes deeper and starts breaking down the tissues that hold your teeth, like the ligaments and supporting bone.
One of the key features of periodontitis is the formation of periodontal pockets—unnatural gaps that form between the roots of your teeth and gums.
The pockets appear when harmful bacteria and inflammation begin destroying the attachment between the teeth and surrounding structures.
These spaces are too narrow and deep for a toothbrush to reach. That’s what makes them the perfect hiding spot for bacteria to grow and cause even more damage.
More pockets → more bacteria → more damage.
You can’t treat periodontitis at home. It's not reversible like gingivitis and requires professional care—typically a procedure called scaling and root planing.
Does Gingivitis Always Lead to Periodontitis?
No, not everyone with gingivitis will develop periodontitis. Periodontitis is more complex than that.Gingivitis, however, is very common and can affect anyone. Most of the time, it's mild and not a big deal.
Gum inflammation is actually a normal, natural reaction to plaque buildup. Anyone—no matter how healthy—who skips brushing and flossing for a few days will likely notice red, swollen, or bleeding gums.
But, once the plaque is removed, the inflammation goes down, and the gums return to normal.
Periodontitis doesn’t work that way!
You can’t predict whether gingivitis will inevitably turn into periodontitis. For periodontitis to start and progress, it requires more than just plaque and bacteria.
It’s rather the result of many specific factors working together, such as:
- The balance between good and harmful bacteria in your mouth
- How your immune system reacts
- Lifestyle and environmental factors like stress and smoking
This explains why some people with poor oral hygiene never develop periodontitis, while others can have gingivitis for years without any bone loss or deep pockets.
So, even though gingivitis doesn’t always lead to periodontitis, it should never be ignored. Treating it early is the best way to avoid the risk—even if that risk seems small.

What Causes Gingivitis to Turn Into Periodontitis?
Under normal conditions, your mouth keeps a delicate balance between bacteria and your immune system. When that balance is maintained, your gums stay healthy.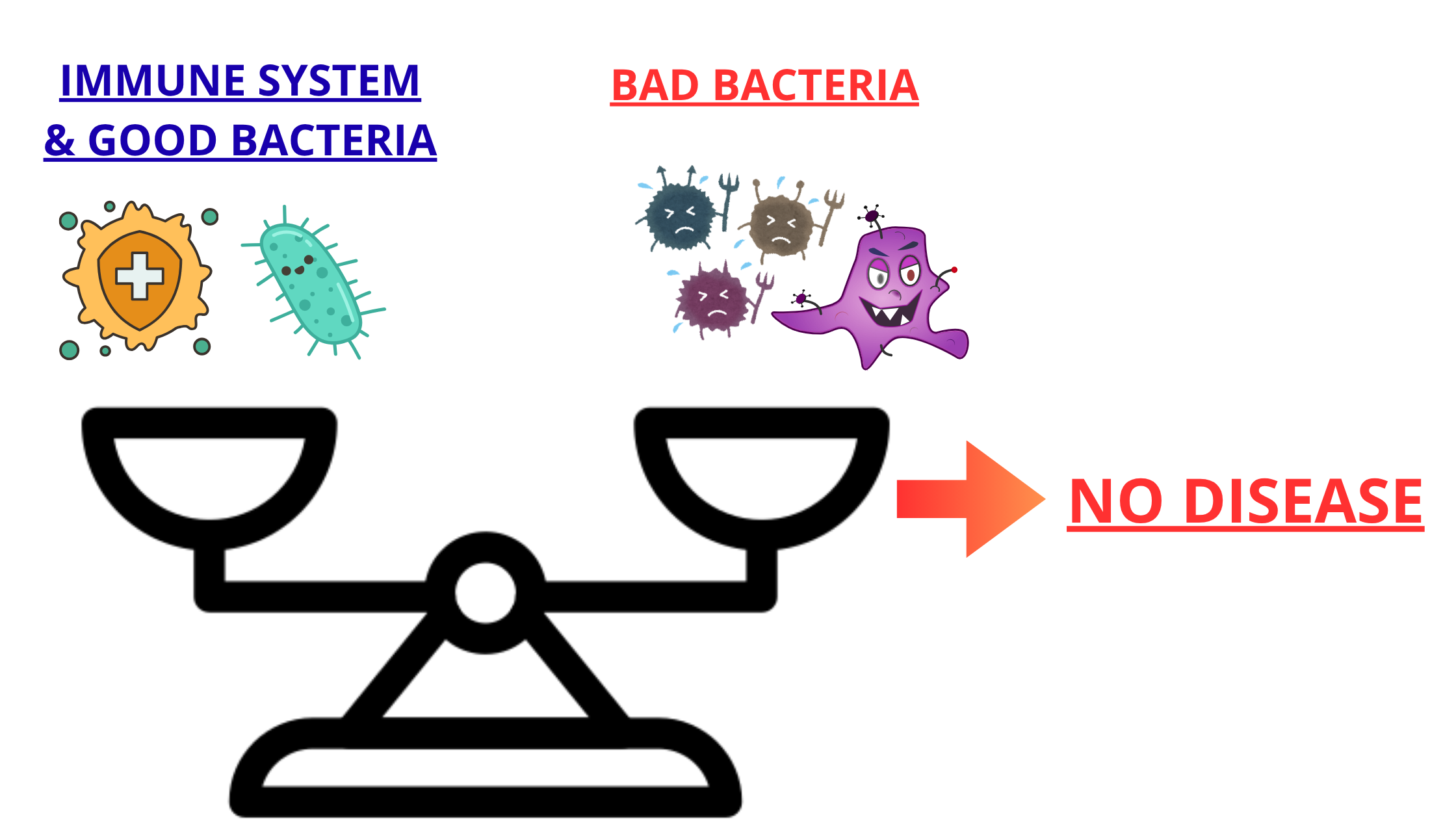
When plaque starts to build up, it irritates the gums and causes gingivitis.
The severity of gingivitis depends more on the amount of bacteria. The thicker the plaque, the more intense the inflammation.
At the gingivitis stage, your immune system is still strong enough to keep the bacteria in check and prevent them from spreading into deeper tissues.
But with periodontitis, it’s no longer about how much bacteria you have—it’s about the specific types of bacteria.
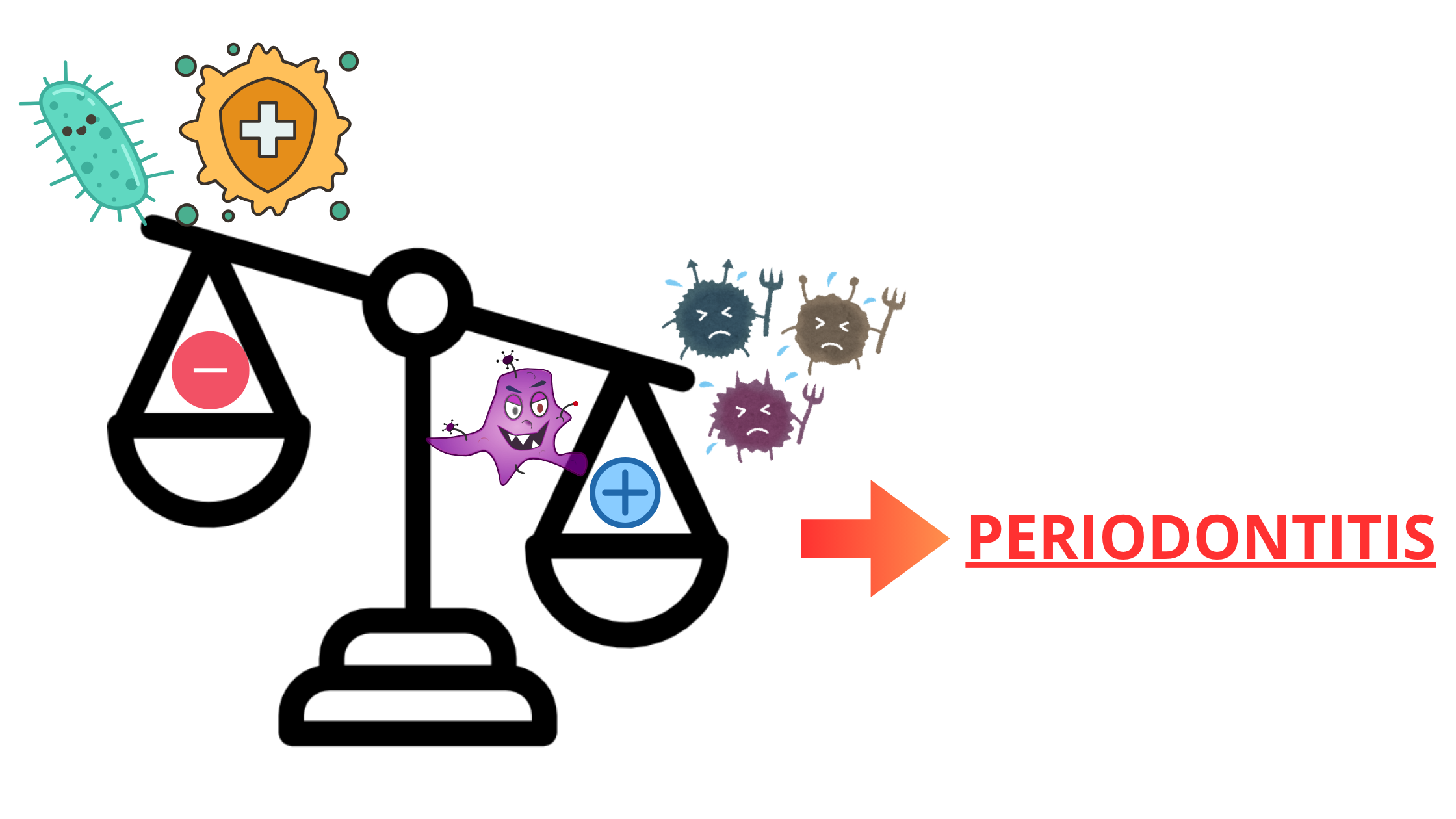
For gingivitis to progress into periodontitis, highly aggressive bacteria need to overcome both your immune system and the friendly bacteria in your mouth.
Still, these bad bacteria alone aren’t enough. How your immune system reacts, along with other local and general factors, plays a major role as well.
Here are some of the factors that can cause gingivitis to progress into periodontitis:
Poor Oral Hygiene
Bacteria are almost always the starting point for any form of gum disease.
If you don’t brush or floss daily, you’re giving bacteria the perfect opportunity to form plaque—a sticky film that helps bacteria become even more harmful.
Having plaque doesn’t automatically mean you’ll get periodontitis. But it's also true that periodontitis can’t develop without harmful bacteria thriving in your mouth.
Plaque forms constantly—even just a few hours after thorough brushing. That’s why regular brushing and flossing are essential to keep it under control.
Anatomical Factors
While these aren’t direct causes of periodontitis, they can increase your risk when combined with other factors:
- Tooth crowding or overlapping: Crowded teeth are harder to clean properly and tend to trap food and plaque more easily.
- Thin gums: People with a thin gum biotype are more likely to experience gum recession. Thin gums are also less resilient and more prone to damage from inflammation.
- Receding gums: When gums pull away from teeth, they expose the root surfaces. Exposed roots can make daily oral hygiene more challenging and increase the risk of further gum problems.
Mouth Breathing and Dry Mouth
People who breathe through their mouth instead of their nose are more likely to suffer from chronic dry mouth.
Dry mouth is a major risk factor not only for gum disease but also for cavities. Saliva plays a key role in cleaning your mouth and fighting off harmful bacteria.
When saliva flow is low, your gums can dry out, allowing bacteria to multiply and cause chronic inflammation.
Genetics
As we've said, gum disease results from an imbalance between your immune system and harmful bacteria. Your genes play a big role in how your immune system responds.
Some people’s immune systems react with severe inflammation that can actually damage tissues instead of healing them.
It’s not uncommon for patients with aggressive forms of periodontitis to have relatives who suffer from the same condition.
Smoking
Tobacco contains hundreds of harmful chemicals that:
- Reduce blood flow to your gums
- Weaken your immune response
- Damage the healthy cells that maintain the gum tissue
- Help harmful bacteria grow further
Compared to non-smokers, smokers:
- Are 6 times more likely to develop gum disease
- Tend to have deeper and more severe periodontal pockets
- Experience more gum recession
- Suffer greater bone loss
- Are more likely to lose teeth
Stress
Stress and anxiety are well-known risk factors for periodontitis. Many studies show that people who experience high levels of stress daily are more likely to develop this serious gum disease.
But how exactly does stress affect your gums? One key reason is the hormone cortisol. When cortisol levels are constantly high, it can weaken your immune system and promote chronic inflammation. Chronic long-lasting inflammation does more harm than good.
What's more, people who are stressed or depressed tend to have poorer eating habits, neglect their oral hygiene, and care less about their gums.
Aging
Aging naturally increases the risk of periodontitis for several reasons:
- Longer exposure to plaque and tartar buildup over time
- The cumulative damage caused by bacteria throughout the years
- A weakening immune system as we grow older
- Increased risks of chronic illnesses that weaken the immune system like diabetes
Unhealthy Diet
People with severe nutritional deficiencies are at a higher risk of developing aggressive forms of gum disease.
For example, a lack of vitamin C can lead to severe forms of gingivitis.
Research also suggests that vitamins E and D, as well as omega-3 fatty acids, may play a role in how gum disease progresses.
While no diet alone can prevent or cure gum disease, eating a healthy, balanced diet is always beneficial—not just for your mouth, but for your overall health as well.
What Happens If Periodontitis Is Left Untreated?
Once gum disease reaches the stage of periodontitis, the damage can no longer heal on its own. Even worse, the disease tends to become self-sustaining and may worsen over time.The deep periodontal pockets can’t be cleaned effectively with regular brushing or flossing. As these pockets widen, more bone is lost, creating even more space for harmful bacteria to thrive.
When bone loss becomes severe, your teeth can loosen and eventually fall out.
But periodontitis is more than just a local issue—it can have effects throughout your entire body.
The chronic inflammation caused by periodontitis can lead to a pro-inflammatory state, which may negatively impact other systems.
When the immune system is weak, bacteria from the gums can travel through the bloodstream to vital organs—sometimes leading to serious complications.
Many studies have found strong links between periodontitis and serious health conditions, including:
- Cardiovascular diseases like atherosclerosis and endocarditis
- Brain complications such as stroke and abscess
- Rheumatoid arthritis
- Lung infections
- Kidney disease
- Diabetes
Takeaway
Treating gum disease early, at the gingivitis stage, is much easier, less painful, and less costly as well.At this point, the condition is completely reversible, and you can stop it from progressing into periodontitis, which is more complex to treat and can be devastating for your gums and bone.
That’s why you should never ignore the early signs of gum inflammation. Redness, swelling, or bleeding are your body’s way of saying something’s wrong.
Take action now—heal your gums and protect your oral health before it’s too late.
Sources
- Impact of Smoking Cessation on Periodontal Tissues - ScienceDirect
- Exploring the Correlation Between Psychological Stress, Anxiety, and Periodontitis Among University Students: A Cross-Sectional Investigation - PMC
- Color Atlas of Dental Medicine: Periodontology by Edith M. Rateitschak and Herbert F. Wolf