How herpes viruses can affect your mouth (with helpful pictures)
 Oral infections caused by the herpes virus are commonly known as cold sores or fever blisters.
Oral infections caused by the herpes virus are commonly known as cold sores or fever blisters.
They’re more common than you might think — in fact, about 67% of people under age 50 carry herpes simplex virus type 1 (HSV-1), which is the main cause of viral infections in the mouth.
Most herpes infections go unnoticed because the virus stays dormant in the body. But when it reactivates, it can cause a range of symptoms, including painful sores and ulcers in and around the mouth.
There isn’t just one — but several types of herpes viruses that can appear in your mouth. In this article, we’ll break them down and share helpful pictures to make them easier to recognize.
In this article:
1. What is herpes virus?
2. How do herpes viruses affect the mouth?
3. What factors can reactivate the herpes virus again?
4. Other types of herpes viruses that can affect the mouth:
5. How is oral herpes infection treated?
6. How to prevent oral herpes infections?
What is herpes virus?
Herpes is a family of viruses that can cause infections in different parts of the body, including the mouth. Oral herpes infections are quite common and can affect people of all ages.There are various types of herpes viruses, each with its own features and symptoms.
The most well-known that affects the mouth is called herpes simplex virus type 1 (HSV1). However, other herpes viruses can also show up in the mouth, such as varicella-zoster virus (VZV), herpes simplex virus type 2 (HSV2), cytomegalovirus (CMV), and Epstein-Barr virus (EBV).
Regardless of the specific type, all herpes viruses go through two distinct phases.
The first phase is known as primary infection, which usually occurs during childhood when you first come into contact with the virus.
The second phase is called the recurrent or secondary phase. This typically happens in adulthood when the virus wakes up again, causing sores and ulcers in and around the mouth.
How do herpes viruses affect the mouth?
Herpes viruses affect the mouth by damaging the cells in the lining (the pink tissue called the mucosa), leading to multiple blister-like lesions. These blisters eventually break open, leaving behind painful ulcers or sores.HSV-1 is by far the type most commonly involved in oral infections. Most people catch it in childhood, usually between the ages of 3 and 5.
The first episode can cause symptoms like skin rashes, fatigue, fever, headaches, and nausea. In the mouth, it often causes diffuse redness and painful sores — a condition known as primary herpes gingivostomatitis.

After the primary infection, the virus becomes dormant and hides in the nerves. Later in adulthood, it can reactivate. The recurrent infection often appears as herpes labialis, which most often affects the lower lip. The sores can cause a burning sensation, itching, redness, and pain.
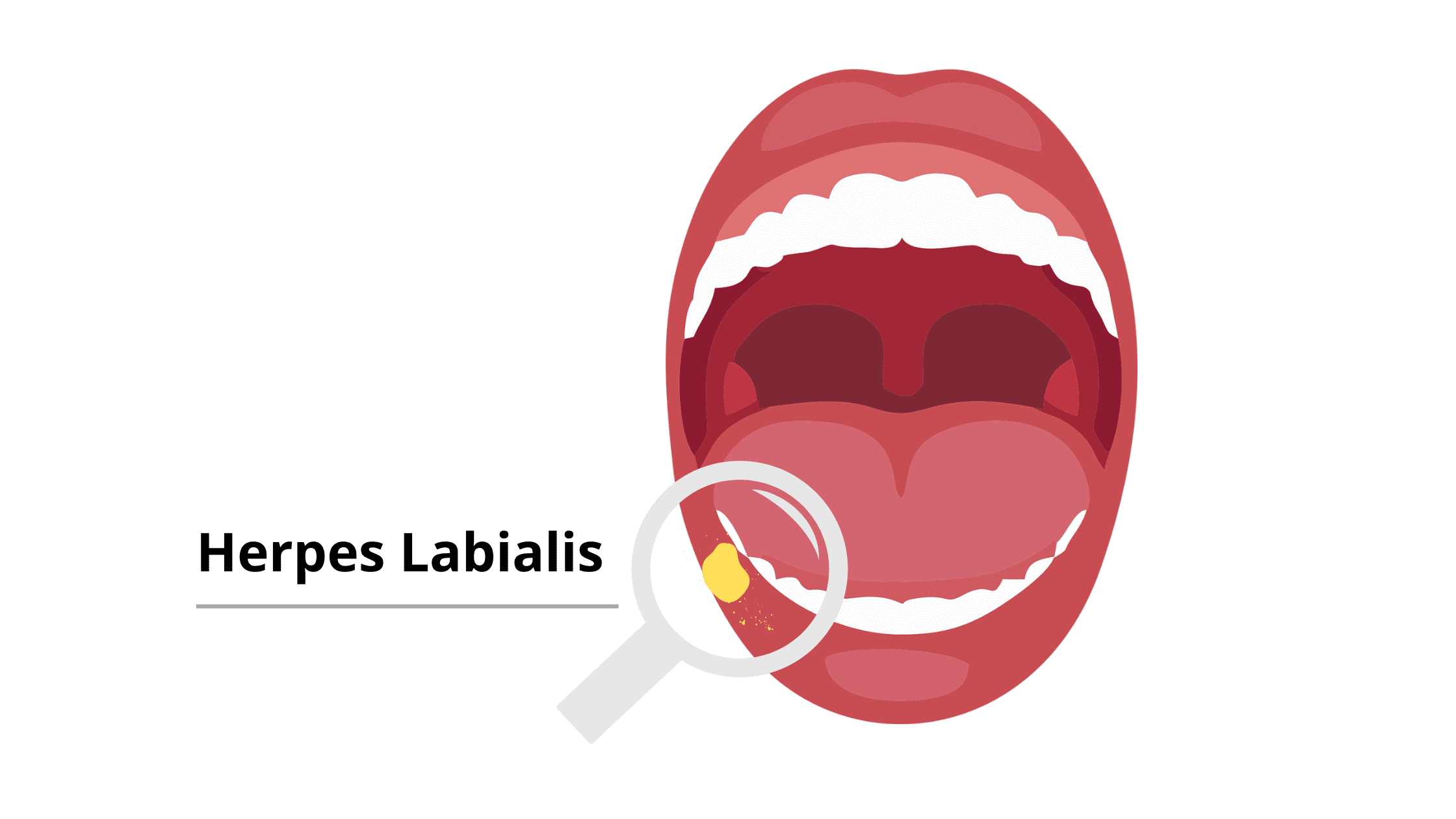
Oral herpes sores usually follow a clear pattern: small blisters appear first, then they break open and leave behind small, painful ulcers. These ulcers typically heal on their own within 7 to 14 days without leaving scars.
What factors can reactivate the herpes virus again?
After the primary infection, the virus hides in the nervous system, where it can stay dormant for decades. However, certain factors can trigger its reactivation and lead to a new outbreak in the mouth. These factors include:- Stress
- Mouth injury or trauma
- Fever or illness
- Common cold
- Malnutrition
- Hormonal imbalance
- Prolonged exposure to sunlight
- HIV infection
Other types of herpes viruses that can affect the mouth:
Aside from HSV-1, other viruses in the herpes family can also cause infections in the mouth. These include:- VZV (Varicella Zoster Virus): VZV is also common and can cause two conditions: chickenpox (the primary infection) and shingles (the secondary infection). Shingles occurs when the dormant VZV reactivates, which is more likely to occur after age 50. It can cause a painful rash in any area of the mouth, such as the gums, cheeks, roof of the mouth, and lips. The sores usually follow a specific nerve path and affect only one side of the mouth.
- HSV2 (Herpes Simplex Virus Type 2): HSV-2 primarily affects the genital area, but it can occasionally be transmitted to the mouth, causing oral herpes.
- EBV (Epstein-Barr Virus): EBV is associated with many conditions like infectious mononucleosis, commonly known as mono. It is highly contagious and mainly spreads through saliva. In addition to symptoms like swollen lymph nodes, fever, headache, and fatigue, mono can also cause bleeding, painful, and ulcerated gums.
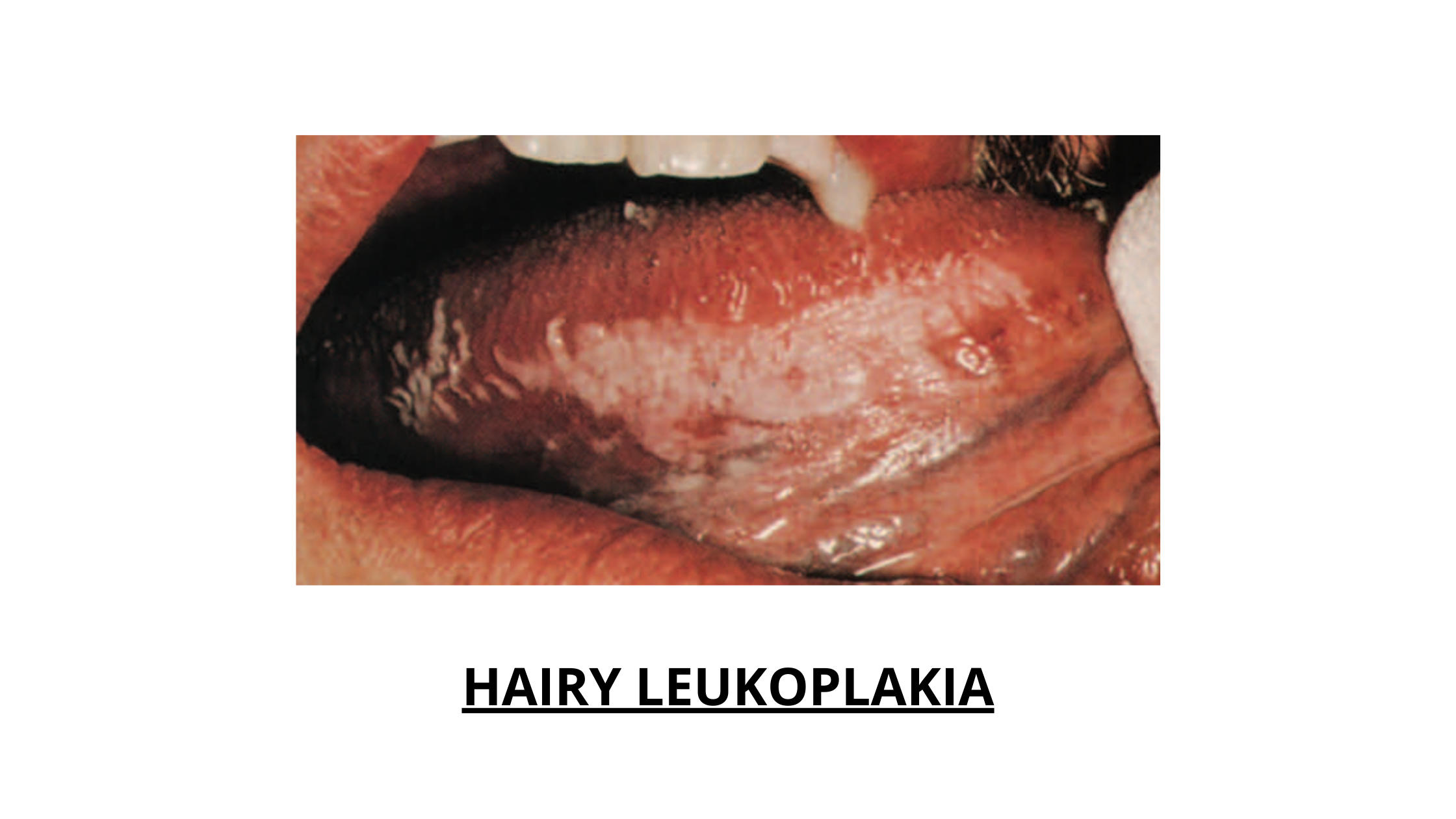
Another oral condition caused by EBV is Hairy Leukoplakia (white, raised patches on the sides of the tongue). It mainly affects people with weakened immune systems, especially those with HIV infection.
- CMV (Cytomegalovirus): CMV is another herpes virus that can manifest in the mouth as canker sores or painful ulcers.
How is oral herpes infection treated?
Oral herpes and most viral infections in the mouth usually heal on their own and don’t require special treatment. However, if an outbreak is severe and very painful, treatment may include the following approaches:- Antiviral medication: Antiviral medications can reduce the severity and duration of outbreaks by slowing down the virus. This helps the body to heal more quickly.
- Antiseptic mouthwash: These can help prevent secondary infections.
- Soft diet: To avoid irritating the affected area, it’s best to avoid hard, crunchy, hot, or spicy foods. Good options include soups, mashed potatoes, yogurt, and smoothies.
- Painkillers: Over-the-counter painkillers like acetaminophen or ibuprofen can be effective for providing temporary relief.
How can I prevent further oral herpes outbreaks?
Most adults carry the dormant form of the herpes virus, and there’s no way to completely kick it out from your body. However, this usually isn’t a problem because your immune system keeps the virus in check and prevents it from causing symptoms.The best way to prevent a herpes outbreak is to avoid triggers that can reactivate the virus and to steer clear of direct contact with someone who has active sores, as they are highly contagious.
Here are some helpful tips:
- Don’t share personal items like toothbrushes, cups, or lip balm, especially with someone who has an active outbreak.
- Likewise, if you have an active herpes infection, avoid close contact with others to prevent spreading the virus.
- Practice good oral hygiene by brushing your teeth regularly, flossing, and cleaning your tongue.
- Use protection during sexual contact.
- Avoid stress, which is a well-known trigger for oral herpes outbreaks.
- Maintain a healthy, balanced diet to fuel your immune system with the nutrients it needs to do its job properly.
Sources
- Detailed STD Facts - Genital Herpes (cdc.gov)
- Report a possible correlation between necrotizing ulcerative gingivitis and mononucleosis (medigraphic.com)
- Infectious Mononucleosis: aka "MONO" (CCSU)
- Herpetic Gingivostomatitis - StatPearls - NCBI Bookshelf (nih.gov)
- Shingles (Herpes Zoster) | CDC
- Herpes simplex virus (who.int)
- Essentials of Oral Pathology by Swapan Kumar Purkait (Author)
- Oral Medicine (A Colour Handbook) by Michael A.O. Lewis (Author), Richard C.K. Jordan (Author)