HIV Mouth Sores: A Complete Visual Guide with Pictures
HIV (human immunodeficiency virus) is a viral infection that slowly weakens the body’s immune system over time. As the disease progresses, the number of important immune cells—called CD4 T cells—gradually drops, while the amount of virus in the body (viral load) increases. This makes it harder for the body to fight off even minor infections or illnesses that it would normally handle easily.
Around 90% of people living with HIV will have at least one symptom in their mouth. One of the most common signs? Mouth ulcers or sores.
In this article, we’ll show you what HIV mouth sores look like, how to tell them apart from regular canker sores, and other mouth conditions that may be warning signs of HIV infection.
Around 90% of people living with HIV will have at least one symptom in their mouth. One of the most common signs? Mouth ulcers or sores.
In this article, we’ll show you what HIV mouth sores look like, how to tell them apart from regular canker sores, and other mouth conditions that may be warning signs of HIV infection.
In this article...
1. Can HIV Cause Mouth Sores?
2. When Do HIV Mouth Sores Appear?
3. What Do HIV Mouth Sores Look Like?
4. Other Common Mouth Conditions That Should Raise a Red Flag for HIV Infection
5. How Are HIV Mouth Sores Managed?
Can HIV Cause Mouth Sores?
Yes, mouth sores or ulcers are a common sign of HIV infection. In fact, studies show that about 50% of people living with HIV will develop some form of mouth sore or ulceration.But, HIV itself doesn’t directly cause the sores. Instead, the virus weakens the immune system, allowing other infections or conditions to flare up and cause these painful lesions.
The most common HIV-related conditions that lead to mouth ulcers are:
Viral Infections
Once HIV enters the body, it can "reactivate" viruses that were previously dormant and harmless. By far the most common of these is oral herpes, which affects 10% to 25% of people with HIV.
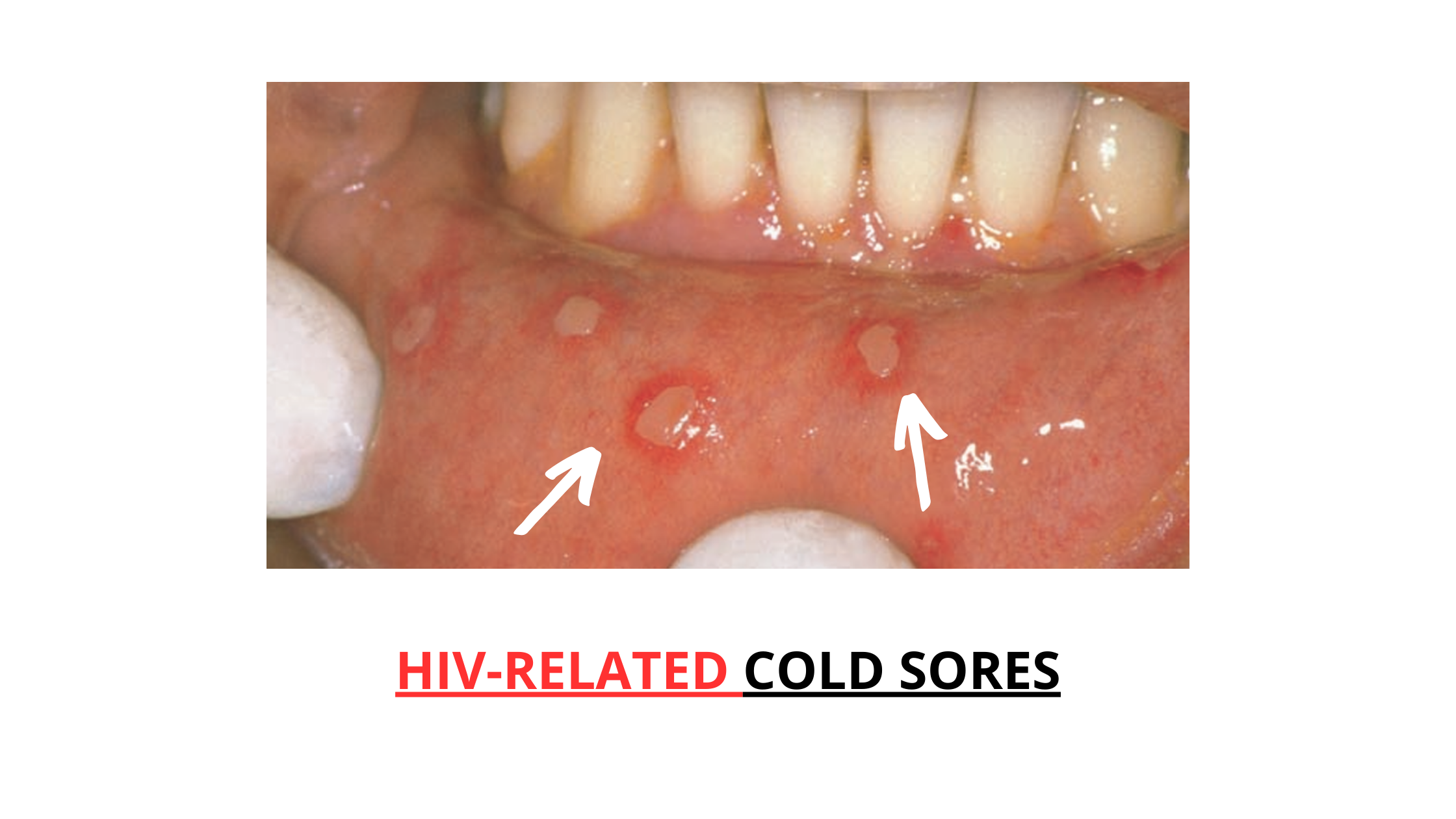
Herpes causes painful sores, often called cold sores or fever blisters. While many people get them occasionally, in those with HIV, the sores tend to be much more severe. They can be larger, more painful, longer-lasting, and even spread to the throat.
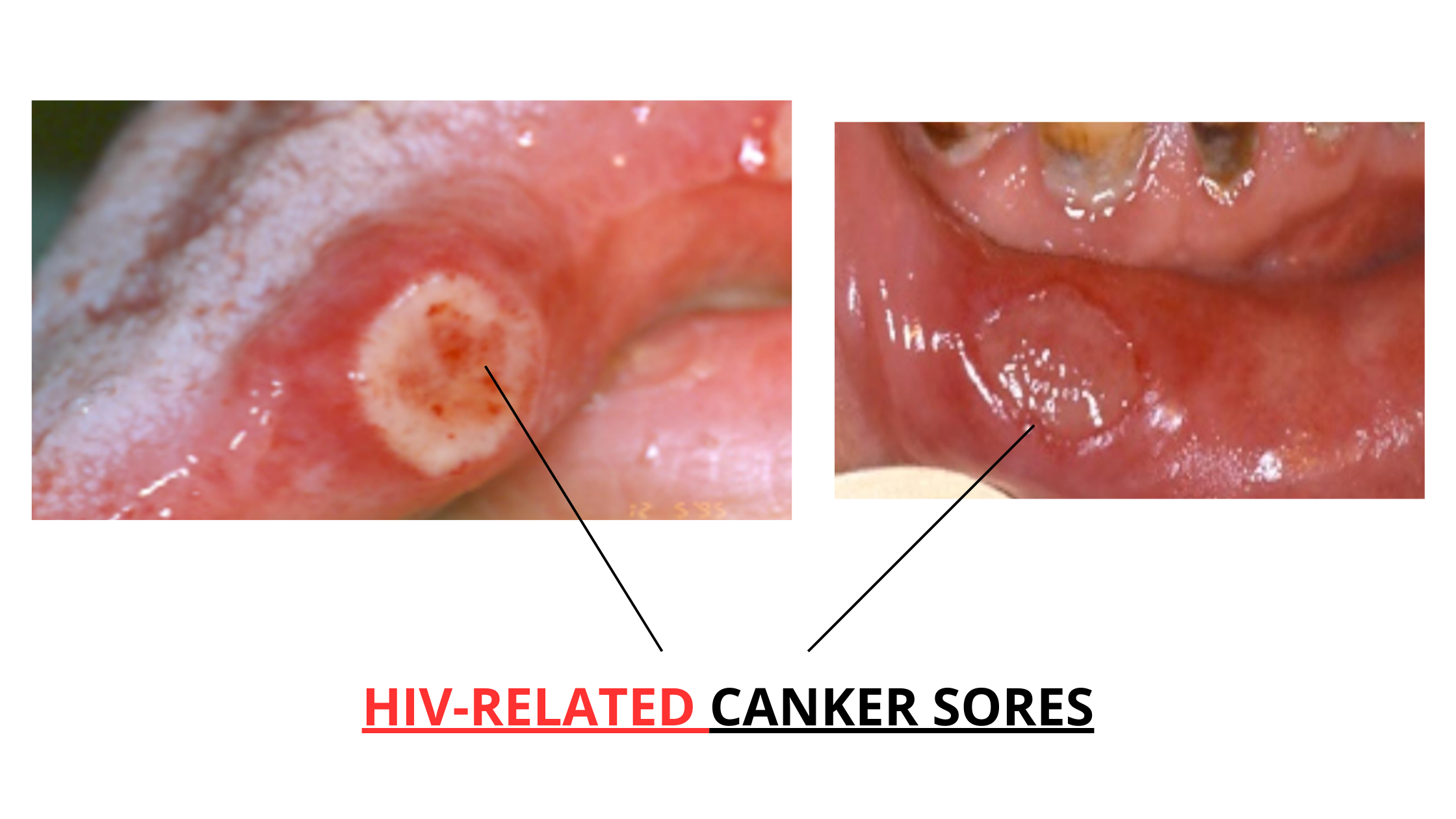
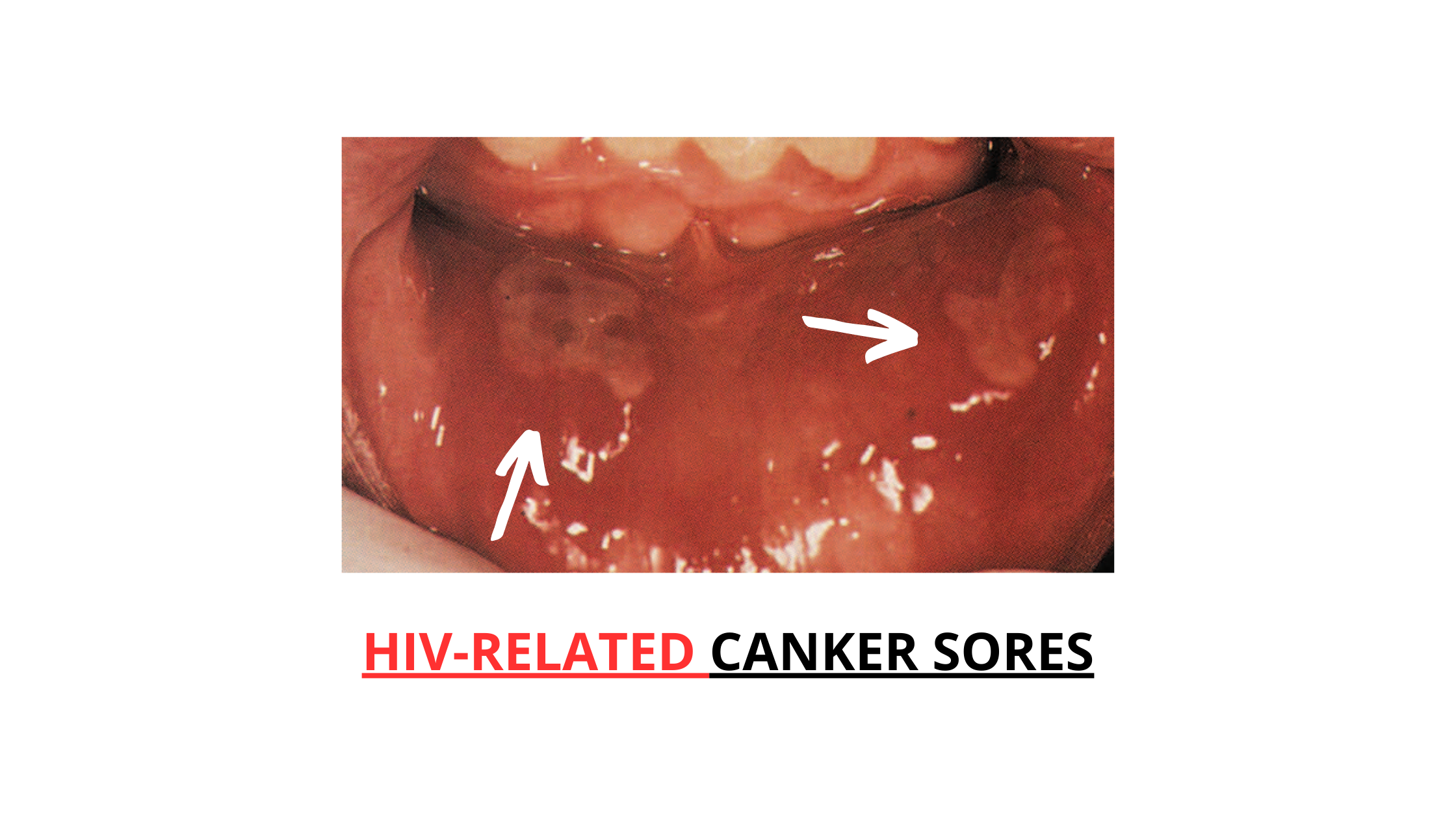
Canker Sores (Recurrent Aphthous Stomatitis)
Canker sores are also too common, even in healthy people. While their exact cause isn’t fully understood, they’re often linked to genetics, stress, trauma, allergies, nutritional deficiencies, or hormone changes.
In people with HIV, canker sores tend to occur more often and are usually more severe. They can be several centimeters wide (over 1 inch), deep, extremely painful, and slow to heal.
While HIV often brings mouth sores, not every sore means you have HIV. In fact, mouth sores are far more common in healthy individuals without any underlying condition. They usually refer to canker sores, which affect up to 25% of the general population.
These small, painful ulcers often come back from time to time, but they’re always harmless, not contagious, and heal on their own within a few days.
Likewise, cold sores—caused by the herpes virus—are common and can affect anyone during their lifetime. Many things can trigger a herpes outbreak, including stress, the common cold, fever, mouth injuries, and even sun exposure.
Cold sores usually show up on or around the lower lip, but they can also appear anywhere inside the mouth. Like canker sores, they are self-limiting and go away without treatment.
These small, painful ulcers often come back from time to time, but they’re always harmless, not contagious, and heal on their own within a few days.
Likewise, cold sores—caused by the herpes virus—are common and can affect anyone during their lifetime. Many things can trigger a herpes outbreak, including stress, the common cold, fever, mouth injuries, and even sun exposure.
Cold sores usually show up on or around the lower lip, but they can also appear anywhere inside the mouth. Like canker sores, they are self-limiting and go away without treatment.
When Do HIV Mouth Sores Appear?
Mouth sores can show up at any point during the course of HIV infection. However, the lower the immune cell count (CD4 cells) and the higher the viral load, the greater the risk and severity of these outbreaks.This means the periods when oral signs are most likely to appear are the early and late stages.
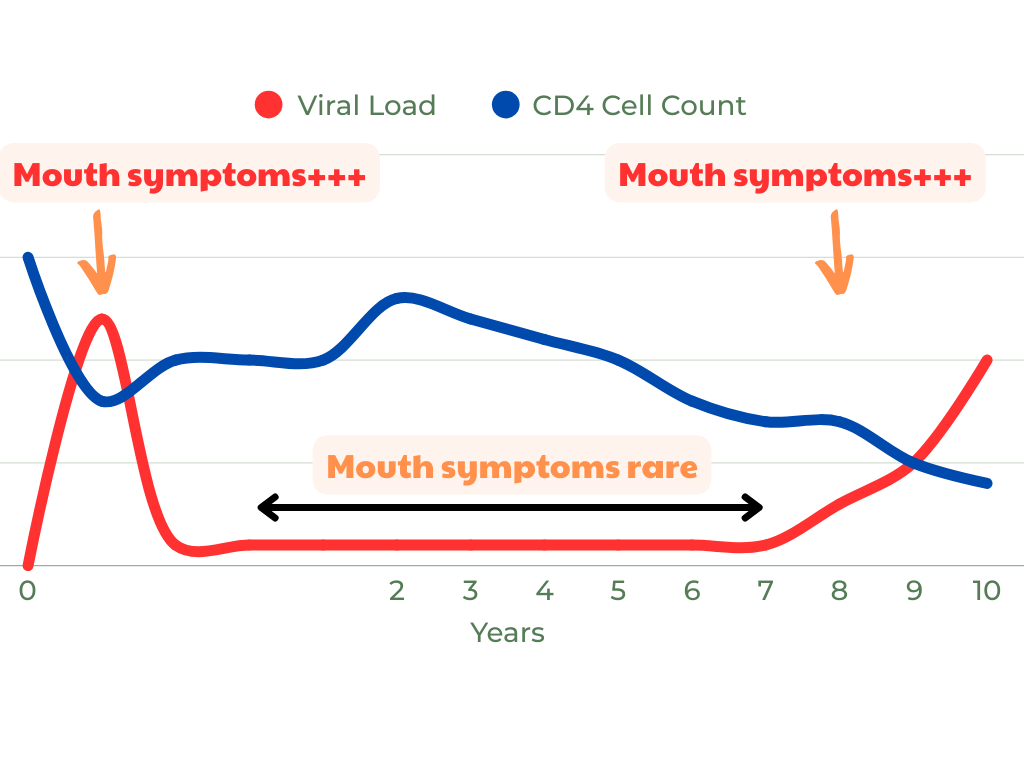
1. The Early Stage (Acute HIV Infection)
When HIV first enters the body, it triggers an acute stage that lasts for a few weeks. During this time, the viral load spikes, and the number of CD4 cells drops sharply.
It's common during this phase to develop mouth sores along with other flu-like symptoms such as fever, rash, sore throat, and headache.
2. The Late Stage (AIDS)
Years after the initial infection, HIV can progress to AIDS, the most serious and advanced stage. At this point, the immune system is collapsing, and the viral load is very high.
Mouth problems become very frequent, including canker sores, cold sores, fungal infections (like thrush), bacterial infections, and other inflammatory conditions.
What About the Middle Stage?
Between the early and late phases, there’s a long chronic stage, often called the asymptomatic stage. This can last for 10 years or more. During this period, the virus is still there but multiplies slowly, and people often don’t show symptoms.
As long as the immune cell count is high and the viral load stays low, mouth sores are usually rare or occasional.
What Do HIV Mouth Sores Look Like?
HIV-related mouth sores often look like common canker sores or cold sores, but the difference is in their severity, size, and how long they last.In healthy individuals, canker sores are usually small (about 0.5 cm or 0.2 inches), shallow, and occur in small numbers. They typically heal on their own within 7 to 10 days without leaving scars.
In people with HIV, however, canker sores can be much larger—up to 4 cm (about 1.6 inches). They may be deeper, extremely painful, and take weeks or even months to heal. They often leave a scar once healed.
The same goes for cold sores (fever blisters). While they’re common and harmless in most people, HIV can make them more severe. These sores can become widespread, very painful, and may take several weeks to go away.
In addition, HIV mouth sores rarely appear alone. Rather, they're often accompanied by other oral and general signs, such as:
- Advanced gum disease
- Widespread mouth inflammation (often due to fungal or bacterial infections)
- Persistent bad breath
- Fatigue
- Unexplained weight loss
- Swollen lymph nodes
- General feeling of being unwell
Other Common Mouth Conditions That Should Raise a Red Flag for HIV Infection
Mouth sores aren’t the only oral signs linked to HIV. Several other mouth conditions are just as common, if not more so, in people with HIV infection. These include:Oral Thrush (Candidiasis)
This is a fungal infection caused by Candida albicans, a yeast that naturally lives in the mouths of most healthy people. When the immune system is strong, it keeps Candida under control. But when the immune system is weakened, the yeast can overgrow and become harmful.
Oral thrush occurs in up to 75% of people with HIV.
What to look for:
- Thick, white or yellowish creamy patches on the tongue, cheeks, or roof of the mouth
- When wiped, the patches reveal a red, sore, and sometimes bleeding surface underneath
- Burning sensation in the mouth
- Difficulty eating or swallowing
- Red patches on the inside of the mouth
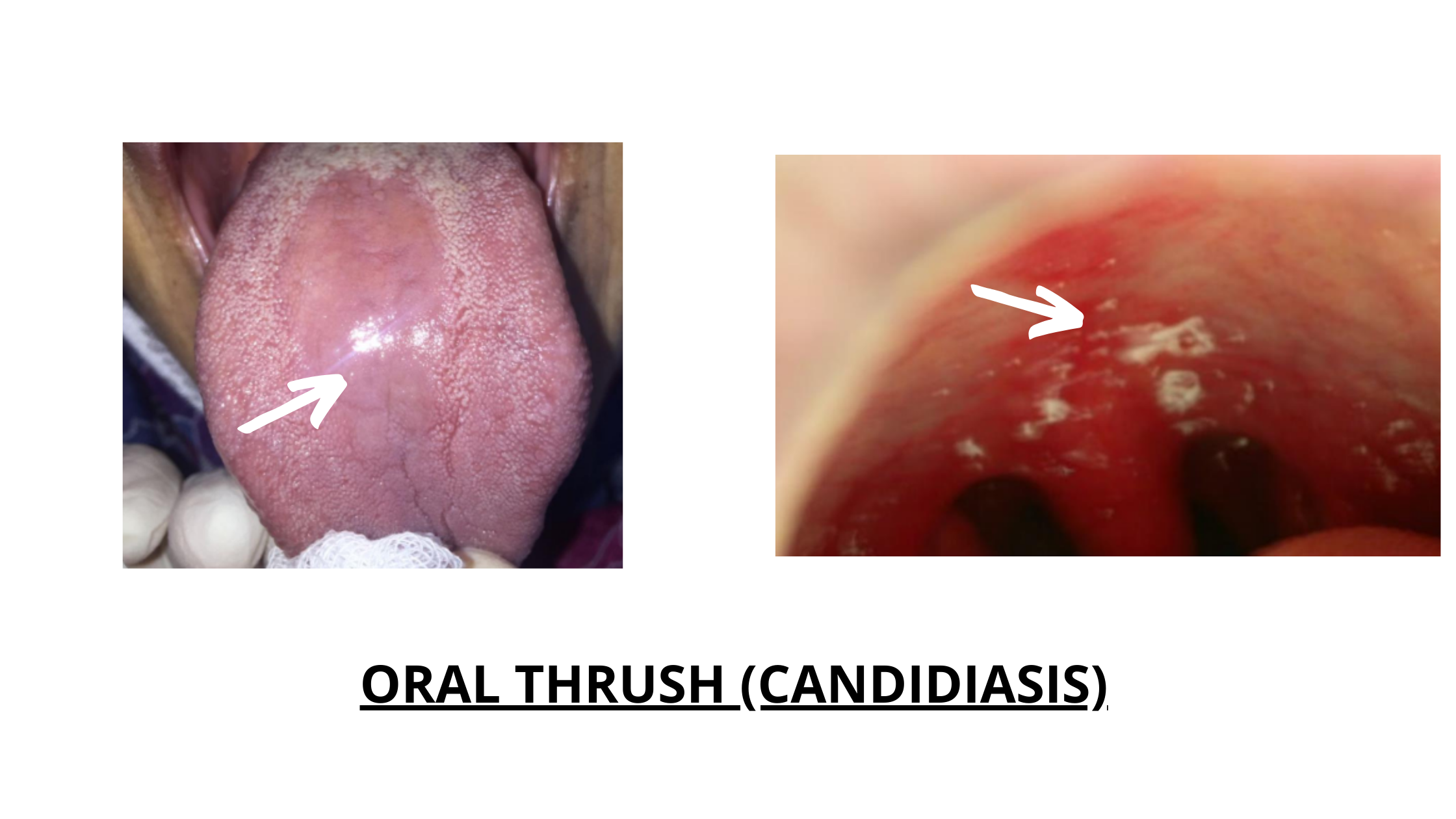
If there's no clear reason for the yeast overgrowth (like recent use of antibiotics or steroid drugs), HIV should be on the list of suspects.
Hairy Leukoplakia
Hairy leukoplakia is caused by the Epstein-Barr virus, another virus that stays dormant in the body until the immune system weakens. Many consider it to be one of the telltale signs of HIV.
Where and how it appears:
- Usually on the sides and underside of the tongue
- Looks like white patches with vertical, hair-like projections, hence its name
- The surface may appear slightly raised and may measure from a few millimetres to several centimetres
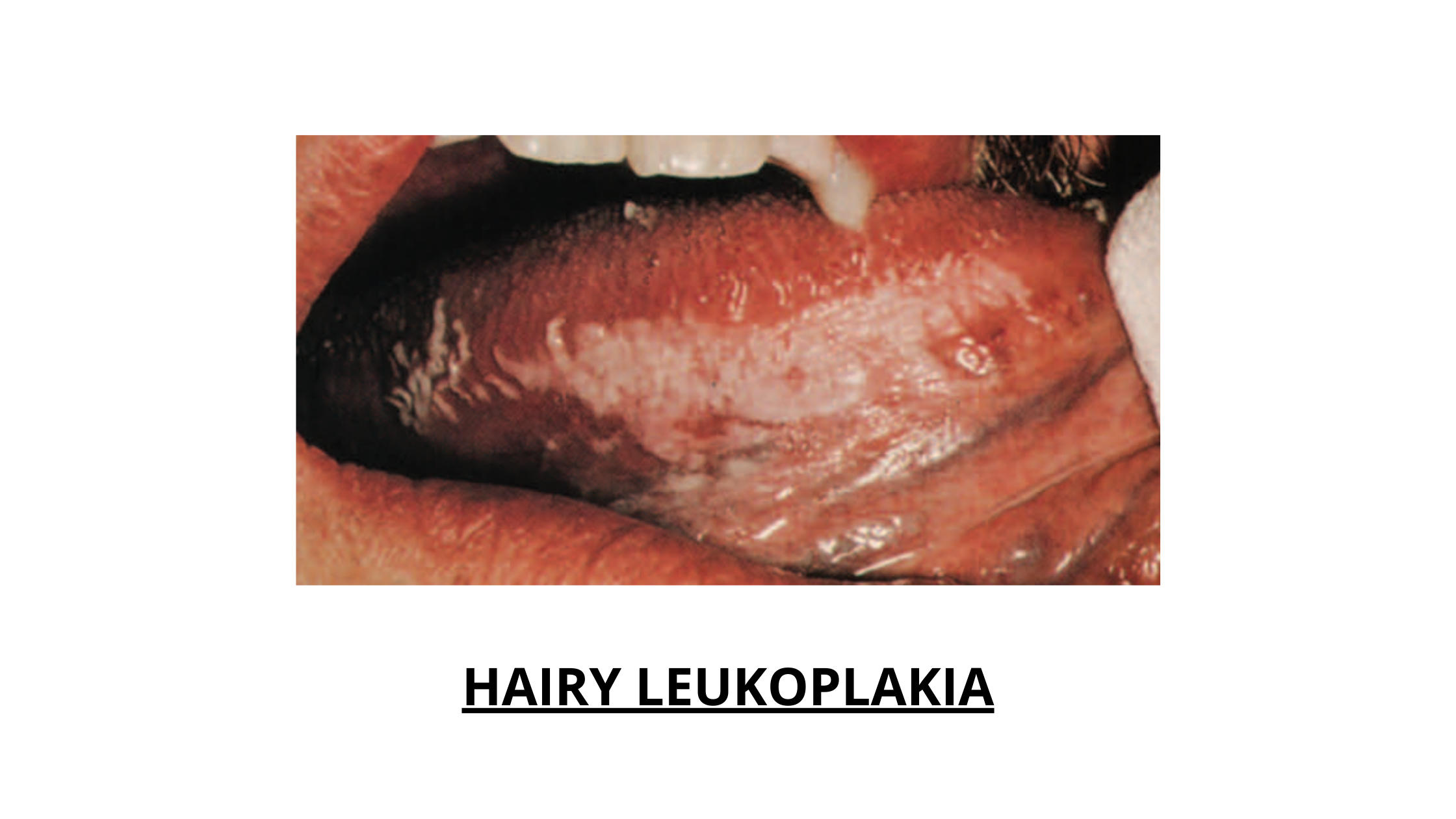
Hairy leukoplakia is harmless, non-cancerous, and doesn't cause pain or discomfort. It typically doesn't need treatment.
Ulcerative Gum Disease
Rapidly progressing, painful gum disease can often be one of the earliest signs of HIV infection. These conditions are known as necrotizing ulcerative gingivitis (NUG) and necrotizing ulcerative periodontitis (NUP).
When the immune system weakens, harmful bacteria in the mouth thrive and lead to gum inflammation and tissue destruction.

It often starts with a red line or band along the gums (image above right), known as linear gingival erythema (once called HIV-gingivitis)
As the condition worsens, painful ulcers and white areas of tissue death (necrosis) form, especially between the teeth. This is the necrotizing ulcerative gingivitis stage.
If left untreated, the infection can spread deeper, destroying the bone that supports the teeth. This advanced stage is called necrotizing ulcerative periodontitis (image above left), and it can lead to:
- Loose or shifting teeth
- Tooth loss
Other symptoms may include:
- Severe pain
- Bad breath or foul taste
- Fever
- Swollen lymph nodes
These gum conditions are extremely aggressive and painful, and require immediate treatment to avoid permanent damage to the gums and jawbone.
How Are HIV Mouth Sores Managed?
There’s no single treatment for HIV-related mouth sores. Instead, the approach depends on the underlying cause of the sore.The main goals of treatment are to:
- Relieve pain
- Promote healing
- Prevent infection or stop it from getting worse
- For fungal infections like oral thrush (Candidiasis): Treatment usually involves using antimicrobial mouthwash and antifungal medications, both topically (as a cream or ointment) and systemically (in pill or capsule form).
- For viral infections like cold sores: Topical antiviral creams can help reduce symptoms, speed up healing, and shorten the duration of outbreaks.
- For canker sores or aphthous ulcers: Treatment may involve topical corticosteroids to reduce inflammation and a numbing gel or cream to ease the pain.
The biggest challenge with HIV-related mouth sores is that they last longer than usual and tend to come back frequently, even after treatment.
That’s why regular dental checkups are key to catching and treating problems early, before they become more serious and harder to control.
Sources
- Color Atlas of Dental Medicine: Periodontology, Book by Edith M. Rateitschak and Herbert F. Wolf
- Essentials of Oral Pathology, Book by Swapan Kumar Purkait
- Recurrent Aphthous Stomatitis - StatPearls - NCBI Bookshelf https://www.ncbi.nlm.nih.gov/books/NBK431059/
- Oral manifestations of HIV infection https://pubmed.ncbi.nlm.nih.gov/8779462/