5 Potential Causes of Multiple Canker Sores at Once
 Canker sores are a common annoyance that can affect people in different ways.
Canker sores are a common annoyance that can affect people in different ways.
Most of the time, they appear as a single sore that heals on its own within a week. However, they can sometimes cause multiple sores to pop up at once, which may take longer to heal.
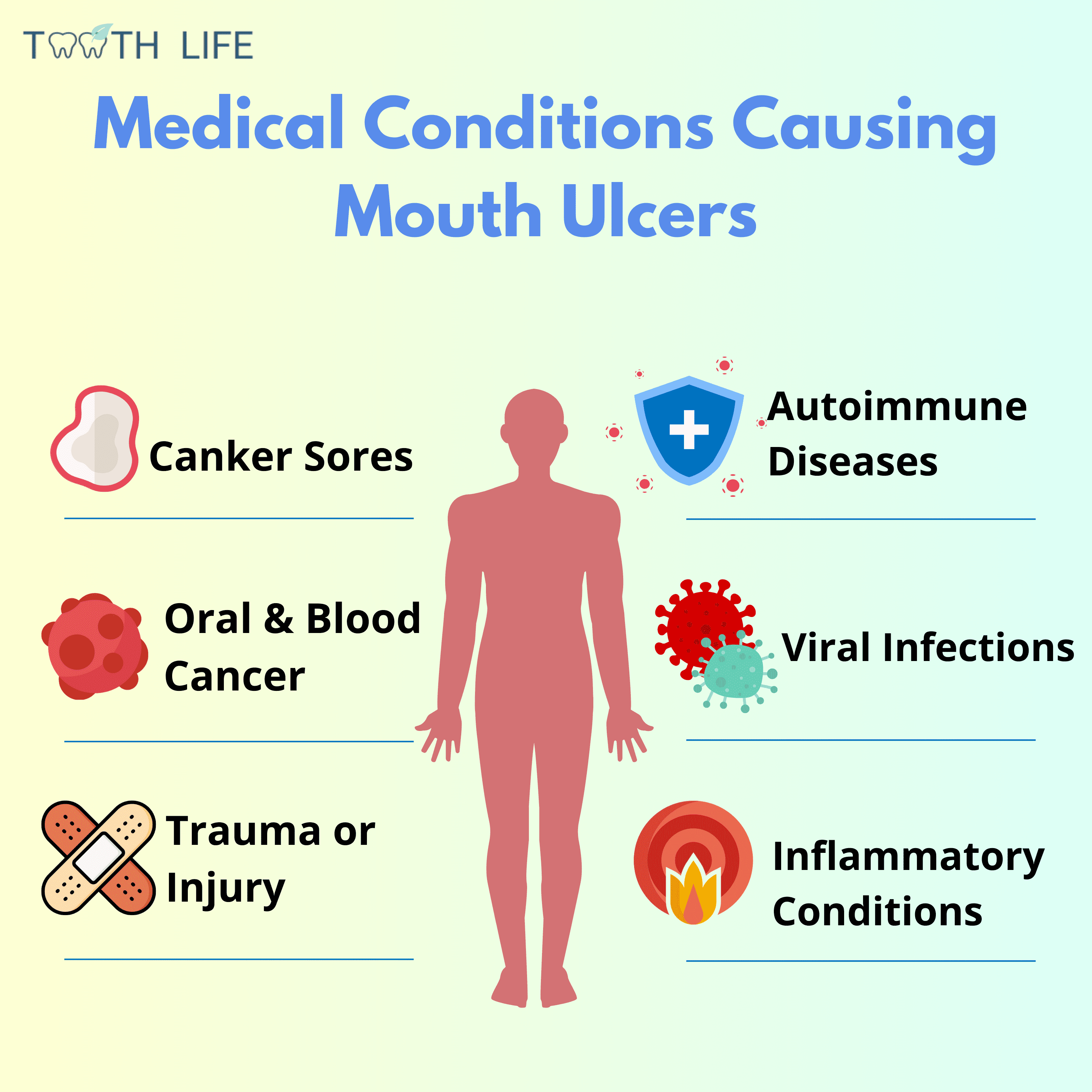
It’s also important to remember that not every ulcer in your mouth is necessarily a canker sore. While they’re the most common cause, many other oral conditions can look similar.
In this article, we’ll explore five possible reasons you might get multiple canker sores at the same time — and what you can do to manage them.
1. Aphthous Ulcers: The Most Likely Reason
2. Ulcerations Due to Injury or Trauma
3. Oral Herpes Infection: When the Virus Wakes up Again
4. Underlying Inflammatory Diseases
5. Autoimmune Diseases
Can multiple mouth sores point to something more serious?
Overcoming Multiple Canker Sores
Here are 5 reasons why you might be getting multiple ulcers. Understanding them will help you manage and prevent them more effectively.
1. Aphthous Ulcers: The Most Likely Reason
In most cases, mouth sores refer to a condition called Aphthous Stomatitis, or as you probably know them, canker sores.It's an inflammatory oral condition that causes small, round or oval sores to appear, with a yellowish-white center surrounded by a red border. These sores can pop up anywhere in your mouth, including the tongue, gums, the inside of the cheeks and lips.
They are known to be extremely painful, especially during meals or when brushing teeth.
Can Aphthous Stomatitis Show Up as Multiple Ulcers?
Canker sores can come in different sizes, numbers, and shapes. There are three types – minor, major, and herpetiform.
The minor ones are the most common, usually showing up as one to five small sores at a time. They're the mildest and usually heal within a week or so without leaving any scars.
The herpetiform form of canker sores can cause tiny countless sores to appear at once, sometimes even up to a hundred. It's called “herpetiform” because it looks like “oral herpes,” a common viral infection of the mouth that can also produce multiple sores (we will discuss this later).
In some cases, these ulcers may merge into a large one, which can take weeks or even months to fully heal.
Major canker sores are the most severe type, but fortunately the rarest (less than 10% of cases). They usually show up as a single, larger, deeper, and very painful ulcer. These sores can grow up to several centimeters in size and often take much longer to heal.
Who Is Most at Risk?
The exact cause is not yet fully understood, but possible triggers include genetics, stress, an abnormal response to mouth injuries, nutritional deficiencies, and allergies.
If it's your first experience with canker sores, some people have to deal with them several times a year. We call this Recurrent Aphthous Stomatitis, affecting roughly a quarter of the world's population.
Treatment
Unfortunately, there's no magic cure for canker sores. The good news is they always heal on their own. However, there are some things you can do to ease the pain and speed up the healing process. Here are some tips:
- Rinse with salt and baking soda: Mix a tablespoon of salt and baking soda in half a glass of water. Gargle with this solution several times a day. Both ingredients are soothing and have anti-inflammatory properties that can help calm canker sores.
- Apply a numbing product: Use an over-the-counter numbing gel like Orajel or Canker-X Mouth Sore Gel. These contain numbing ingredients that can reduce your discomfort.
- Use an antiseptic mouthwash: Choose an alcohol-free, peroxide-based rinse like Orajel Mouth Sore Rinse or Colgate Peroxyl Mouth Rinse. These help prevent infections and can promote healing.
2. Ulcerations Due to Injury or Trauma
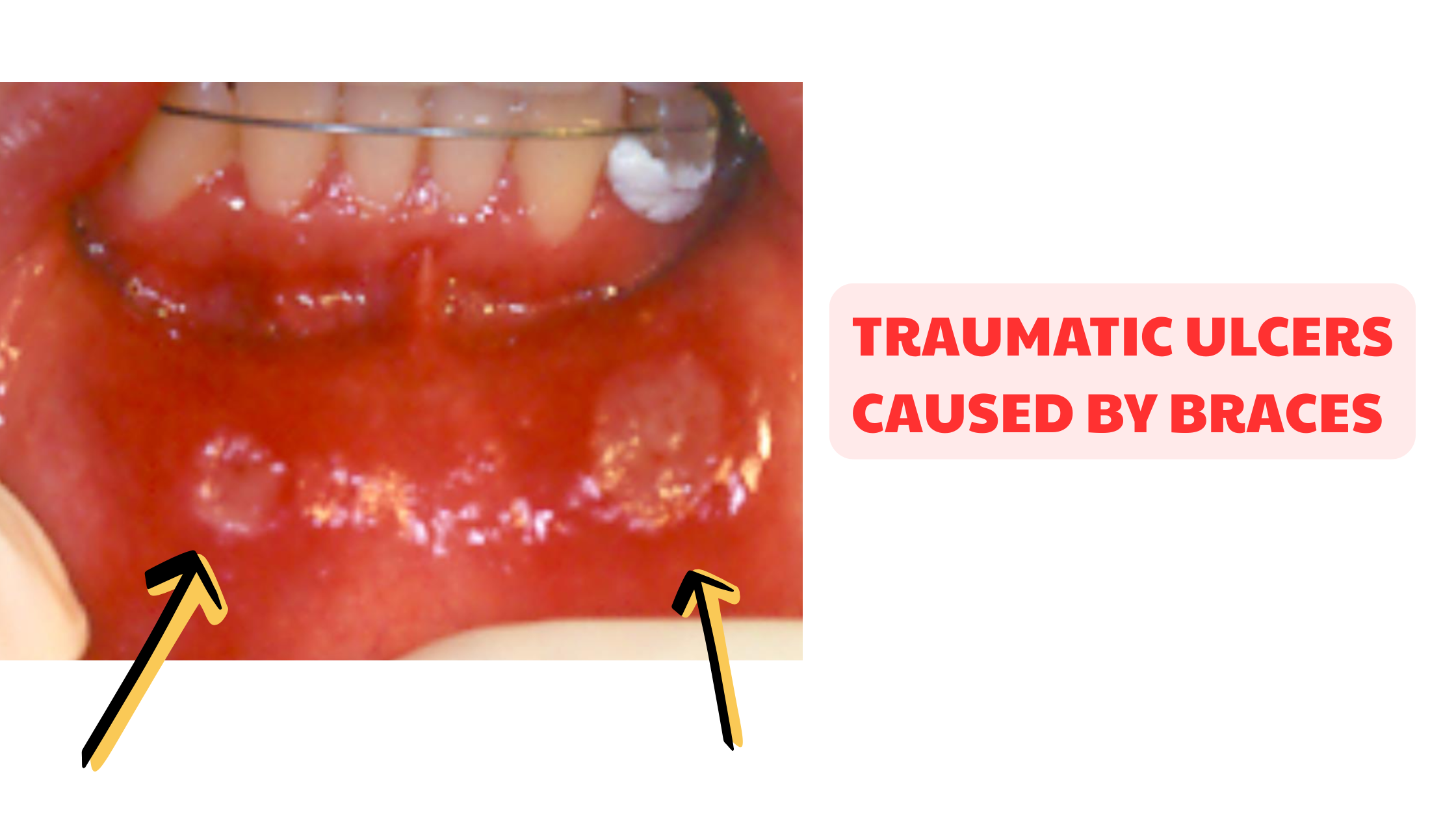
Ulcers that appear after you injure your mouth or burn it with something too hot can look like canker sores, but they’re actually different. These are called traumatic ulcers.
They can be caused by different things, including:
- A sharp tooth edge or rough dental filling rubbing against your cheek or tongue
- Wearing braces
- Injuries from a toothbrush or toothpick
- A mouth burn from very hot, spicy, or acidic foods and drinks
- Overusing a harsh, alcohol-based mouthwash
Unlike canker sores, traumatic ulcers usually don’t have a well-defined, round shape. They often look larger with uneven edges or borders.
Treatment for Traumatic Ulcers
Like canker sores, traumatic ulcers usually heal on their own once the source of injury is removed. First, identify what’s causing the problem and address it.
If the pain is too severe or the sores make it hard to eat, the same treatments mentioned above for canker sores will work.
3. Oral Herpes Infection (Cold sores or fever blisters)
Oral herpes is caused by a virus called herpes simplex virus type 1 (HSV-1). Most adults—about 67% of people under 50—carry the virus in its dormant form, which usually remains harmless and causes no symptoms.
The first exposure to the virus typically occurs in childhood, between the ages of 3 and 5. It's called the primary HSV infection.
During the primary infection, tiny, fluid-filled blisters can appear all over the mouth, often along with fever, fatigue, difficulty eating, and swollen lymph nodes. Other times, there are no noticeable symptoms.
After this initial episode, the virus retreats and hides in the body, staying dormant—sometimes for a lifetime.
Occasionally, the virus can reactivate and cause mild symptoms in the mouth, commonly known as fever blisters or cold sores. These usually appear on the lower lip but can affect any area of the mouth, including the gums (as shown below).

What triggers cold sores? Stress, mouth injuries, sun exposure, or a weakened immune system can all wake the virus.
An oral herpes outbreak typically begins with a tingling, burning, or numbing sensation, followed by clusters of yellowish blisters. These blisters eventually break open, forming multiple painful ulcers.
Oral Herpes Treatment
Cold sores typically heal on their own within 7 to 10 days. Your dentist or doctor might prescribe antiviral medications to help speed up recovery.
Home remedies and antiseptic mouthwashes can relieve and prevent these sores from getting worse.
4. Underlying Inflammatory Diseases
Mouth ulcers are essentially intense inflammatory reactions that occur in a specific spot, causing the breakdown of the mouth’s lining (mucosa). The red halo commonly seen around canker sores is a hallmark of this inflammation.
Some inflammatory conditions affecting the body can also affect the mouth, leading to sores. Two common examples are Behçet’s disease and Crohn’s disease.
Behcet's Disease
Behcet's disease is a rare disorder that causes chronic inflammation of blood vessels.
In your mouth, it can manifest as multiple, superficial, and painful ulcers that resemble canker sores.
This disease can also affect other body parts, such as the eyes, skin, kidneys, and brain. While the exact cause remains a bit of a mystery, it's thought to result from abnormal immune activity where the body mistakenly attacks its own cells.
Crohn's Disease
Symptoms might include redness and swelling, especially in your tongue and lips, along with canker sores. In fact, up to 20-30% of patients with Crohn's disease have reported experiencing aphthous ulcers (8).
5. Autoimmune Diseases
Less commonly, outbreaks of mouth ulcers can be linked to autoimmune diseases such as lupus, lichen planus, pemphigus and mucous membrane pemphigoid.Lupus
People with lupus often get several sores at the same time, which can be painful, especially when eating spicy or acidic foods.
Other common mouth symptoms related to lupus include red and white patches, flaky lesions, and dryness.
Lichen Planus
In fact, most people with lichen planus experience symptoms in the mouth, which can include:
- Lacy white patches
- Diffuse red areas
- Painful open sores
Oral symptoms tend to come and go, with flare-ups followed by periods of remission.
Pemphigus Disease
In pemphigus disease, the immune system overreacts and targets the components of the mouth's lining, specifically the proteins that hold the cells together. This self-destruction process causes fluid to leak through the mucosa, forming fluid-filled, bubble-like lesions. Since these bubbles are fragile, they burst quickly, leaving behind erosive surfaces and extremely painful ulcers.
Pemphigoid Disease
Pemphigoid follows a similar process, but it affects deeper layers of the oral mucosa, causing blister-like lesions that are tougher and less likely to rupture easily.
Once diagnosed, they should be managed promptly, as some can be life-threatening.
Treatment typically involves oral corticosteroids, which help by suppressing the immune system activity to prevent further damage to the body’s tissues.
Can multiple mouth sores point to something more serious?
Mouth ulcers are common and usually harmless. Anyone can get them, even the healthiest individuals.
Can mouth ulcers signal a serious medical condition? The answer is yes—but this is very unlikely.
Benign ulcers are typically temporary and heal on their own within up to two weeks without scarring. If they last too long, don't ignore them.
It’s best to rule out more serious conditions, which can include:
- Oral cancer: A persistent ulcer that lasts unusually long can be an early sign. Not only sores, but any persistent lesion or change in your mouth—red or white patches, lumps, or unexplained bleeding—should be checked by your dentist.
- Blood cancer: The type most commonly associated with multiple and severe mouth ulcers is leukemia. Swollen gums and unexplained bleeding in the mouth are common signs as well.
- HIV infection: People with HIV may experience multiple, severe canker sore outbreaks, especially in the early and late stages of infection. These sores are often major—large, deep, and very painful.
Overcoming Multiple Canker Sores
Now that we’ve covered the possible causes of multiple canker sores at once, it’s up to you to identify your own risk factors that might be triggering the sores and making them worse.
By spotting and addressing these factors, you can reduce the frequency and severity of outbreaks.
Some helpful measures include:
- Managing stress effectively
- Avoiding foods you may be sensitive or allergic to
- Addressing nutritional deficiencies, especially B12, iron, and zinc
- Protecting your mouth to prevent injuries
If you find yourself getting canker sores several times a year, you’re not alone — about 25% of people experience this. With the right habits, you can prevent outbreaks or at least reduce their severity.
As we’ve seen, although canker sores are the most common cause of mouth ulcers, they aren’t the only ones. Mouth sores can also signal underlying health conditions that may require medical attention.
If your sores don’t heal within one or two weeks or continue to worsen, it’s worth having them checked by your dentist or doctor.
- Essential Of Oral Pathology - Book by Swapan Kumar Purkait
- Canker Sore - an overview | ScienceDirect Topics
- Prevalence and risk factors of recurrent aphthous stomatitis among college students at Mangalore, India
- Herpes simplex virus (who.int)
- Behcet's Disease | National Institute of Neurological Disorders and Stroke (nih.gov)
- Crohn's disease - Symptoms and causes - Mayo Clinic
- Oral Pemphigus Vulgaris - PMC (nih.gov)
- Oral manifestations of inflammatory bowel disease | DermNet (dermnetnz.org)