Oral Thrush: A Common Fungal Infection of the Mouth
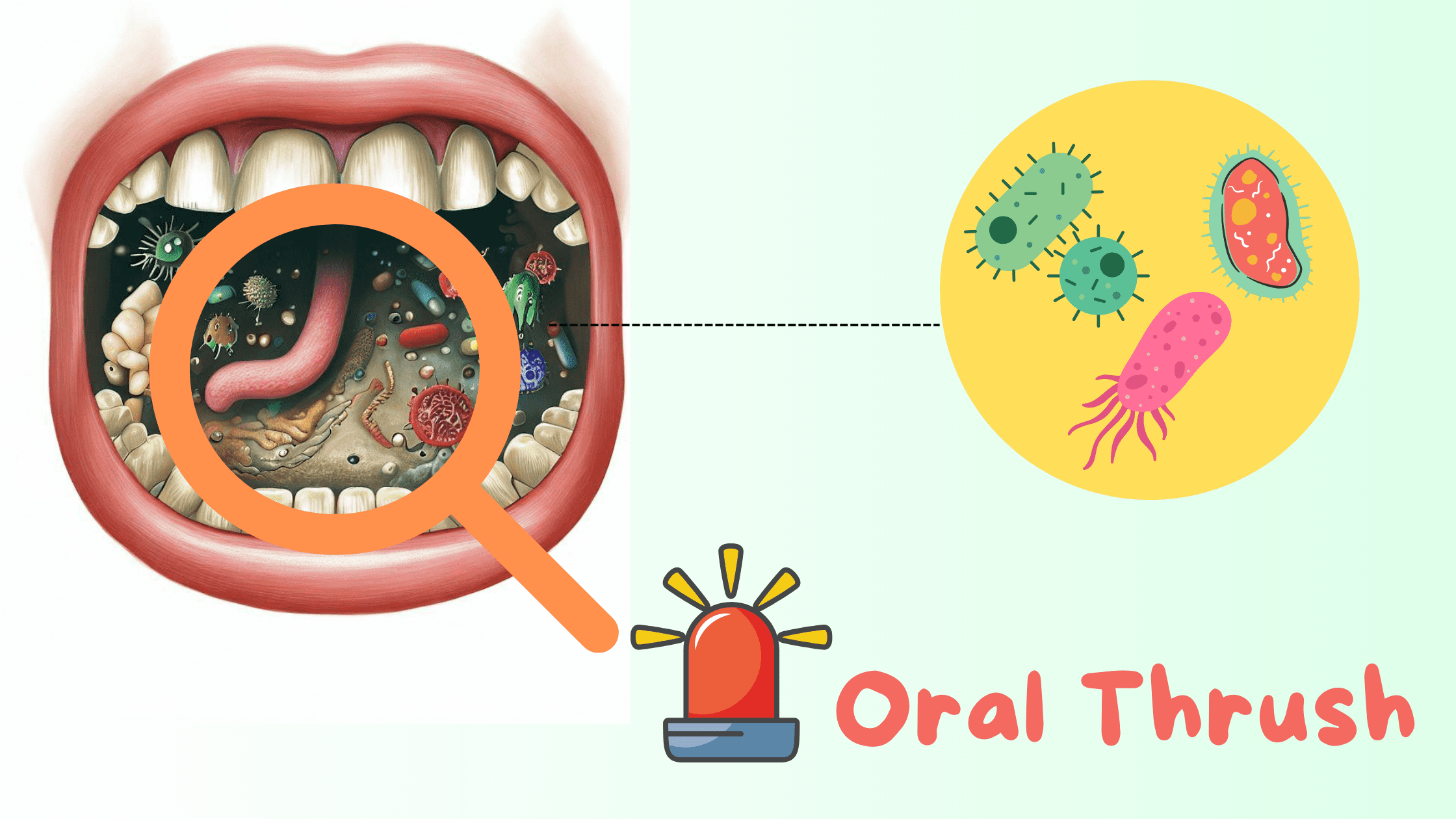 Oral thrush is a common fungal infection caused by a yeast called Candida albicans.
Oral thrush is a common fungal infection caused by a yeast called Candida albicans.
But Candida albicans itself isn’t the real problem.
In fact, 40 to 60% of healthy adults naturally carry this fungus in their mouths and digestive tracts without any issues.
That’s because when your immune system is working well, Candida albicans lives in balance with other friendly bacteria and microorganisms. It doesn’t cause any symptoms or infections.
The trouble starts when the immune system weakens. That’s when Candida can overgrow and cause an infection known as oral thrush (or oral candidiasis).
Keep reading to discover the main risk factors, early warning signs, and proven strategies to restore a healthy balance in your mouth.
In this article:
1. How Does Candida Albicans Lead to Oral Thrush?
2. Symptoms of Oral Thrush
3. What Causes Oral Thrush?
4. Oral Thrush Can Become Chronic
5. Can Oral Thrush Spread to the Body?
6. Other Oral Conditions That Resemble Candidiasis
7. Oral Thrush Home Treatment
8. When to See Your Dentist
9. How to Maintain an Optimal Oral Microbiome
How Does Candida Albicans Lead to Oral Thrush?
When Candida albicans grows out of control, it forms a thick biofilm—a kind of protective shelter that helps it survive and increases its resistance. This biofilm often appears as a thick white layer, one of the telltale signs of oral thrush.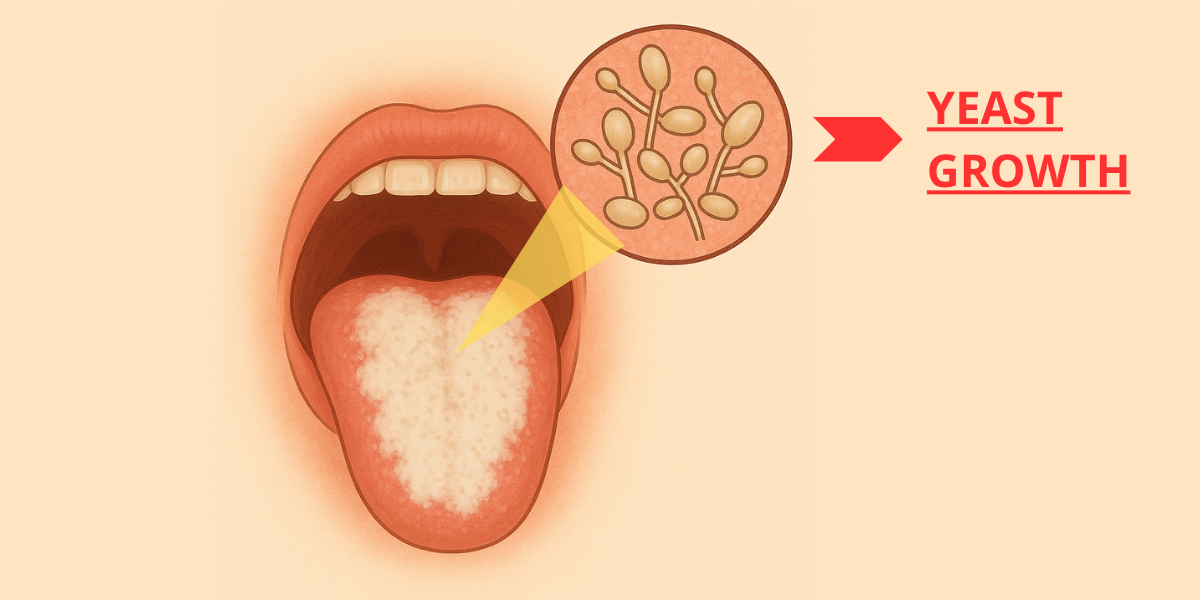
As Candida albicans thrives in the mouth, it can trigger hypersensitivity reactions and release toxins that help it invade deeper layers of the mouth lining.
The result is redness, sensitivity, a burning sensation, and general discomfort inside the mouth.
Oral thrush usually stays confined to the outer lining of the mouth, affecting areas like the tongue, inner cheeks, and lips. But if the immune system becomes severely weakened, the infection can spread beyond the mouth to other areas, such as the throat or even the lungs.
Symptoms of Oral Thrush
Oral thrush is just one of the many forms of the fungal infection, medically known as Acute Pseudomembranous Candidiasis.It can cause a wide range of symptoms, but it's most commonly recognized by a thick, creamy white or yellow coating in the mouth that resembles cottage cheese.
This coating can often be easily scraped off, revealing a red, tender, and inflamed surface underneath.
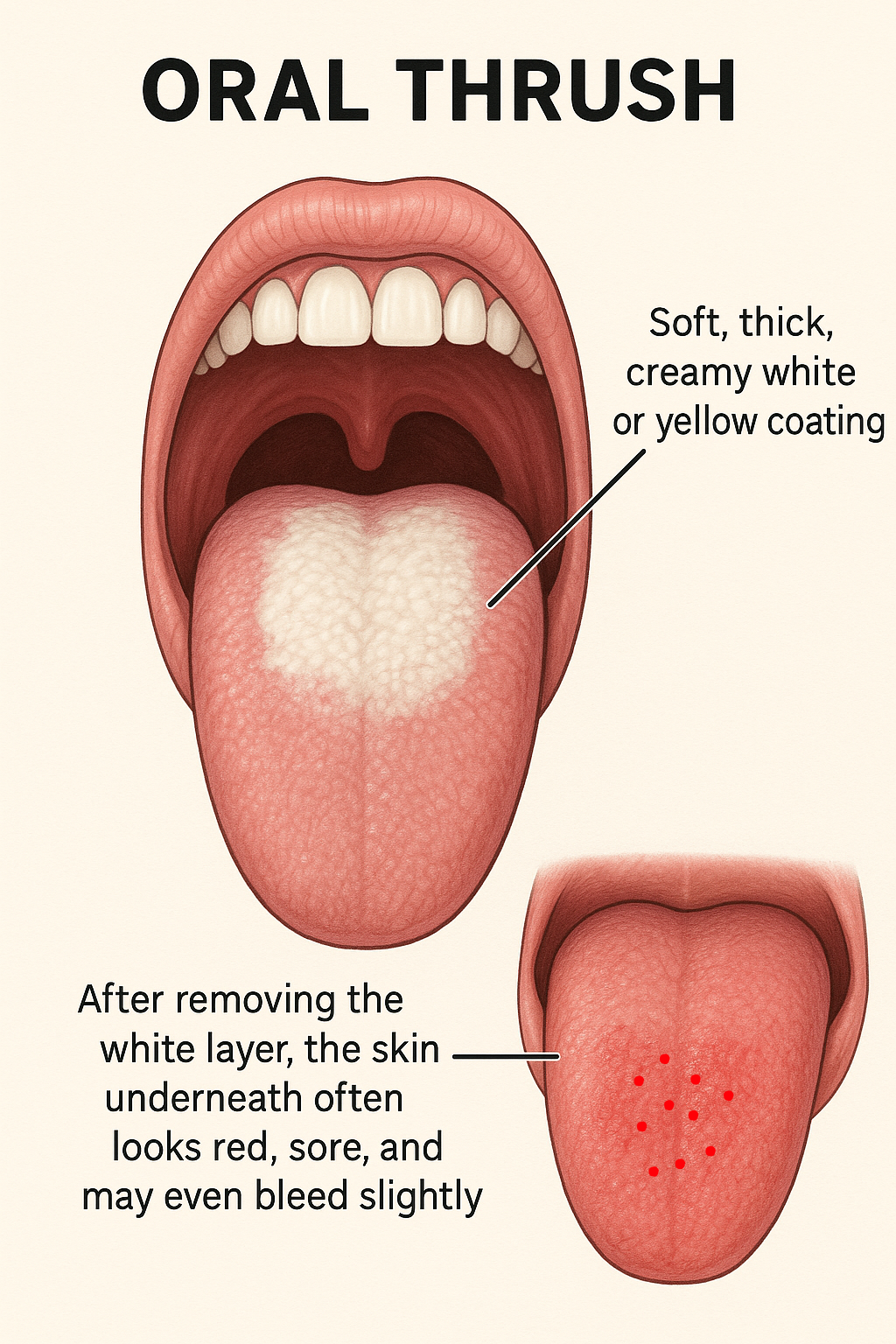
Other symptoms include a burning sensation, dry mouth, and altered taste — typically described as a metallic taste.
A less common form of the infection is called Acute Atrophic Candidiasis. It occurs when the white thick coating of oral thrush is lost. Symptoms include diffuse redness, along with pain, tenderness, and difficulty eating or swallowing.
What Causes Oral Thrush?
Oral thrush doesn’t have one specific cause. Instead, it develops due to underlying factors that weaken the immune system and disrupt the balance of the oral microbiome.
That’s why it’s more commonly seen in older adults and young children, whose immune systems is usually weaker than those of healthy young adults.
Some of the risk factors include:
- Anything that disrupts the oral microbiome: Factors like overusing strong mouthwashes, inappropriate antibiotic use, or a sugar-rich diet can all upset the delicate balance of the oral microbiome. This can help certain yeasts or harmful bacteria to grow, leading to infections.
- Poor oral hygiene: Not brushing and flossing regularly gives harmful bacteria and yeast the chance to grow and form biofilm on your teeth and oral surfaces. That’s why maintaining proper oral hygiene is essential to keep this biofilm in check and prevent buildup.
- Smoking: Smoking reduces blood flow to the tissues in your mouth, weakens the immune response, and creates an environment where harmful microbes can win out.
- Ill-fitting dentures: Candida albicans can survive on non-living surfaces as well, like dentures. In fact, denture wearers are at a higher risk of developing oral thrush than others.
- Dry mouth: Saliva is your mouth’s best natural defense. It helps clean away bacteria and yeast, preventing them from growing and forming plaque. When saliva flow is low, harmful microbes can overgrow, raising the risk of infection and many other dental issues.
- Sugar-rich diet: Sugars and other carbohydrates fuels the growth of oral yeast and harmful bacteria.
- HIV infection: People with HIV have weaker immune systems. Oral thrush is often one of the first noticeable mouth sign of HIV infection.
- Cancer and its treatment: Individuals with cancer, or those undergoing chemotherapy or radiotherapy, are more prone to oral issues like dry mouth and infections, including oral thrush.
Oral Thrush Can Become Chronic Over Time
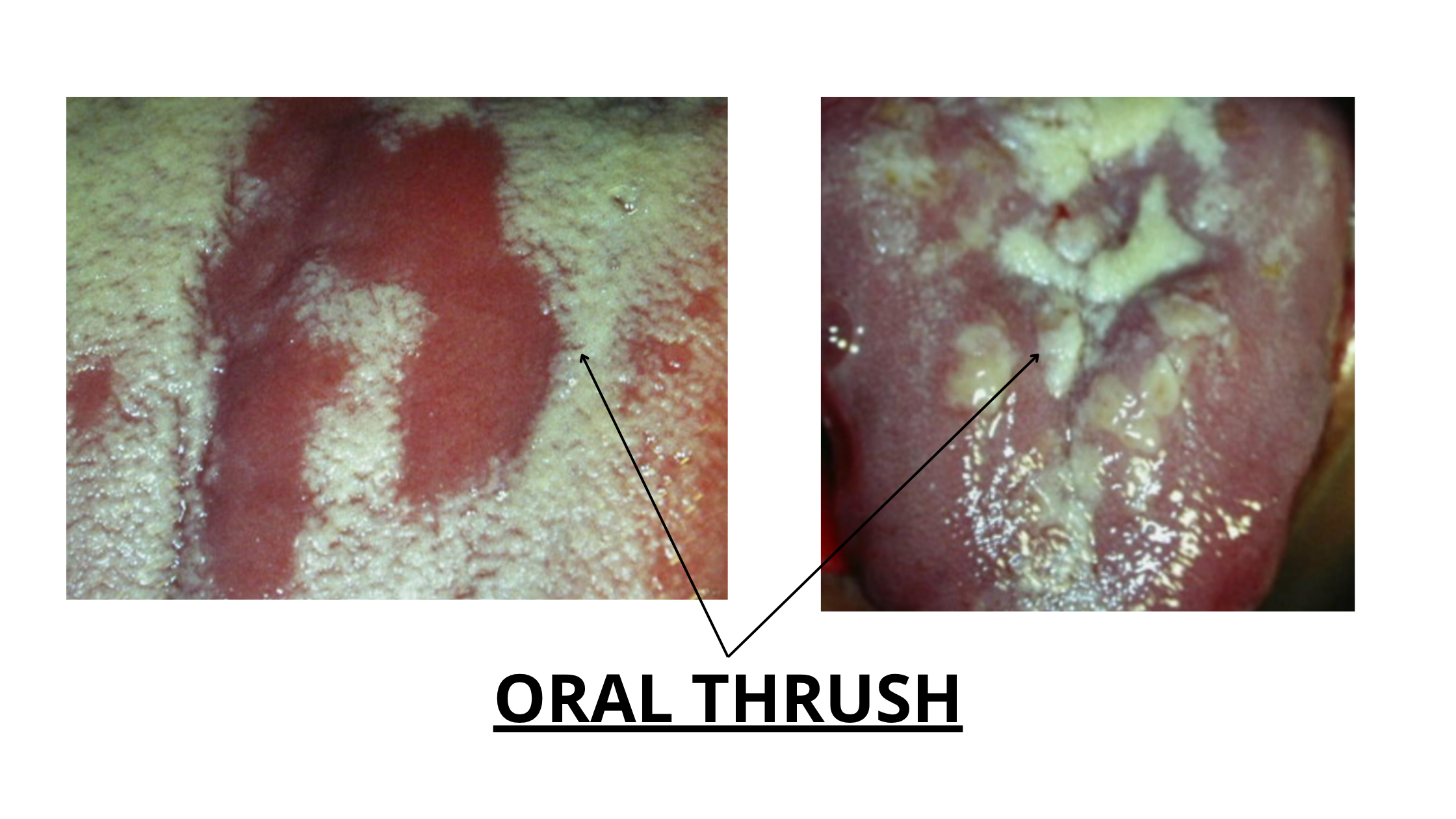
When the acute form of oral thrush persists or becomes resistant to treatment, it can develop into Chronic Candidiasis. This chronic form appears as thick, long-lasting, and irregular white patches with a rough surface.
Unlike the acute version, the white plaques of chronic candidiasis cannot be wiped away. This is because the thickening isn’t caused by a buildup, but by overproduction of keratin, a tough protein produced by the underlying cells.
Unlike the acute version, the white plaques of chronic candidiasis cannot be wiped away. This is because the thickening isn’t caused by a buildup, but by overproduction of keratin, a tough protein produced by the underlying cells.
This leads to increased tissue thickness, a condition known as hyperkeratosis. In rare cases, these lesions may even carry the risk of malignant transformation (cancer).
Another form of chronic candidiasis is Angular Cheilitis, which affects the corners of the mouth where the lips meet. It results in soreness, redness, and cracks at the corners of the mouth that may extend onto the surrounding skin, causing both discomfort and cosmetic issues.
Can Oral Thrush Spread to the Body?
Oral thrush is mostly harmless, remains confined to the mouth, and usually clears up within a few days or weeks after treatment and addressing the underlying cause.However, in some people with certain medical conditions, especially those with weak immune responses, complete recovery may take longer. In rare cases, the infection can spread beyond the mouth, leading to serious complications.
The fungal infection may extend to the throat, lungs, heart (Candidal Endocarditis), or brain (Candidal Meningitis). However, this is very unlikely.
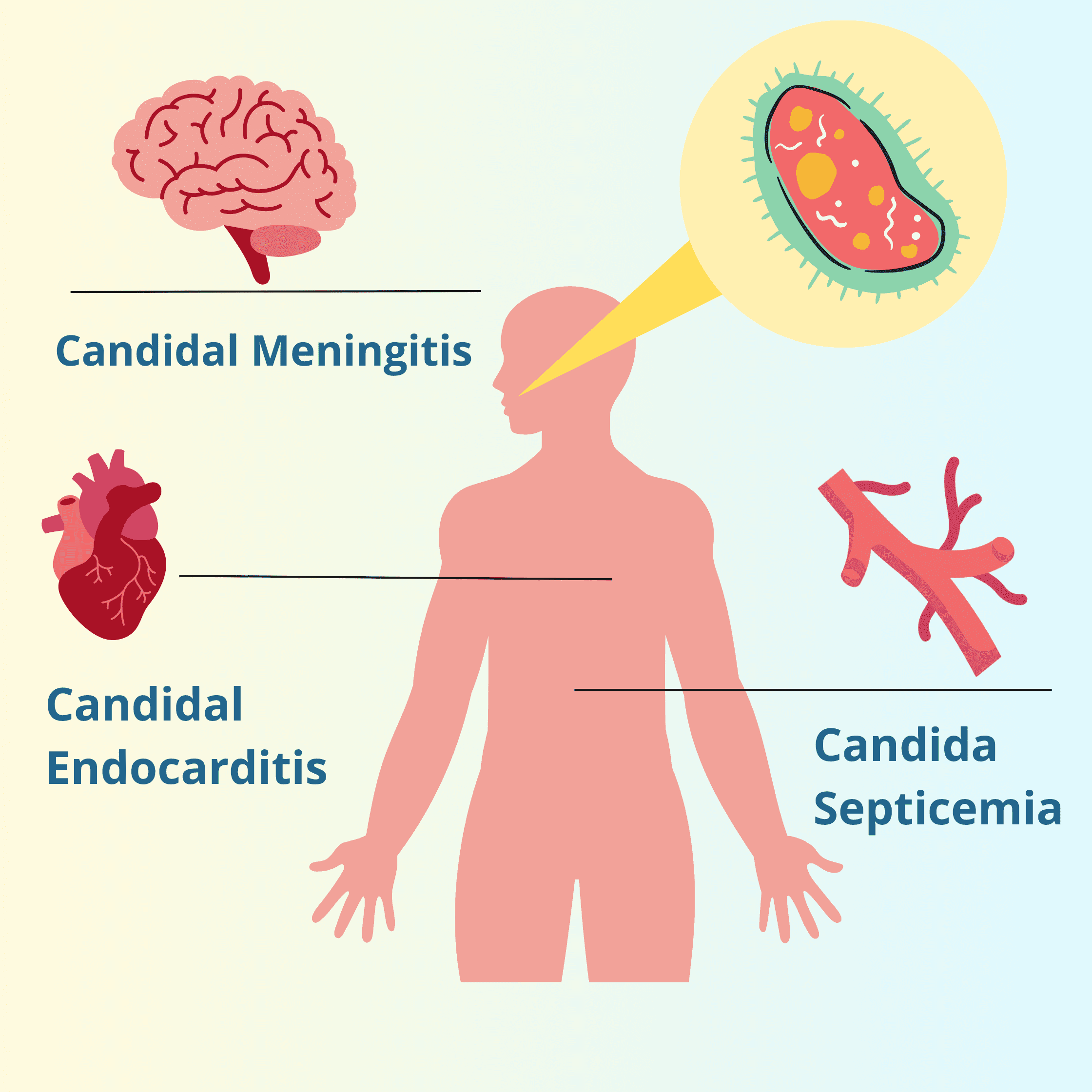
If the fungus enters the bloodstream and spreads throughout the body, it can lead to a life-threatening condition known as Candida Septicemia, where the body reacts with a severe inflammation.
Other Oral Conditions That Resemble Candidiasis
Several oral conditions can look like oral thrush, causing white patches and discomfort. These include:- Leukoplakia: White or grayish patches that can appear in any area of the mouth. Some may be precancerous.
- Lichen Planus: Autoimmune condition causing white patches, redness, or sores in the mouth.
- Geographic Tongue: Tongue with changing map-like patterns, often painless.
- Traumatic Ulcers:Painful mouth sores from physical injury or irritation. Usually, they heal on their own after removing the trigger.
- White coated tongue: A common and usually harmless condition where the surface of the tongue appears white or yellow due to a buildup of dead skin, food debris, and bacteria. It most often occurs when you don't brush or clean your tongue regularly.
A thorough examination by your dentist is crucial to rule out these conditions before diagnosing oral thrush.
Oral Thrush Home Treatment
Treatment mostly depends on the severity of the infection and your overall health.
Most cases are mild and may not require specific treatment, aside from some home remedies. These may include:
Most cases are mild and may not require specific treatment, aside from some home remedies. These may include:
- Improve your oral hygiene.
- Rinse your mouth several times a day with a baking soda solution: mix half a tablespoon of baking soda in a glass of water.
- Treat dry mouth by staying hydrated and chewing sugar-free gum.
- Reduce or quit smoking.
- Limit sugar intake in your diet.
- If a medication is suspected to be a cause, talk to your doctor about replacing it or adjusting the dosage.
When to See Your Dentist
If your symptoms do not improve after 14 days, seek professional help as soon as possible.
The main treatment usually involves applying antifungal creams or gels directly to the affected areas. It’s best to use these medications between meals and keep them in contact with the patches for as long as possible. Treatment typically lasts from one to three weeks.
The main treatment usually involves applying antifungal creams or gels directly to the affected areas. It’s best to use these medications between meals and keep them in contact with the patches for as long as possible. Treatment typically lasts from one to three weeks.
In more severe cases or if you have an underlying condition, your doctor may recommend antifungal tablets in addition to the topical treatment.
How to Maintain an Optimal Oral Microbiome
Preventing oral thrush begins with maintaining a healthy oral microbiome, which means strengthening your immune system and promoting friendly bacteria.Here are some tips:
- Maintain Good Oral Hygiene: Brush your teeth at least twice a day with a soft toothbrush and floss daily to remove biofilm from the surfaces of your teeth and gums. This biofilm is a primary culprit behind many mouth infections, including cavities, gum disease, and thrush.
- Clean Your Tongue: The tongue can trap plaque and food debris. If not cleaned regularly, a white coating can form, leading to issues like bad breath. Use a toothbrush or, even better, a tongue scraper once a day to keep your tongue clean.
- Check Your Overall Health: Medical conditions and medications, such as diabetes, HIV infection, cancer treatments, antibiotics, and corticosteroids, can weaken your immune system and promote Candida albicans overgrowth in your mouth. Remember, your mouth is a window on your body; what happens in your mouth can reflect your overall health, and vice versa.
- Watch Your Diet: Cutting back on sugar helps stop feeding the yeast and harmful bacteria in your mouth. Instead, focus on foods rich in vitamins and minerals to support your immune system. Eating probiotic-rich foods like yogurt, kefir, and cheese can also lower Candida levels and boost the good bacteria in your mouth (and gut).
- Stop Using Strong Antibacterial Products: Using strong mouthwashes too often can upset the natural balance of bacteria in your mouth. While they may help short-term with conditions like gum disease, long-term use can do more harm than good.
- Oil Pulling: This involves swishing oil in your mouth for 15 to 20 minutes, then spitting it out and rinsing. It has been shown to significantly reduce the number of harmful microbes in the mouth. You can use any oil, but coconut oil and olive oil are the best choices if you’re looking for antifungal benefits.
- A Color Handbook of Oral Medicine De Richard C. K. Jordan, Michael A. O. Lewis
- Essential Of Oral Pathology - Book by Swapan Kumar Purkait
- Relationship between oral hygiene and fungal growth in patients: users of an acrylic denture without signs of inflammatory process - PMC (nih.gov)
- Candidal Leukoplakia | Exodontia
- SciELO - Brasil - Effect of sodium bicarbonate on Candida albicans adherence to thermally activated acrylic resin Effect of sodium bicarbonate on Candida albicans adherence to thermally activated acrylic resin
- Could probiotics help with oral thrush? | Professionals (optibacprobiotics.com)