Oral lichen planus: A Mysterious Mouth Condition
Lichen planus is among the conditions labeled as idiopathic, meaning they arise without a clearly identifiable cause. While it can manifest anywhere in the body, from hands and feet to the scalp and nails, the mouth is the most commonly affected site. In this article, we will look at the essential facts about this mysterious condition.
In this article:
1. What is Oral Lichen Planus?
2. Quick Lichen Planus Facts
3. The Different Forms of Oral Lichen Planus
4. Symptoms of Oral Lichen Planus
5. What Factors Can Worsen Oral Lichen Planus Lesions?
6. Risk Factors for Malignant Transformation
7. Oral lichen planus treatment
What is Oral Lichen Planus?
Oral Lichen Planus is a chronic inflammatory condition affecting certain body parts, particularly the lining tissues like skin and mucous membranes. Mucous membranes or mucosa are the soft tissues lining the inside of cavities and organs throughout the body, such as the mouth, digestive tract, and genital area.This condition remains a mystery because its exact cause is still unknown. But what we do know is that it involves your immune system acting unusually, attacking its own cells.
The result? Lesions showing up in many forms - white patches, lines, red spots, open sores, and inflammation.
About 77% of people dealing with lichen planus experience these lesions in the mouth. And while it can appear anywhere, the inside of your cheeks is the most frequent target. One of the telltale signs of the condition is the symmetry of lesions, affecting both sides of the mouth.
Lichen Planus is not cantagious. It is a disorder that occurs inside the body, rather than a viral or bacterial infection.
Although the World Health Organization (WHO) classifies it as a potentially malignant oral disease, the actual risk is too low, ranging from 0 to 2% according to studies. Still, to be on the safe side, it's always a good idea to check your symptoms with your doctor, whatever changes you notice in your mouth.
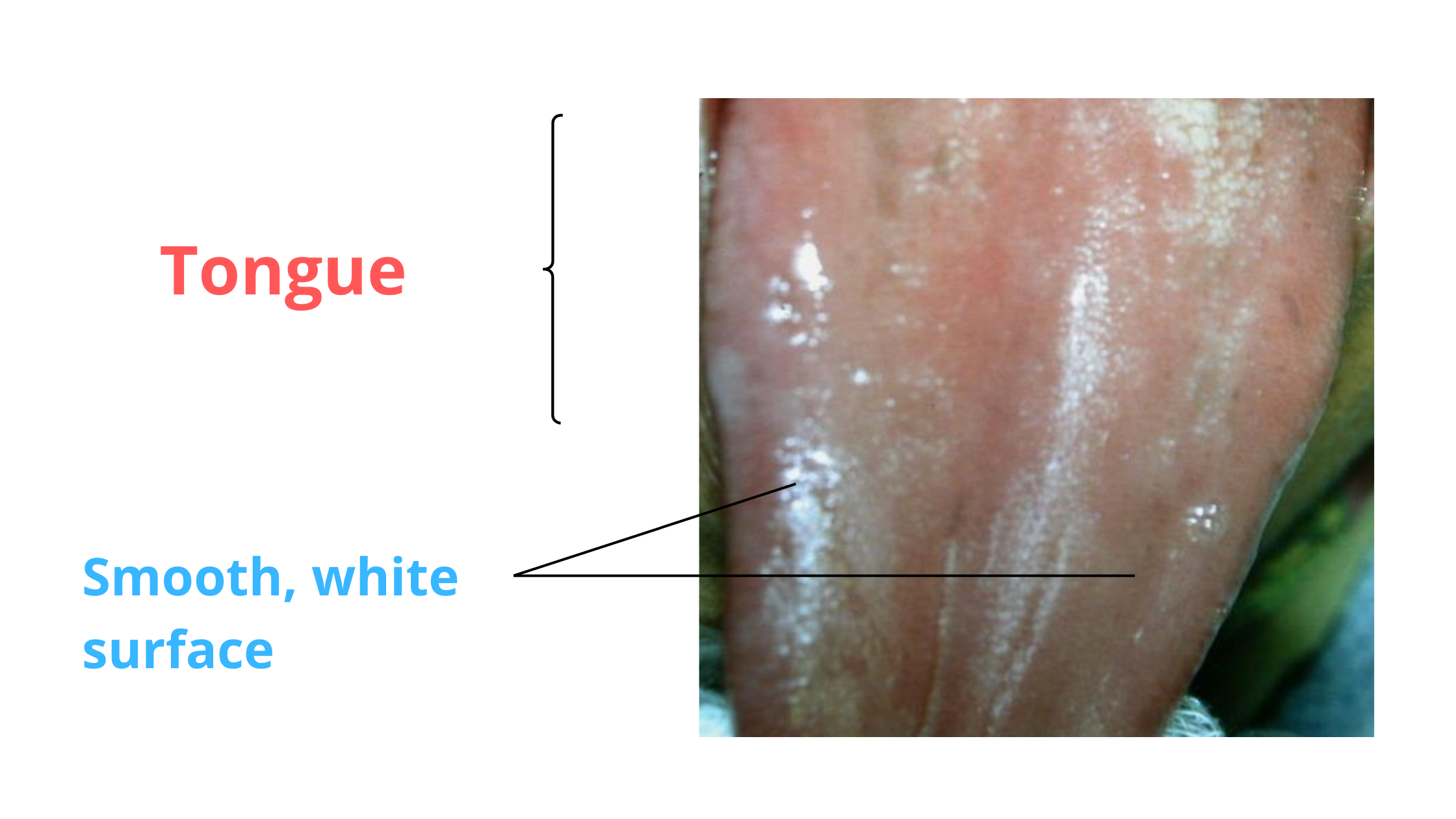
Lichen planus lesion on the surface of the tongue
Quick Lichen Planus Facts
- Lichen Planus affects 0.5% to 2.0% of the population.
- Females have double the risk compared to males.
- It generally appears in middle-aged and elderly people, between the ages of 30 and 60.
- Children are the least affected.
- It's mostly benign, and the chances of it turning into oral cancer are exceptionally low.
The Different Forms of Oral Lichen Planus
Oral Lichen Planus presents in various forms, but sometimes multiple subtypes can coexist simultaneously. The three most common are the Reticular, Erosive, and Plaque Types.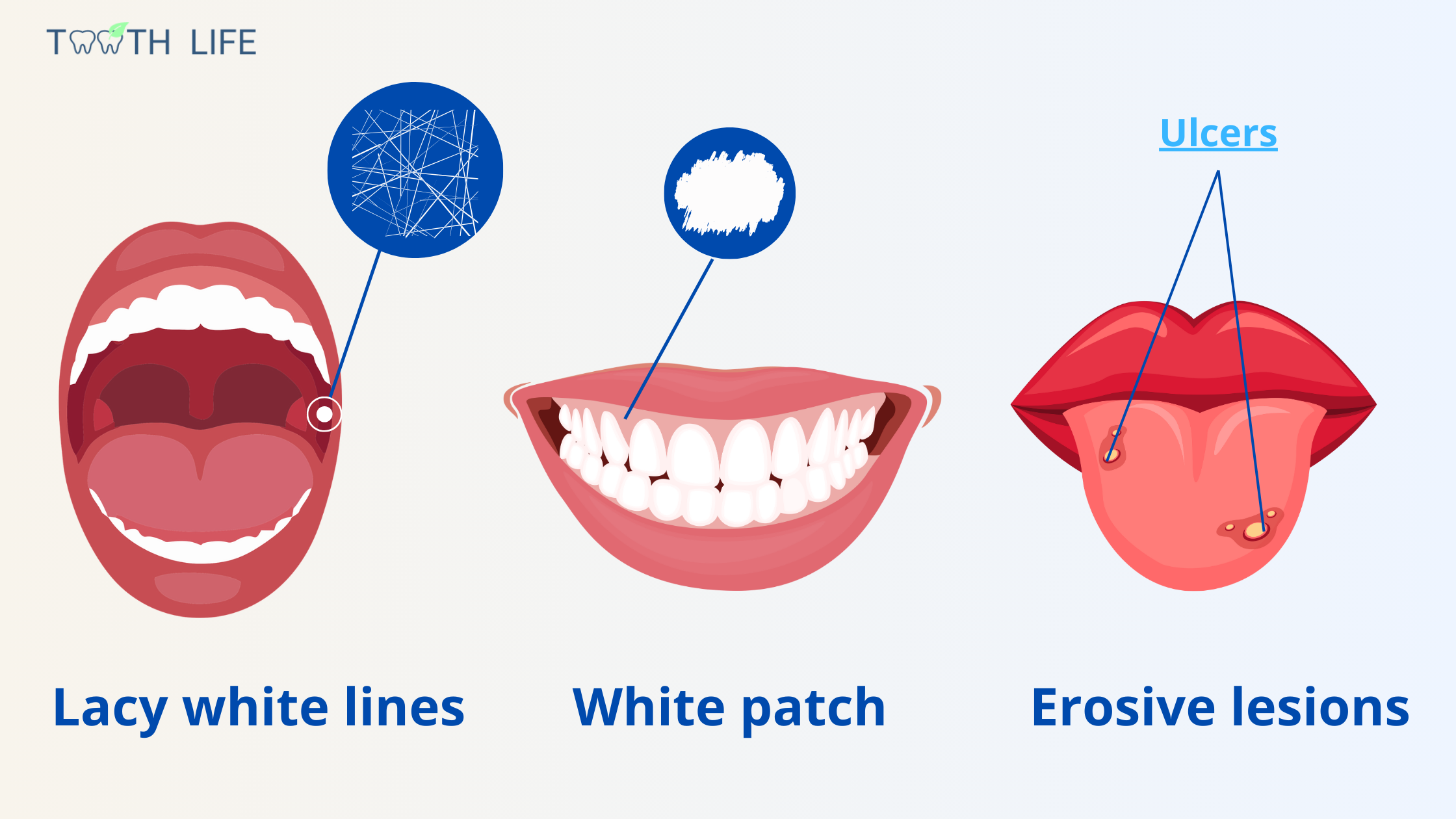
1. Reticular Type:
The reticular type is the most common form. It is characterized by tiny white lines that interlace, forming a distinctive lace-like pattern known as Wickham striae.
These white lines typically appear inside the cheeks and result from the overproduction of keratin. They often arise symmetrically, affecting both the right and left sides of the mouth.
While often asymptomatic, the lacy white lines may occasionally cause discomfort.
2. Erosive Type:
Erosive Lichen Planus shows up as red, painful patches caused by the immune system attacking and breaking down the outer lining of the mouth. The erosive lesions can look similar to canker sores, except that they are larger with irregular margins.
They can also manifest as thickened areas with redness and ulceration, which may be covered by a whitish or yellowish layer, indicating tissue death (necrosis).
During flare-ups, the sores can cause intense discomfort, often described as a burning feeling, especially when eating hot or spicy foods.
3. Plaque Type:
The plaque lesions present as raised or flattened white areas on the mucosa with irregular margins. They are mostly seen on the tongue and inside the cheeks.
These white patches can look like Leukoplakia, another potentially malignant oral condition.
Symptoms of Oral Lichen Planus
Oral Lichen Planus often shows no symptoms initially, as its onset is usually gradual and mild. However, as it progresses, you might start noticing a few signs.As the lines or patches thicken, the lining of your mouth might feel rough. Discomfort tends to set in, especially with the erosive and ulcerative forms.
These symptoms can fluctuate, intensifying during flare-ups and subsiding during remission phases. During the flare-up period, you might experience:
- Burning Sensation and Pain.
- Sensitivity to Hot, Acidic, or Spicy Foods.
- Touching the lesions may result in bleeding.
- Painful, thick patches.
- Everyday activities like talking, eating, or swallowing might become challenging during symptomatic periods.
What Factors Can Worsen Oral Lichen Planus Lesions?
Since Oral Lichen Planus is caused by an abnormal immune reaction, anything that affects this response or worsens inflammation can trigger or worsen flare-ups. Here are the main suspected risk factors:- Psychological factors like stress and anxiety.
- Hepatitis C and B virus.
- Hypertension and diabetes.
- Allergic reactions to dental materials like amalgam, composite, and nickel-cobalt.
- Immune reactions after transplant.
- Some medications, including antihypertensives, hypoglycemics, and non-steroidal anti-inflammatory drugs.
Risk Factors for Malignant Transformation
Malignant transformation of oral lichen planus is a controversial topic, with varying reports on risk factors and associated mechanisms.While some studies suggest a risk of up to 5%, others propose that malignant transformation may occur independently of lichen planus.
But what is certain is that lichen planus involves chronic inflammation, a condition linked to various forms of cancer.
The following risk factors may contribute to cancerous changes in oral lichen planus lesions:
Erosive and Ulcerative Forms
Most cases of oral lichen planus that become malignant usually appear as ulcers or erosions. The reason might be because these lesions make the oral mucosa more vulnerable and exposed to carcinogens.
90% of oral cancers are known as squamous cell carcinomas. The most common symptom is an ulcer that doesn't heal, even after several weeks. It may look like a canker sore, but cancerous ulcers are usually irregular, protruding, aggressive, and hard to the touch.
So, if you notice that an ulcer persists for more than two weeks, don't wait to have it checked by your dentist.
Involvement of the Tongue
The tongue, particularly its sides, is a common site for oral cancer. Any persistent lesions in this area of your mouth deserve to be examined.
Smoking and Alcohol
Smoking and excessive alcohol use harm both your overall and oral health. Although their direct role in the malignant transformation of oral lichen planus isn’t proven, people who both smoke and drink heavily are 30 times more likely to develop oral cancer.
Mouth Infections
Certain mouth infections, such as the human papillomavirus type-16 and chronic Candida albican infection (candidiasis or oral thrush), have been identified as risk factors for oral cancer.
Treating existing oral infections should also be part of lichen planus treatment.
Oral Lichen Planus Treatment
Lichen planus is a chronic condition that can’t be completely cured, but there are several ways to ease symptoms and reduce flare-ups.Mild and symptom-free reticular oral lichen planus usually doesn’t need treatment. But regular check-ups are important to watch for any changes.
For more widespread, ulcerative, and painful lesions, treatment focuses on managing risk factors, ease symptoms, and lower the risk of potential malignant transformation.
1. Managing Risk Factors
This involves identifying possible causes of the lesions and addressing them.
- Diagnose and Treat Underlying Health Conditions: Conditions like liver disease, diabetes, hypertension, or viral infections should be diagnosed and treated.
- Managing Psychological Factors: Reducing stress and anxiety can help reduce lichen planus episodes.
- Addressing Local Irritants: This might include quitting smoking and heavy drinking, treating cavities, or fixing an old filling or crown that's irritating your mouth.
- Stopping or Replacing Certain Medications: If a specific drug is suspected, replacing it with an alternative may resolve the symptoms.
2. Symptomatic Treatment
To ease symptoms, the following approaches can be considered:
- Topical Corticosteroids: The first-line treatment involves using corticosteroids in the form of mouthwash, ointment, or gel applied directly to the lesions.
- Systemic Corticosteroids: If topical treatment fails or the condition is widespread, oral corticosteroid tablets may be prescribed.
- Topical Numbing Agents: For painful ulcers, your doctor may recommend numbing agents like lidocaine to relieve discomfort.
3. Prevention
Lichen planus can be challenging to control as the underlying cause is unknown. However, certain factors seem to aggravate the condition, and that's where we can take action.
Start by effectively managing periods of heightened stress, and most importantly, don't let the condition take over your mental health.
Improve your diet and oral hygiene with regular brushing, and avoid bad habits and certain foods that can make your symptoms worse.
You should also keep a close eye on your mouth, noting any new lesions and monitoring their progress, whether they regress, worsen, are painful, or are asymptomatic.
In case any lesion persists or causes discomfort for more than two weeks, see your doctor or dentist as soon as possible.
If the lesion has changed or looks unusual, your dentist or doctor may recommend a biopsy to check for any signs of cancer or precancerous changes.
- Oral lichen planus - PMC (nih.gov)
- Oral Lichen Planus: an Overview of Potential Risk Factors, Biomarkers and Treatments - PMC (nih.gov)
- Oral lichen planus: a literature review and update - PubMed (nih.gov)
- The possible premalignant character of oral lichen planus and oral lichenoid lesions: a prospective study - PubMed (nih.gov)
- Mouth Cancer Action Month: Mouth cancer risk factors (dentalhealth.org)
- Oral squamous cell carcinoma: clinicopathological features from 346 cases from a single Oral Pathology service during an 8-year period - PMC (nih.gov)