What is this white line that suddenly appeared on my gums?
 If you suddenly see a white line on your gums and aren’t sure why it’s there, start by thinking about when and how it first appeared.
If you suddenly see a white line on your gums and aren’t sure why it’s there, start by thinking about when and how it first appeared.
These white lines can be caused by many things, including trauma (or chronic irritation), recent dental procedure (like a tooth extraction), certain medications, or gum disease. Other times, they may come from oral conditions that don’t have a clear cause.
While many of these white lines are harmless and even temporary, some can rarely develop into more serious problems if ignored.
We will discuss 8 possible reasons for white lines on your gums — and what you can do about each one.
In this Article: 8 Causes of White Lines on Gums
1. Early sign of receding gums caused by chronic irritation
2. Tartar accumulation
3. After extraction or oral surgery
4. Oral thrush
5. Leukoplakia
6. Lichen planus
7. Gum disease
8. White lesions due to tobacco use
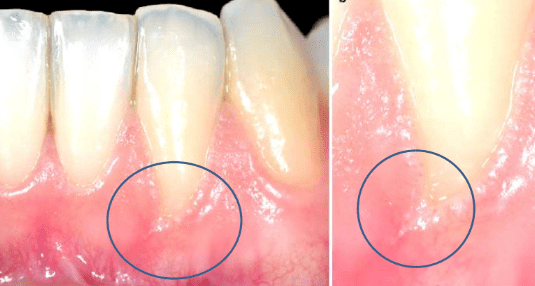
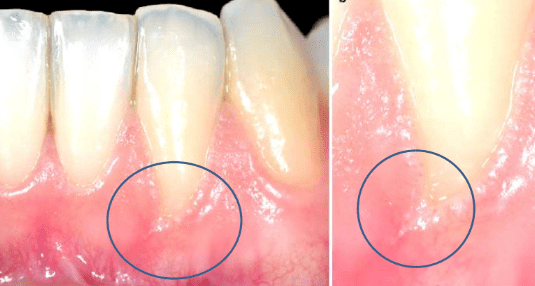
1. Early sign of receding gums caused by chronic irritation
Two main triggers can cause your gums to recede and pull away from your teeth: plaque buildup and trauma.One of the earliest signs of receding gums is a white or red line along your gum line, especially when chronic trauma or ongoing irritation is the cause. This most often happens from brushing too aggressively or using a hard-bristled toothbrush.
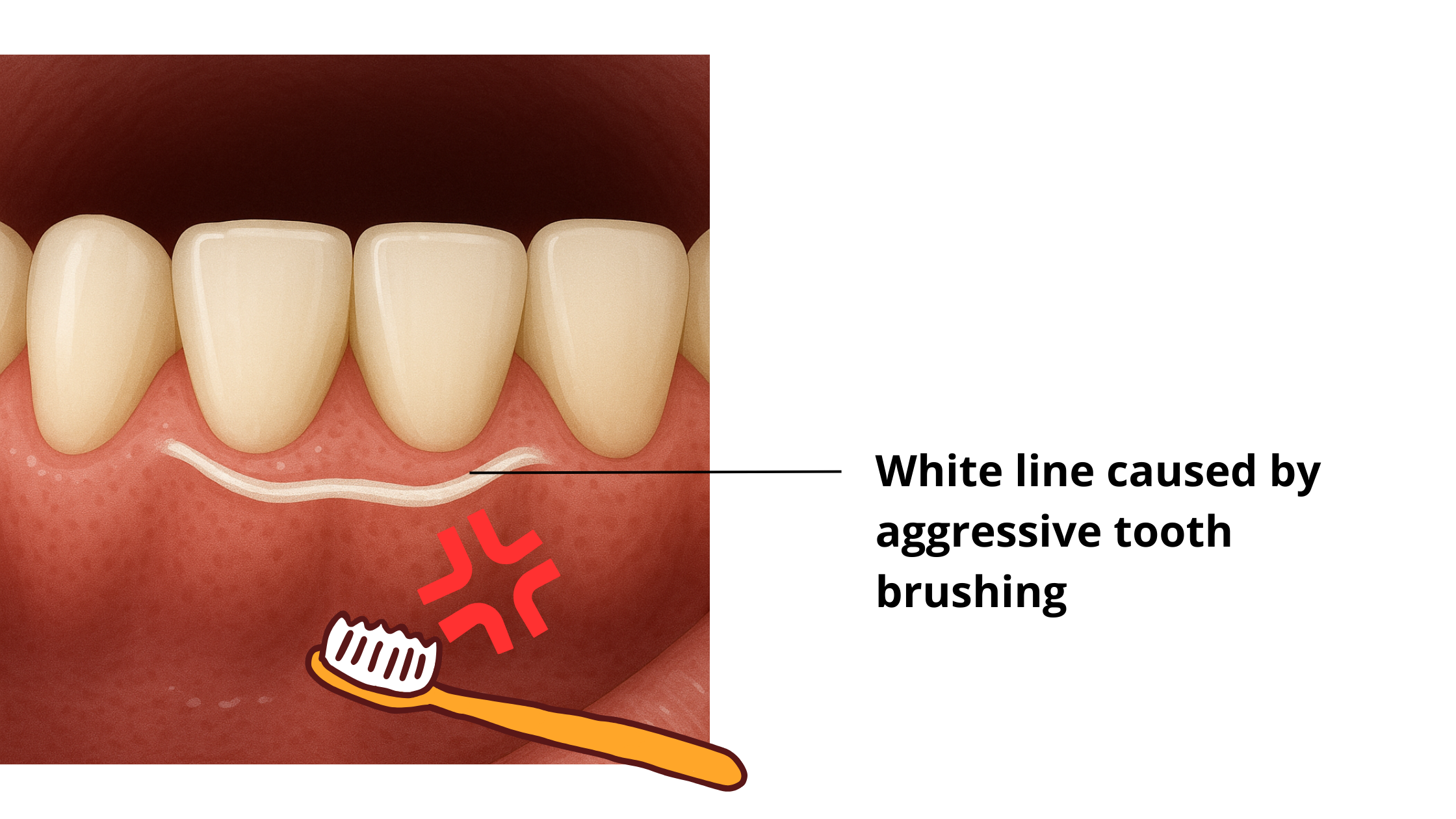
How can you tell if you’re brushing too hard? Take a look at your toothbrush bristles. If they look frayed and worn out, chances are you’re using too much pressure.
The areas most likely to be affected are the gums near your upper canines and premolars, since these spots tend to get extra pressure during brushing.
These small but repeated injuries can damage your gums and first appear as white or red lines that can sometimes be painful. Over time, they may turn into small grooves or fissures known as Stillman’s Cleft.
Other things that can injure your gums and lead to these white lines include wearing a tongue or lip piercing or overusing toothpicks.
These could be early signs of gum recession. But the good news is, they’re completely reversible. Once you remove the cause of the irritation or injury, the gums will heal on their own.
But if ignored, the problem can get worse and lead to more widespread gum recession.
What you can do about white lines caused by gum injury
The first thing to do is to spot and stop what's irritating your gums. Start by brushing your teeth gently with a soft bristle toothbrush.
Also, be sure to visit your dentist for a checkup. You may need a professional cleaning to remove tartar or other buildup from your teeth and along the gum line.
Getting rid of the root cause is usually all it takes to stop the damage — and even reverse it in the early stages.
2. Tartar accumulation
Plaque is a soft, whitish film full of bacteria that naturally builds up on your teeth over time. If you don’t remove it regularly by brushing, minerals from your saliva and food can harden it, turning it into calculus, also known as tartar.Tartar can build up both above and below your gum line. It often looks like a white-yellow deposit that’s tough to remove on your own. Over time, it can darken and turn brown or even black as it absorbs pigments from food and drinks.
Because tartar sticks firmly to your teeth, the only way to get rid of it is through a professional dental cleaning, known as scaling.
3. White line after extraction or oral surgery
After surgery—especially if your dentist has cut and stitched your gums, like after a gum graft or wisdom tooth extraction—you need to give your tissues time to heal properly.In the early stages of healing, your gums might look unusual: white, swollen, or even bleeding.
These are completely normal and temporary and should gradually improve as your gums heal.
Usually, your gums will return to their normal look within 2 to 4 weeks, depending on how complex the procedure was.
In rare cases, a whitish or pale pink line of scar tissue may remain permanently at the surgery site. This is more common in older adults, smokers, and people with diabetes, as the body’s ability to heal is reduced.
4. Oral thrush
Oral candidiasis, also known as oral thrush, is an infection caused by a type of yeast called Candida albicans.In healthy mouths, Candida albicans live peacefully alongside bacteria and other microorganisms.
But certain factors can upset this balance, leading to an overgrowth of Candida albicans. These include:
- Poor oral hygiene
- Wearing old or poorly fitting dentures
- Dry mouth
- Excessive use of antibiotics or mouthwash
- Long-term use of corticosteroids
- Chemotherapy or radiotherapy
- Some diseases and viral infections, such as diabetes and HIV
Oral thrush can cause soft, thick, creamy white or yellow patches inside your mouth that often look like curdled milk or cottage cheese. These patches can appear anywhere on the pink lining inside your mouth.
It typically starts on the tongue and the inside of your cheeks, but can also spread to the gums and the roof of the mouth.
You might also notice other symptoms like redness, dry mouth, burning sensation, bleeding, or difficulty eating.
How is oral thrush managed?
The treatment for oral thrush depends on how severe it is.
For mild cases in healthy individuals, treatment usually involves applying topical antifungal creams or gels directly inside the mouth.
In moderate or severe cases, treatment may include both local antifungals and oral (systemic) medications.
5. Leukoplakia
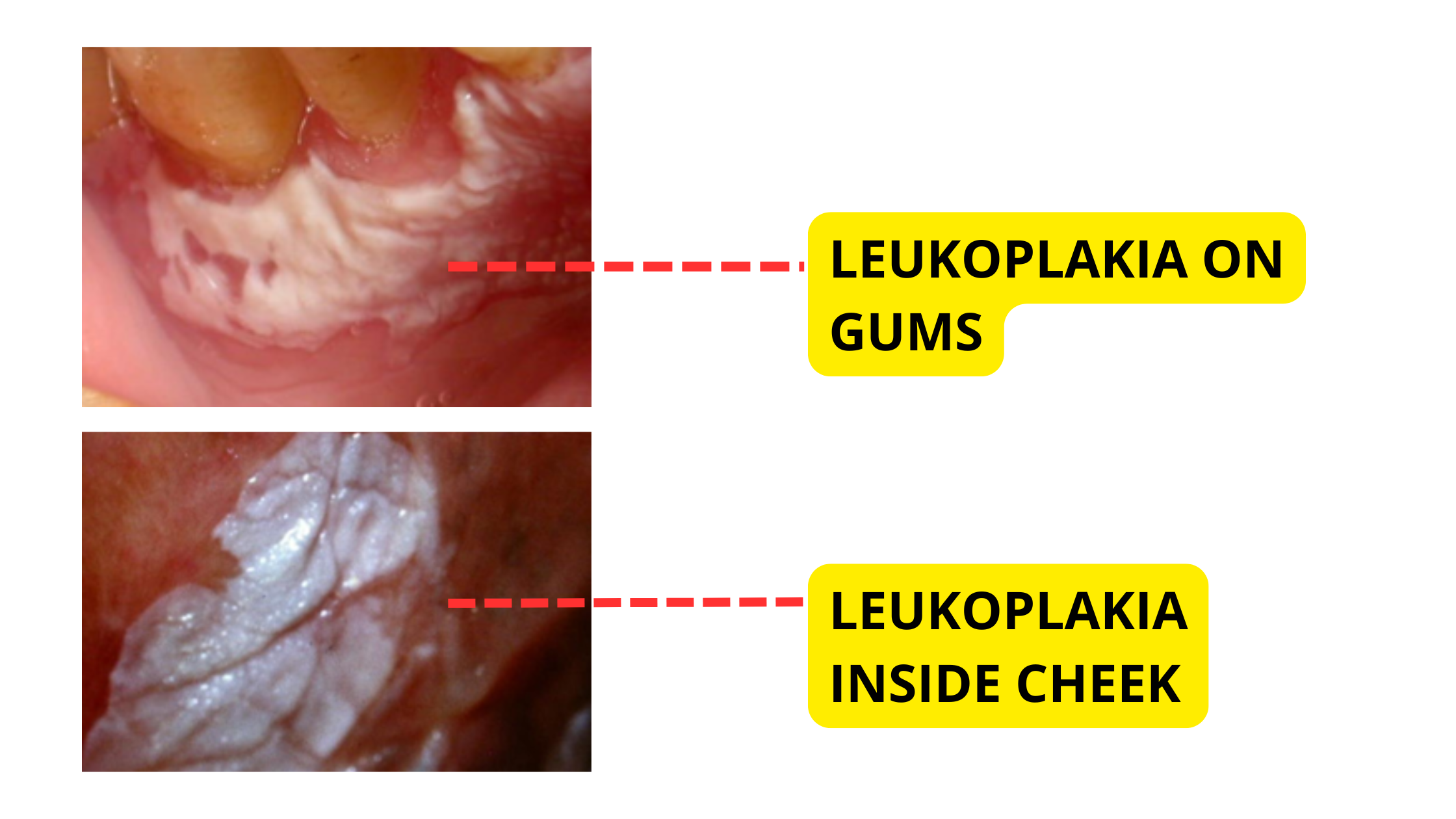 Leukoplakia is a condition that causes white patches inside the mouth that cannot be rubbed off. It affects roughly 1 to 2% of the general population.
Leukoplakia is a condition that causes white patches inside the mouth that cannot be rubbed off. It affects roughly 1 to 2% of the general population.
These patches form when the mouth lining becomes thicker and produces too much keratin—a protective protein that helps shield your tissues from damage.
That happens when your mouth overreacts to constant irritation or injury by building up a thicker layer of keratin. It’s the body’s way of protecting itself from ongoing stress.
The most well-known cause of leukoplakia is smoking and tobacco use. Other factors that can contribute include:
- Alcohol.
- Oral thrush.
- Viral infection.
- Hormonal imbalance.
- Chronic Trauma or irritation.
- Some nutrient deficiencies.
The areas most often affected by leukoplakia are the inside of the cheeks, followed by the tongue, lips, roof of the mouth, and gums.
Most leukoplakia lesions are harmless and not cancerous. However, in some cases, they can show early signs of cancer. That's why they need to be monitored regularly to spot any potentially serious changes early.
How is leukoplakia managed?
Leukoplakia cannot be diagnosed by appearance alone. A biopsy is necessary because many conditions, including oral cancer, can look similar.
If the biopsy shows no signs of cancer or precancer, no treatment is needed—just regular checkups every six months.
If the patch is suspected to have precancerous potential, the best approach is to eliminate risk factors like smoking and alcohol and to treat any underlying infections. Surgical removal may sometimes be the best approach to eliminate the risk.
6. Lichen planus
Lichen planus is an inflammatory condition that happens when the immune system mistakenly attacks the keratin-producing cells in the lining of your mouth.As a result, your body produces excess keratin, forming the typical white, lacy lines or patches. These most commonly appear on the tongue, gums, and the inside of the cheeks.
This autoimmune disease is fairly common, affecting about 1–2% of people worldwide.
The exact cause of lichen planus is still unknown, but stress is thought to make flare-ups worse.
Like leukoplakia, lichen planus lesions should be monitored regularly, as they can sometimes develop into precancerous changes, especially in the presence of risk factors such as smoking or alcohol consumption.
How is lichen planus managed?
Treatment focuses on eliminating any potential triggers, such as stress, certain medications, or allergies.
In the short term, topical anti-inflammatory creams or steroid gels can help reduce symptoms and provide relief.
7. Gum disease
Gum diseases are inflammatory conditions caused by bacteria that damage the tissues around your teeth, including your gums, bones, and ligaments.White or red patches along your gum line, along with swelling and bleeding, can be an early sign of gum disease. This initial stage is called gingivitis, which simply means inflammation of the gums.
If left untreated, gum disease can worsen and start destroying the tissues that support your teeth. This advanced stage is called periodontitis, and it’s the leading cause of tooth loss in adults.
One of the rarest and most severe forms is necrotizing ulcerative gingivitis (NUG). This painful condition tends to progress aggressively and rapidly.
It usually starts by affecting the triangular-shaped gum tissue between your teeth. Early on, you might see red, painful spots covered with a grayish-white layer, which can quickly turn into ulcers.
At advanced stages, the gum tissue between your teeth can be destroyed entirely, and the damage may spread to the surrounding gums.
Other symptoms of NUG include bad breath, fever, and swollen lymph nodes. People with weakened immune systems are the most affected. Among the risk factors:
- HIV infection.
- Stress.
- Smoking.
- Poor oral hygiene.
How is gum disease managed?
In the early stage of gingivitis, gum disease is completely reversible. All it takes is improving your oral hygiene at home.
When gum disease progresses to periodontitis, the standard treatment is a professional deep cleaning, also known as scaling and root planing, to remove plaque, tartar, and infected tissue.
8. White lesions due to tobacco use
Smoking affects your mouth in many harmful ways. The heat, toxins, and carcinogenic chemicals in tobacco irritate the oral lining, which can cause ulcers, white patches, and other changes — including oral cancer.Smokers are 10 times more likely to develop oral cancer than people who have never smoked.
Smoking is also a major risk factor for gum disease. Studies show that over half of advanced gum disease cases are linked to tobacco use.
Smokers, compared to non-smokers, are:
- Six times more likely to develop gum disease
- More likely to have deeper periodontal pockets around their teeth
- Prone to greater gum recession
- At higher risk of bone loss
- More likely to lose their teeth
- Less likely to show gum bleeding, which can hide early signs of gum disease
Takeaway
White lines or spots on your gums can have many causes — some are harmless and temporary, while others may be more serious.
Because it’s often hard to tell just by looking, any white lines or patches that last more than two weeks or start getting bigger should be checked by your dentist or doctor.
If they are suspicious, a biopsy may be needed to get an accurate diagnosis.
- The gingival Stillman's clefts: histopathology and cellular characteristics. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4755679/
- Cho, Y.-D.; Kim, K.-H.; Lee, Y.-M.; Ku, Y.; Seol, Y.-J. Periodontal Wound Healing and Tissue Regeneration: A Narrative Review. Pharmaceuticals 2021, 14, 456. https://doi.org/10.3390/ph14050456
- Oral Changes Associated with Tobacco Use. https://maaom.memberclicks.net/
- A Color Handbook of Oral Medicine De Richard C. K. Jordan, Michael A. O. Lewis