How Can Various Dental Infections and Abscesses Affect You?
Dental infections occur when bacteria manage to penetrate deeper into your tooth or the surrounding tissues, such as the gums and bone.
The most common causes are cavities, gum disease, and cracks or fractures in the tooth’s hard outer layers.
An infected or abscessed tooth is often linked to that sharp, throbbing pain — but not always. In the chronic forms, when the infection develops slowly, you might not notice any obvious symptoms at all.
Keep reading to learn more about the different types of dental infections, how they can affect your teeth and overall health, how to recognize them, and the best ways to treat and prevent them.
In This Article....
1. What Does an Infected Tooth Mean?
2. How Can I Tell If I Have a Tooth Infection?
3. Types of Dental Infections
4. Who Is Most at Risk for Dental Infections?
5. How Does the Dentist Diagnose a Tooth Infection?
6. How Are Dental Infections Treated?
7. Healing from a Dental Abscess
8. How Can a Tooth Infection Spread if Left Untreated?
9. How to Prevent Tooth Infections
What Does an Infected Tooth Mean?
A tooth infection occurs when harmful bacteria win out over your body’s natural defenses.Normally, your teeth are protected by strong outer layers called enamel and dentin. When these layers break down, often due to cavities, they create an open door for bacteria to reach the pulp, the soft inner tissue containing nerves and blood vessels.
Once bacteria reach the pulp, they can spread beyond the tooth into the surrounding bone and gum tissue. This can lead to a buildup of pus, forming an abscess (also known as a gum boil or pimple on the gum).
However, cavities aren’t the only cause. In cases of gum disease, harmful bacteria can also penetrate deep beneath the gum line. When they infect the supporting tissues — like the bone and ligaments that hold your teeth in place — they cause severe inflammation and can also lead to abscess formation.
How Can I Tell If I Have a Tooth Infection?
Dental infections are known for their severe pain, making it hard to bite, chew, or even open your mouth comfortably.
However, pain usually appears only during the acute phase — when bacteria are actively spreading and damaging your tissues.
However, pain usually appears only during the acute phase — when bacteria are actively spreading and damaging your tissues.
In chronic infections, your immune system keeps the bacteria in check and prevents them from thriving. Because it's progressing slowly and silently, you might not notice any symptoms at all.
So, how can you tell if you have a chronic dental infection?
The truth is, you can’t without a professional dental check-up. Your dentist may need to take an X-ray, which is the only reliable way to spot hidden, symptom-free infections.
So, how can you tell if you have a chronic dental infection?
The truth is, you can’t without a professional dental check-up. Your dentist may need to take an X-ray, which is the only reliable way to spot hidden, symptom-free infections.
In the X-rays below, you can notice a dark shadow near the root tip. This indicates a buildup of pus, confirming the presence of a dental abscess.
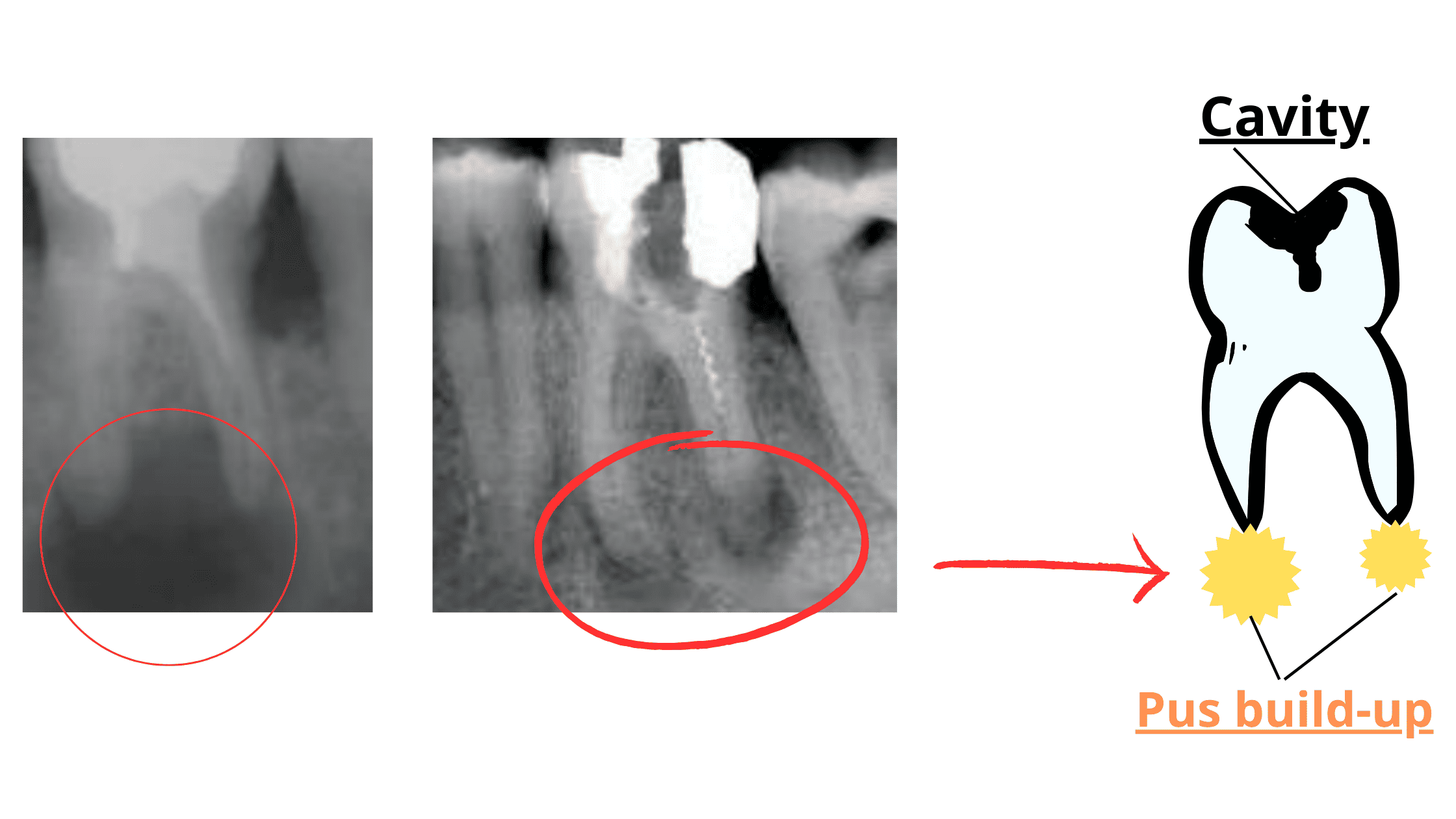
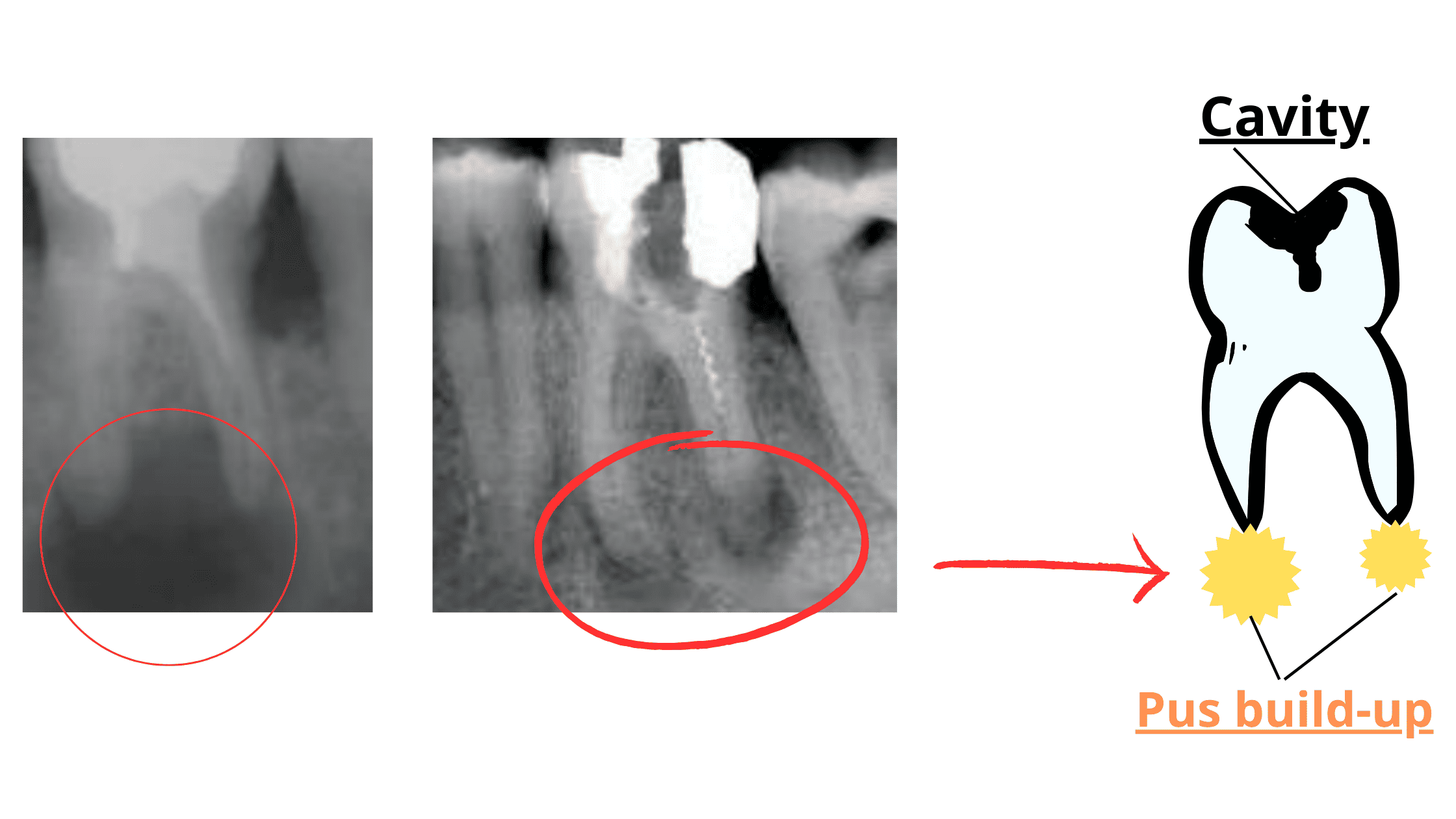
Ideally, you should visit your dentist twice a year (every six months) for routine check-ups to catch issues early.
When an infection flares up and produces symptoms, you might notice the following:
- Throbbing or constant toothache that doesn’t improve with painkillers
- Swelling, redness, or pus around the affected tooth or gum
- A bad taste or foul smell in your mouth
- Trouble chewing, swallowing, or opening your mouth
- Fever, headache, or nausea
Never ignore these signs. A tooth infection will never heal on its own. Without treatment, it can only spread further and become more serious over time.
Types of Dental Infections
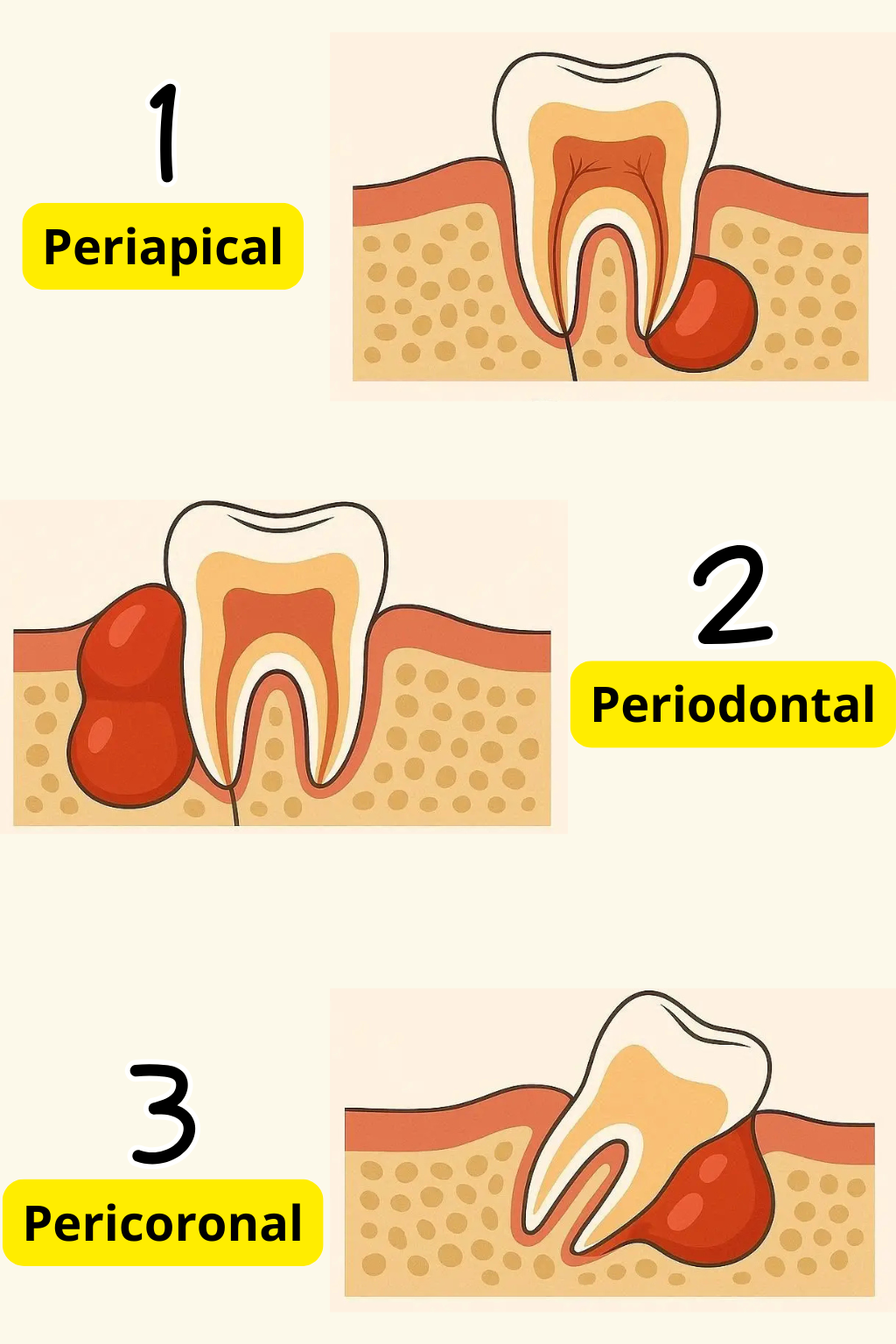
There are different types of tooth infections, based on where and how they developed.1. Periapical abscess:
A periapical abscess is often the first stage before bacteria spread further into the bone, gums, and surrounding facial tissues.
Other possible causes include cracked or broken teeth and failed dental treatments, especially root canals.

2. Periodontal abscess:
The toxins released, along with the intense inflammation, lead to a pocket of pus forming along the sides of the roots. It often appears as a localized swelling on the gums near the gum line (as shown below).


Periodontal abscesses are more common in people with poor oral hygiene, diabetes, or other medical conditions that compromise the immune defense.
3. Gingival abscess:

4. Pericoronal abscess:
Sometimes, the problem resolves on its own once the tooth fully erupts and aligns properly. However, if there isn’t enough space for the tooth to come in, the infection may keep returning and can spread or worsen over time.

Who Is Most at Risk for Dental Infections?
Healthy teeth and gums depend on a delicate balance between oral bacteria and your immune system. When that balance shifts towards harmful bacteria, dental infections can result.Several risk factors can cause the bad bacteria to overpower your immune defense, including:
1. Untreated Cavities
Nearly 90% of adults aged 20 to 64 have experienced tooth decay.
Cavities create tiny holes in the teeth that trap food particles, plaque, and more bacteria. As the decay progresses deeper, it can expose the tooth’s inner layers and nerves, leading to infection.
Once a cavity forms, the damage is irreversible, meaning it won’t heal on its own. The longer you wait, the more serious the damage and the higher your risk of infection.
2. Injury or Trauma
A chip, crack, or fracture in a tooth gives bacteria a direct path to the pulp, where they can multiply and cause an infection.
3. Failed Dental Work
Having a filling, crown, or root canal doesn’t make your tooth immune to problems. Without proper care and regular dental check-ups, restorations can wear down or develop new cavities underneath, leaving your tooth more vulnerable.
4. Poor Oral Hygiene
Not brushing properly and skipping flossing and professional cleanings allows plaque and tartar to build up. Tartar is the hardened form of plaque, which is extremely sticky and difficult, if not impossible, to remove at home.
5. Smoking
Smoking weakens your immune system and reduces blood flow to your gums, making it harder for your body to fight off harmful bacteria. It also increases the risk of many other oral conditions, like dry mouth, bad breath, gum disease, and oral cancer.
6. Weakened Immune System
Certain medical conditions — such as diabetes, HIV, or cancer — can compromise the immune system, making the body more vulnerable to dental infections, cavities, and gum disease.
7. Improper Use of Antibiotics
Misusing antibiotics can lead to antibiotic resistance, which simply means that some bacteria become stronger and harder to kill. This can turn a mild and easily treatable infection into a serious and potentially life-threatening condition.
How Does the Dentist Diagnose a Tooth Infection?
To diagnose a tooth infection, your dentist will perform several clinical tests and may use dental X-rays to reveal what's hidden inside the tooth.Here are the most common methods:
- Tapping or pressing on the tooth:
Your dentist may gently tap or press on the tooth to see if it causes pain. If it does, it’s a sign that the tissues around the tooth are inflamed or infected. - Palpating the gums:
This will help check for any swelling or pus buildup. If pus is present or leaking from the gum line, it's a strong sign of an active infection. - Thermal (hot and cold) tests:
Exposing the tooth to hot or cold stimuli will help assess whether the tooth is alive or not.
If the tooth is sensitive, it means the nerve is still alive.
If there’s no response, the nerve may be dead, and a root canal treatment could be necessary. - Dental X-rays:
X-rays help your dentist examine the inside of the tooth and the deep tissues that aren’t visible (such as the bone). They can reveal hidden decay, show the extent of infection, detect bone loss, and identify chronic or symptom-free infections.
How Are Dental Infections Treated?
The treatment for a tooth infection depends on its type and severity. Common approaches include:Incision and Drainage:
For certain abscesses, your dentist may make a small cut to drain the pus, which often provides immediate relief from pain and pressure. This drainage is typically followed by either a root canal or tooth extraction, depending on what's left of the tooth.
Root Canal Treatment:
If the tooth’s nerve is infected, a root canal is needed. During this procedure, your dentist removes the decayed tissues and cleans the canals inside the tooth. The canals are then shaped, disinfected, and filled. After healing, the tooth can be restored with a filling or a crown.
Extraction:
If the tooth is too damaged to save, removal may be the only option. This is usually the last resort when other treatments are less likely to be successful.
Antibiotics:
Not every dental infection requires antibiotics. Mild and localized infections are often resolved through surgical treatment alone. Your dentist will prescribe antibiotics only if your immune system is weakened due to a medical condition or if the infection has spread to surrounding tissues or other facial areas.
Healing from a Dental Abscess
After treatment for a dental abscess, here’s what you can expect:- Mild pain: It’s normal to experience some discomfort during the first few days. Pain usually peaks on the first day and gradually subsides, and can typically be managed with over-the-counter painkillers.
- Swelling: Some swelling around the treated area is common.
- Bruising and bleeding: These are temporary and usually resolve on their own.
What's the healing time?
The gums generally recover quickly within the first week. Bone and deeper tissues, however, take longer to fully heal, usually several months.
The gums generally recover quickly within the first week. Bone and deeper tissues, however, take longer to fully heal, usually several months.
When to worry about persistent pain?
Most pain should improve by the end of the first week. Contact your dentist if the pain is worsening instead of improving, or if new pain suddenly appears days later. This can indicate that the infection was not fully cleared or has returned.
Most pain should improve by the end of the first week. Contact your dentist if the pain is worsening instead of improving, or if new pain suddenly appears days later. This can indicate that the infection was not fully cleared or has returned.
Tips to support recovery:
- Take all medications as prescribed, and complete the full course.
- Apply cold compresses to the treated area for 10–20 minutes at a time, several times a day, during the first 24 hours.
- Avoid strenuous activity on the first day to prevent bleeding.
- Avoid smoking or tobacco products for at least a few days.
- Start with soft foods, gradually returning to a normal diet as your mouth heals.
- Rinse your mouth with warm salt water, starting from the second day.
- Brush and floss gently as usual, but avoid touching or injuring the treated area.
- Keep all follow-up appointments with your dentist to monitor healing closely.
How Can a Tooth Infection Spread if Left Untreated?
A tooth infection should never be ignored or delayed. Without treatment, it won’t heal on its own and can spread to the face, jaw, throat, and neck. The longer you wait, the more serious it becomes, and the more complicated and costly the treatment may be.In severe cases, bacteria can even enter the bloodstream, affecting other organs and causing life-threatening complications.
Some potential complications include:
1. Bone Infection (Osteomyelitis)
Bacteria can move from the tooth into the underlying jawbone, causing swelling, pain, and tooth loss. If left untreated, significant portions of the jawbone can be destroyed, leading to facial deformities and noticeable changes.
2. Facial Cellulitis
The infection can spread to the soft tissues of the face, including the cheeks, chin, and under the eyes. Symptoms include redness, warmth, diffuse swelling, and pain. Areas such as the throat, neck, and under the jaw are considered “danger zones” because if a dental infection spreads there, it can block the airways, causing difficulty breathing or even choking.
3. Sinusitis
The upper back teeth are located just below the sinuses. If an infection spreads upward, it can cause a sinus infection (sinusitis). Symptoms include severe pain and pressure around the cheeks and eyes, headaches, and nasal congestion.
4. Sepsis
Sepsis occurs when bacteria from the infection enter the bloodstream, triggering a severe immune response. This can lead to a dangerous drop in blood pressure, organ failure, and, if untreated, death.
5. Endocarditis
This is when bacteria spread to the heart, causing inflammation of the heart lining and valves. This is a life-threatening complication that requires urgent medical care.
6. Brain Abscess
Although rare, a tooth infection can spread to the brain, forming a pocket of pus (brain abscess). This is possible because the venous network of the mouth and face connects directly to the brain. People with weakened immune systems are at higher risk for this severe complication.
How to Prevent Tooth Infections
The best way to deal with dental infections is to prevent them from happening in the first place.Maintaining a consistent oral hygiene routine and taking a few simple steps is all it takes to keep harmful bacteria in check and protect your teeth and gums, as well as your oral and overall health.
Here are some tips:
- Brush at least twice a day: Use fluoride toothpaste to remove plaque, the main culprit behind cavities and gum disease.
- Floss daily: To remove food particles and plaque from between your teeth and just under the gum line. The best time to floss is before bed. You can also use other interdental cleaning tools, like water flossers or interdental brushes, if you prefer.
- Limit sugar intake: Sugar feeds the bacteria that cause cavities. Not only will reducing sugar protect your teeth, but your overall health will thank you too.
- Visit your dentist regularly: Routine check-ups and cleanings help your dentist detect and treat early signs of decay or gum disease before they advance and become serious.
- Reduce, or even better, quit smoking altogether: Smoking takes a serious toll on your teeth and gums. Smoking also makes dental treatments less effective and less successful. Quitting may be challenging at first, but it’s a step that pays off for your oral and overall health in the long run.
- Periodontal Abscess https://www.ncbi.nlm.nih.gov/books/NBK560625/
- Dental Abscess https://www.ncbi.nlm.nih.gov/books/NBK493149/
- Textbook of General and Oral Surgery
- Bilateral Maxillary and Mandibular Periapical Abscesses https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9038579/
- Dental abscess - Antibiotic use in dental infections https://www.mayoclinic.org/diseases-conditions/tooth-abscess/diagnosis-treatment/