Here’s How a Tooth Infection Can Affect Your Heart
 It all begins with a small cavity. If left untreated, the decay deepens, eventually reaching the dental pulp, where the tooth's blood vessels and nerves are housed.
It all begins with a small cavity. If left untreated, the decay deepens, eventually reaching the dental pulp, where the tooth's blood vessels and nerves are housed.
What many don't realize is that these blood vessels are connected to the rest of the body. In severe cases, a tooth infection can spread throughout the body, reaching vital organs like the brain, lungs, and heart.
Keep reading to discover how a tooth infection can lead to three serious cardiovascular complications.
1. Tooth Infection & Atherosclerosis
What is atherosclerosis?
This occurs when the inner lining of blood vessels thickens over time due to the buildup of low-quality fats, or bad cholesterol. This buildup forms plaque, known as atheroma, inside the vessels. As a result, blood flow becomes restricted, potentially leading to serious complications.
How does tooth infection occur?
The starting point of most dental infections is tooth decay. As the decay progresses deeper and reaches the pulp, the tooth, while still alive, tries to contain the infection and prevent it from spreading.
However, once the pulp dies (a condition called pulpal necrosis), the infection travels down the root canals to the area around the root tip, known as the periapical area. This condition is called apical periodontitis.
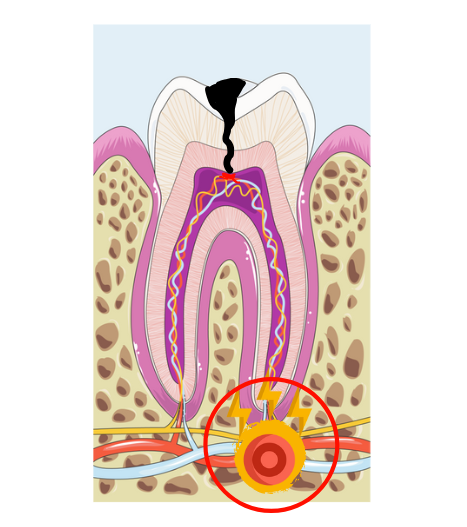
What makes apical periodontitis tricky is that it's often chronic and asymptomatic, meaning you can have it without feeling any symptoms. This is why regular dental check-ups are crucial—only an X-ray can detect these hidden lesions. Sometimes, apical periodontitis flares up, leading to a tooth abscess with symptoms such as:
- Intense pain that spreads to the jaw, joints, and ears
- Sensitivity to hot foods
- A "long tooth" sensation
- Bad breath or taste
- Swelling or an abscess near the root tip
- Swelling in the cheeks or beneath the jaw
- Fever
How Can a Dental Infection Contribute to Atherosclerosis?
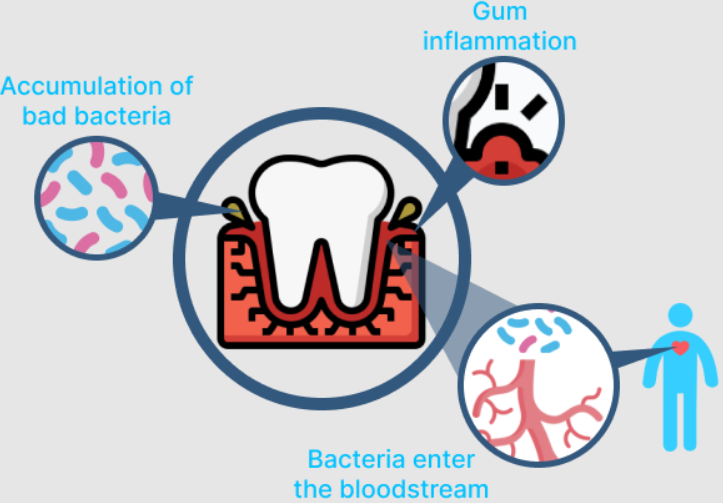
Two bacteria commonly associated with gum and tooth infections, Actinobacillus actinomycetemcomitans (Aa) and Porphyromonas gingivalis (Pg), have been detected in atherosclerotic lesions.
But to understand this link, you have to understand how atherosclerosis develops.
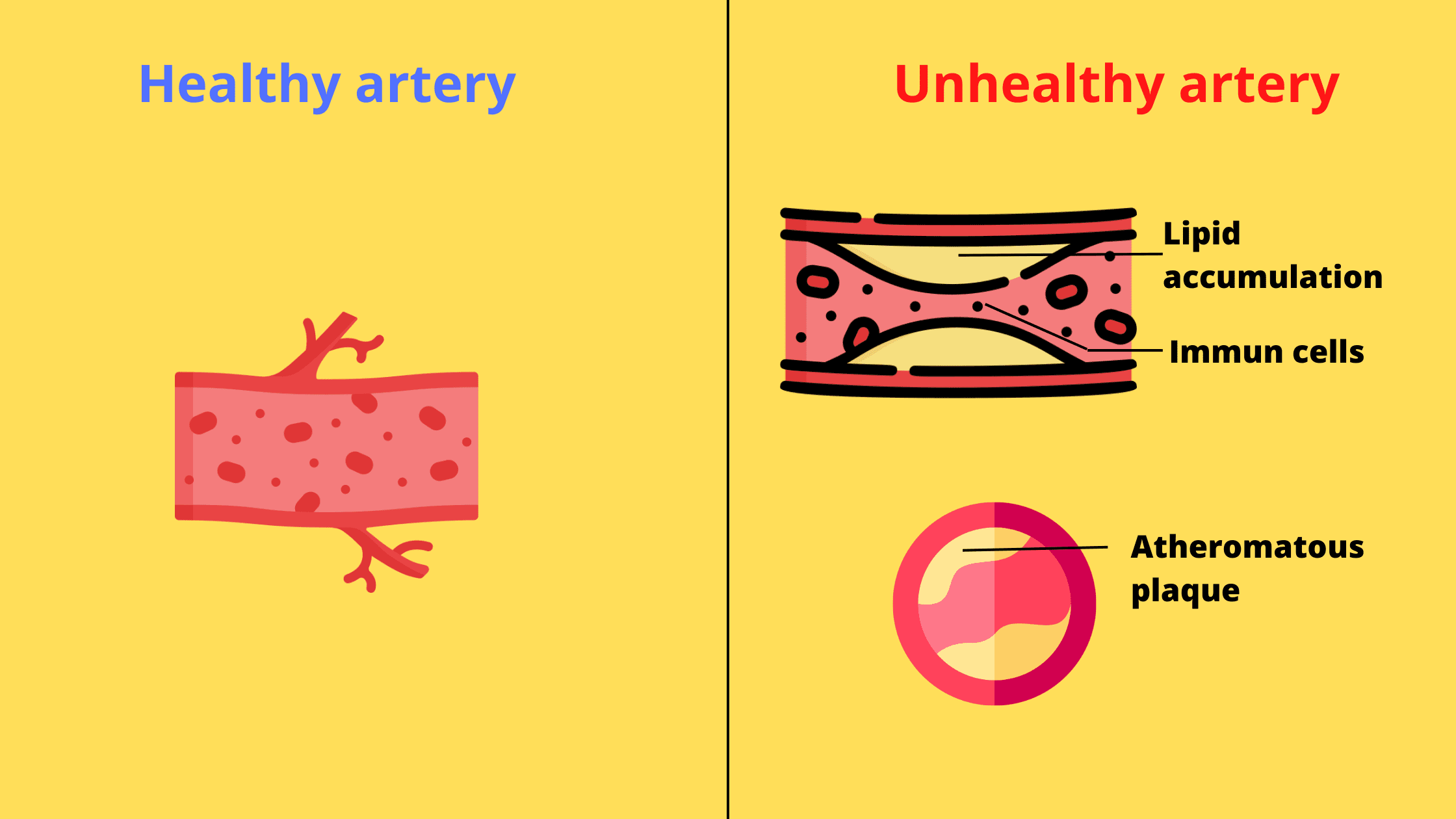
Atherosclerosis develops when bad cholesterol, primarily from high-fat diets, builds up in the inner lining of blood vessels, forming a thick mass known as an atheroma plaque.
As the fatty buildup oxidizes over time, it triggers inflammation, attracting immune cells to the area in an attempt to eliminate the plaque. However, as these cells absorb the cholesterol, they bulk up. Eventually, these cells die and further clog the arteries.
Even worse, over time, the plaque can break down and rupture, activating the blood clotting process. This can block blood flow, leading to life-threatening complications.
So, how can a tooth infection lead to atherosclerosis?
Remember that atherosclerosis is primarily driven by inflammation.
While the body does a good job at containing infections and preventing their spread, inflammation doesn’t work the same way. The inflammatory response triggered by a tooth infection can leave its mark on the entire body!
So, by increasing inflammation, a tooth infection can accelerate the progression of atherosclerosis. This means it can increase the risk of existing arterial plaques thickening or rupturing, which can have serious complications. For example, if the coronary artery is affected, it may result in heart problems; if the carotid artery is involved, it can cause brain damage.

Furthermore, bacteria from a tooth or gum infection can enter the bloodstream and settle directly in existing atheroma plaques. This can trigger additional inflammation and further accelerate the progression of atherosclerosis.
In summary, while inflammation is meant to protect the body, chronic tooth infections can cause undesirable persistent inflammation with harmful effects, including:
- Accelerating atherosclerosis, which can lead to severe consequences like stroke (if the carotid artery is affected) or heart attack (if the coronary artery is involved).
- Increasing oxidative stress throughout the body.
- Reducing the antioxidant properties of HDL (good cholesterol).
- Contributing to high blood pressure.
2. Tooth Infection & Coronary Artery Disease
What is coronary artery disease?
Coronary artery disease (CAD) refers to a condition in which the coronary arteries, which supply blood to the heart, become narrowed or blocked by a buildup of plaque.
The mechanism is similar to that of atherosclerosis. Increased inflammatory molecules in the blood can affect the coronary arteries, promoting further plaque buildup and narrowing of the arteries. This results in reduced blood supply to the heart.
Symptoms of Coronary Artery Disease include chest pain, shortness of breath, and fatigue. If left untreated, the condition can progress to more serious complications, such as heart attack and heart failure.
3. Tooth Infection & Infectious Endocarditis
What is infectious endocarditis?
It's an infection affecting the heart valves, a kind of gate that prevents the blood pumped by the heart from changing direction.
It results from bacteria that enter the body through a lesion, circulate in the bloodstream, and eventually attach to the heart.
Infective endocarditis occurs when a damaged or injured heart valve traps bacteria that have entered the bloodstream. This complication mainly affects people with weakened hearts or those already suffering from heart problems. For these individuals, any mouth injury or infection can allow bacteria to enter the bloodstream and attach to the heart.
Bacteria can even enter the bloodstream during simple daily activities such as brushing teeth or chewing hard foods.
However, for most healthy individuals, this is temporary, as the body quickly eliminates the invaders.
However, in people at risk, the bacteria can adhere to a heart valve and form a bacterial plaque. This can lead to ulceration or even perforation of the affected valve, resulting in life-threatening heart dysfunction.
Signs That May Indicate a Risk of Heart Complications
As mentioned earlier, most of the time a tooth infection will stay contained where it started, as long as the immune system functions properly and there are no risk factors. In such cases, symptoms are limited to the area around the tooth and may include swelling, redness, pain, and pus buildup.However, there are signs that the infection may be taking a more serious turn and spreading beyond the tooth. These symptoms may affect parts of the body far from the involved site and can include:
- Fever, fatigue, and dehydration: These typically occur when the infection has spread, triggering an intense inflammatory reaction. They may also indicate a life-threatening condition known as sepsis, which is a severe response by the body that can lead to a dramatic drop in blood pressure and organ failure.
- Increased heart and breathing rate: If a tooth infection causes noticeable changes in your heart or breathing rate, this indicates the body is fully engaged in fighting the infection. They can also be the early signs of sepsis.
If you experience any of these symptoms, seek emergency dental care immediately to prevent serious complications. - Swelling: A common sign of dental infection is localized swelling, known as a gum boil or dental abscess. Sometimes, the swelling can spread to surrounding tissues like the cheeks and chin, leading to facial cellulitis.
In severe cases, this can extend to the area below the jaw, potentially blocking the upper airways and making breathing difficult, which can be life-threatening.
Risk factors for heart complications
Heart complications from dental infection are rare, but certain factors increase the risk drastically. Some of them include:- Weakened immune system due to diabetes, HIV infection, chemotherapy or radiotherapy, or blood disorders.
- Wearing a heart valve prosthesis
- History of endocarditis
- Unoperated congenital heart disease
- Stress
- Smoking
- High cholesterol levels.
- High blood pressure
- Overweight
How to prevent heart complications
The best way to prevent cavities and gum disease, therefore, potential heart complications, is to practice good oral hygiene.Cleaning your mouth regularly and properly will help reduce plaque build-up and bacterial load, which can help prevent dental infections and possible heart damage. Oral hygiene measures include:
- Brush your teeth twice a day and clean between your teeth with dental floss or interdental brushes daily. This will help you remove bacterial plaque, the leading cause of cavities and gum disease.
- Eat a healthy diet that includes essential nutrients for your oral and heart health. These include vitamin C, vitamin D, essential fatty acids, iron, and other minerals.
- Quit smoking and reduce your alcohol consumption to reduce your risk of both oral and cardiovascular diseases.
- Schedule regular check-ups and professional dental cleanings with your dentist to remove tartar buildup and detect any dental infections early on.
- If you have heart disease, make sure to inform your dentist and provide them with a list of your medications and contact information for your cardiologist. This will help them take the necessary steps to avoid any complications.
- Association between chronic apical periodontitis and coronary artery disease https://pubmed.ncbi.nlm.nih.gov/24461397/
- Apical periodontitis and atherosclerosis: Is there a link? Review of the literature and potential mechanism of linkage https://pubmed.ncbi.nlm.nih.gov/28462408/
- The connection between C-reactive protein and atherosclerosis https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3364506/
- Periodontal Disease-Induced Atherosclerosis and Oxidative Stress https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4665422/
- Heart Valves and Infective Endocarditis https://www.heart.org/en/health-topics/heart-valve-problems-and-disease/heart-valve-problems-and-causes/heart-valves-and-infective-endocarditis
- What Is Sepsis? Symptoms and Treatment https://share.upmc.com/2017/09/what-is-sepsis/