Why does my gum hurt years after wisdom tooth removal?
 After wisdom tooth removal, everything should be back to normal. Swelling and pain should gradually decrease, and your gums will return to their normal appearance within a few weeks.
After wisdom tooth removal, everything should be back to normal. Swelling and pain should gradually decrease, and your gums will return to their normal appearance within a few weeks.
If the pain persists longer than expected, talk to your dentist, as this may be a sign of a complication. Other times, it may be due to other conditions unrelated to the procedure itself.
Pain that lasts for months or years, or that comes and goes periodically, is referred to as chronic, and we'll look at the reasons behind this.
In this article:
1. Potential causes of pain years after wisdom teeth removal
- Cavities or infections of neighboring teeth
- Gum disease
- Something may be stuck in your gum
- Muscle and joint pain
- A nerve may have been damaged during the procedure
- Jaw cyst
- Atypical odontalgia
2. Takeaway
Potential causes of pain years after wisdom teeth removal
You feel pain in your mouth when specific nerve endings—called nociceptors—are triggered. This usually happens due to injuries or inflammation caused by dental issues like cavities, gum disease, or infections.
But pain isn’t always caused by visible damage or active inflammation. Sometimes, it can happen without obvious cause. That's the case with neurogenic and psychogenic pain:
- Neurogenic pain: Caused by damage or dysfunction in the nerves that transmit sensations.
- Psychogenic pain: Linked to psychological factors like anxiety, stress, or depression.
Pain that lasts or suddenly appears years after a wisdom tooth extraction can have different meanings.
It is not necessarily related to the extraction procedure. Certain dental conditions such as gum disease, apical periodontitis, and pulpitis affecting nearby teeth can cause pain to spread throughout the face and jaws, including the extraction site.
Less commonly, a nerve that controls sensation may have been damaged during the procedure, resulting in a long-term tingling or burning sensation.
Here are 7 potential causes of pain years after wisdom teeth removal:
1. Cavities or infections of neighboring teeth
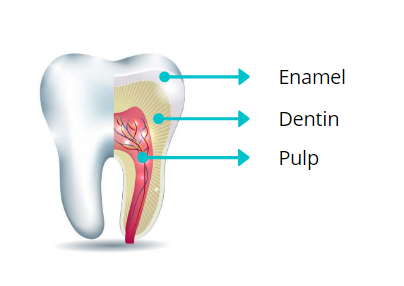 Cavities affect the hard tissues of the teeth, including the enamel (the outermost layer), and the underlying dentin. If left untreated, cavities will continue to progress toward the pulp where the nerves and blood vessels of the tooth are located.
Cavities affect the hard tissues of the teeth, including the enamel (the outermost layer), and the underlying dentin. If left untreated, cavities will continue to progress toward the pulp where the nerves and blood vessels of the tooth are located.
Once bacteria are inside the pulp, they grow and thrive, resulting in a painful infection. The pain can be so intense and throbbing that it can keep you awake at night.
The discomfort may extend to nearby teeth, jaws, temporomandibular joints, and even the ear, making it often difficult to pinpoint the exact source of the pain.
So the pain you feel in one area of your mouth may actually be arising from another tooth infection that needs prompt treatment.
2. Gum disease
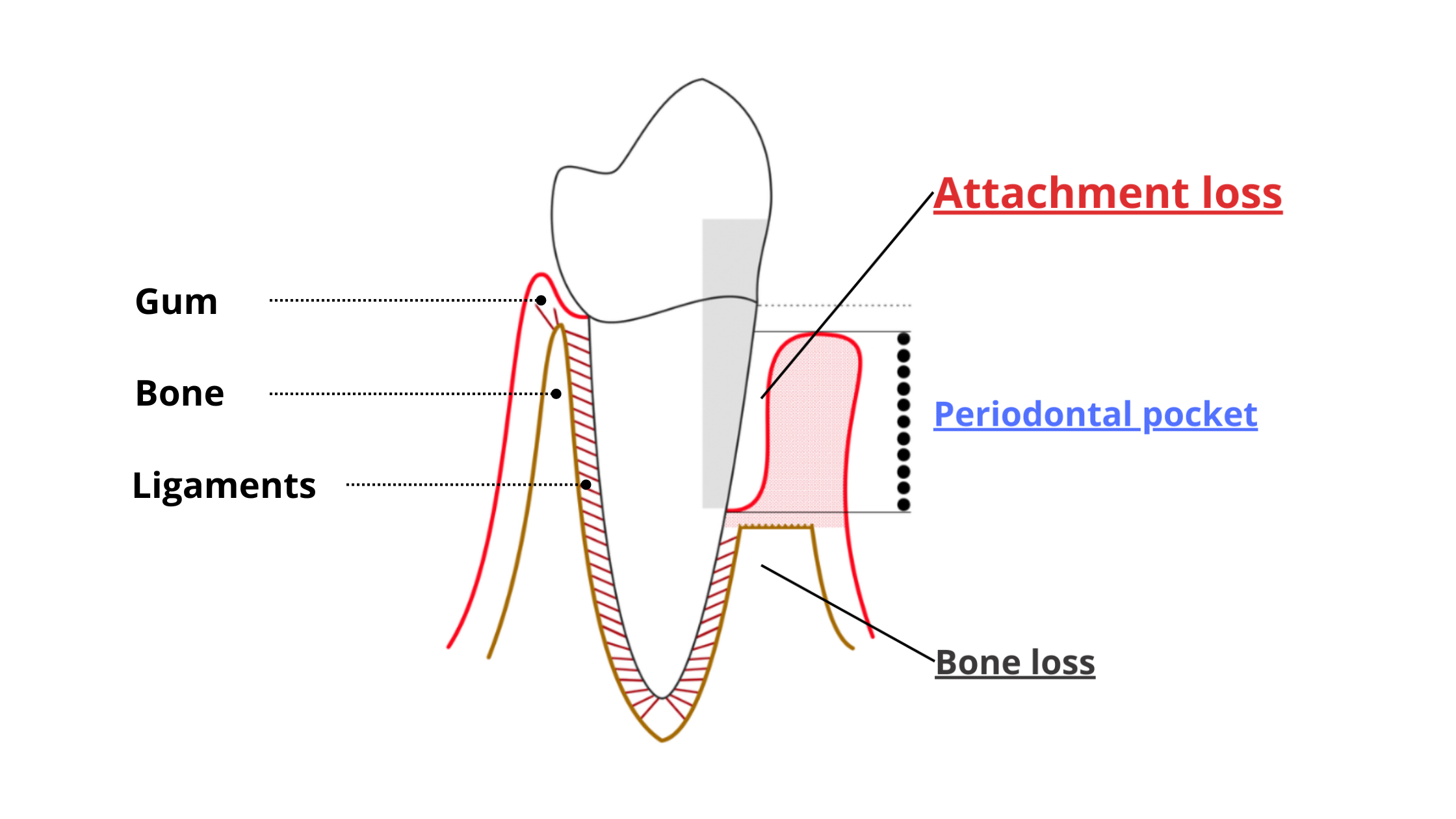 Gum disease includes conditions such as gingivitis and periodontitis, which are inflammatory conditions caused by some “bad” bacteria.
Gum disease includes conditions such as gingivitis and periodontitis, which are inflammatory conditions caused by some “bad” bacteria.
When plaque accumulates along your gum line, harmful bacteria grow and damage the tissues surrounding your teeth.
Teeth at the back of the mouth are the most vulnerable, as they are harder to reach and clean with a toothbrush. So, plaque is more likely to accumulate there.
As a result, the gums and bone that hold the teeth in place gradually break down and recede, causing sensitivity. At an advanced stage, tooth loss becomes a real threat.
Symptoms of gum disease include:
- Redness and swelling of the gums.
- Bleeding when you eat or brush your teeth.
- Gum and tooth sensitivity.
- Gum recession and tooth loosening.
- Pus discharge around the teeth.
- Bad breath.
- Teeth shifting leading to an improper bite.
Treatment for gum disease begins with addressing all underlying causes. This includes good oral hygiene (regular brushing and flossing) and professional dental cleaning to remove plaque and tartar, the main culprits behind gingivitis and periodontitis.
3. Something may be stuck in your gum
Pain and swelling in your gums can be caused by food debris or a foreign object stuck in them.Have you eaten anything crunchy or hard lately, like popcorn or chips? If so, it's possible that a piece got stuck in your gum and is causing the discomfort.
You may notice that your gums are red and swollen, and even some pus leaking along the gum line if the infection has already set in.
4. Muscle and joint pain
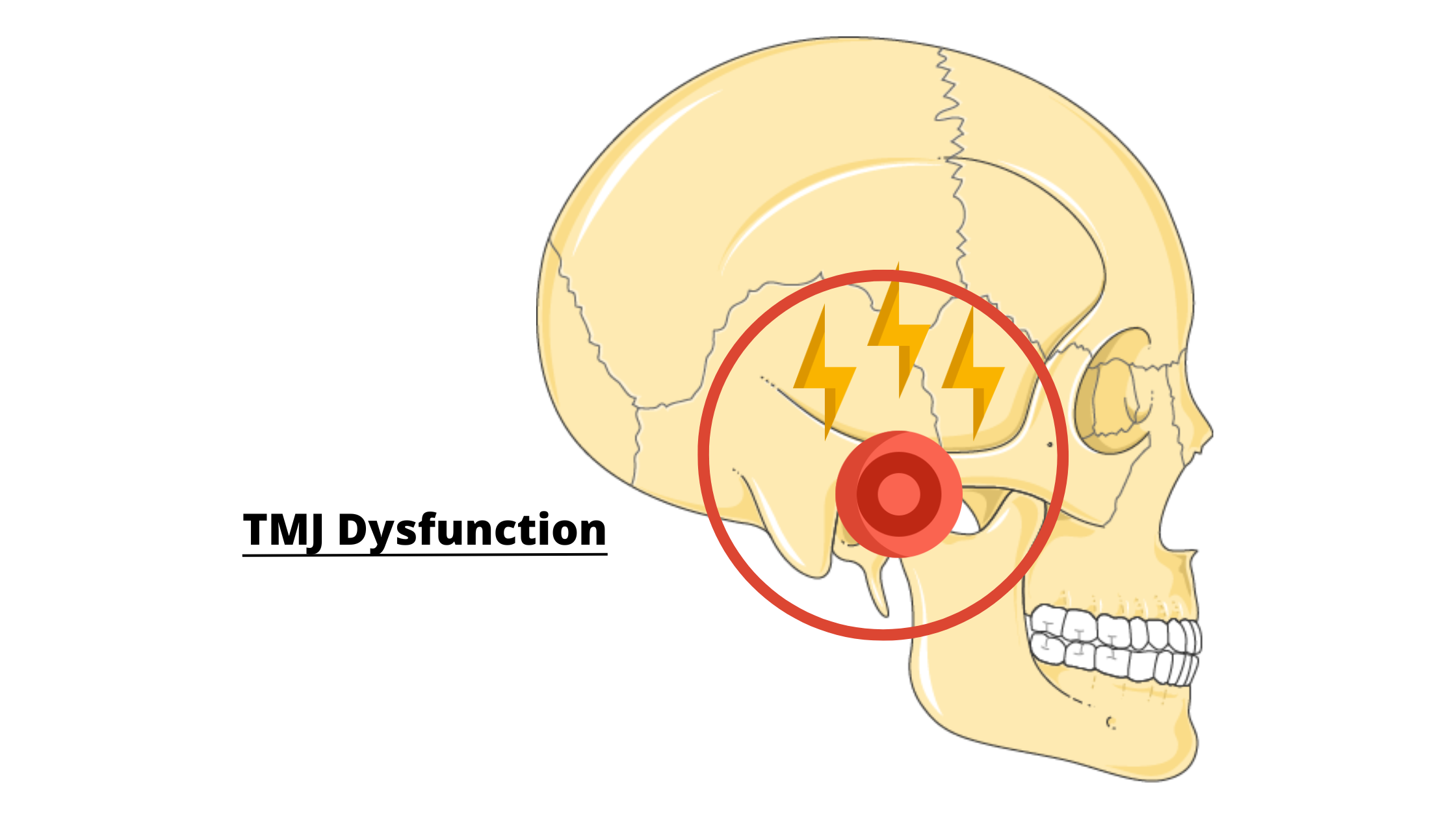 Temporomandibular joint disorders (TMDs) are one of the most common causes of facial and oral pain. These disorders affect the chewing muscles and joints that connect the lower jaw to the skull.
Temporomandibular joint disorders (TMDs) are one of the most common causes of facial and oral pain. These disorders affect the chewing muscles and joints that connect the lower jaw to the skull.
TMDs can cause pain to spread throughout the jaws and teeth. That's why patients often feel like they have tooth pain rather than muscle or joint problems.
Symptoms may include:
- Pain or tenderness in the jaw, face, neck or around the ears.
- Difficulty opening or closing the mouth.
- Increased pain when chewing.
- Clicking sound in your joints when you chew or open your mouth.
- Morning headaches, especially if you grind your teeth at night.
5. A nerve may have been damaged during the procedure
Nerve damage during wisdom tooth removal is uncommon. Even if it occurs, it's typically a temporary issue that resolves on its own within a few weeks or months.During the extraction procedure, there is a small risk that a nerve may be accidentally injured or, more seriously, severed.
This is more common with lower wisdom teeth than upper ones because they're often located close to large nerves that innervate most of the lower face and jaw, including the teeth, gums, chin, tongue, and lower cheeks.
Nerve injuries during the procedure may cause long-lasting tingling or numbness (paresthesia), pain and burning sensation (allodynia), or complete loss of sensation (anesthesia).
In most cases, these symptoms resolve within the first six months after surgery as the damaged nerve heals. However, if symptoms persist or show no improvement after 24 months, there is a strong chance that the damage is permanent.
6. Jaw cyst
Cysts are fluid-filled sacs that can develop anywhere in the body. They usually grow slowly and often don’t cause any symptoms for years—or even decades.Jaw cysts are relatively uncommon, but when they do appear, they’re most often linked to teeth. Impacted wisdom teeth (those that are trapped in the jawbone) are one of the most frequent causes of these cysts.
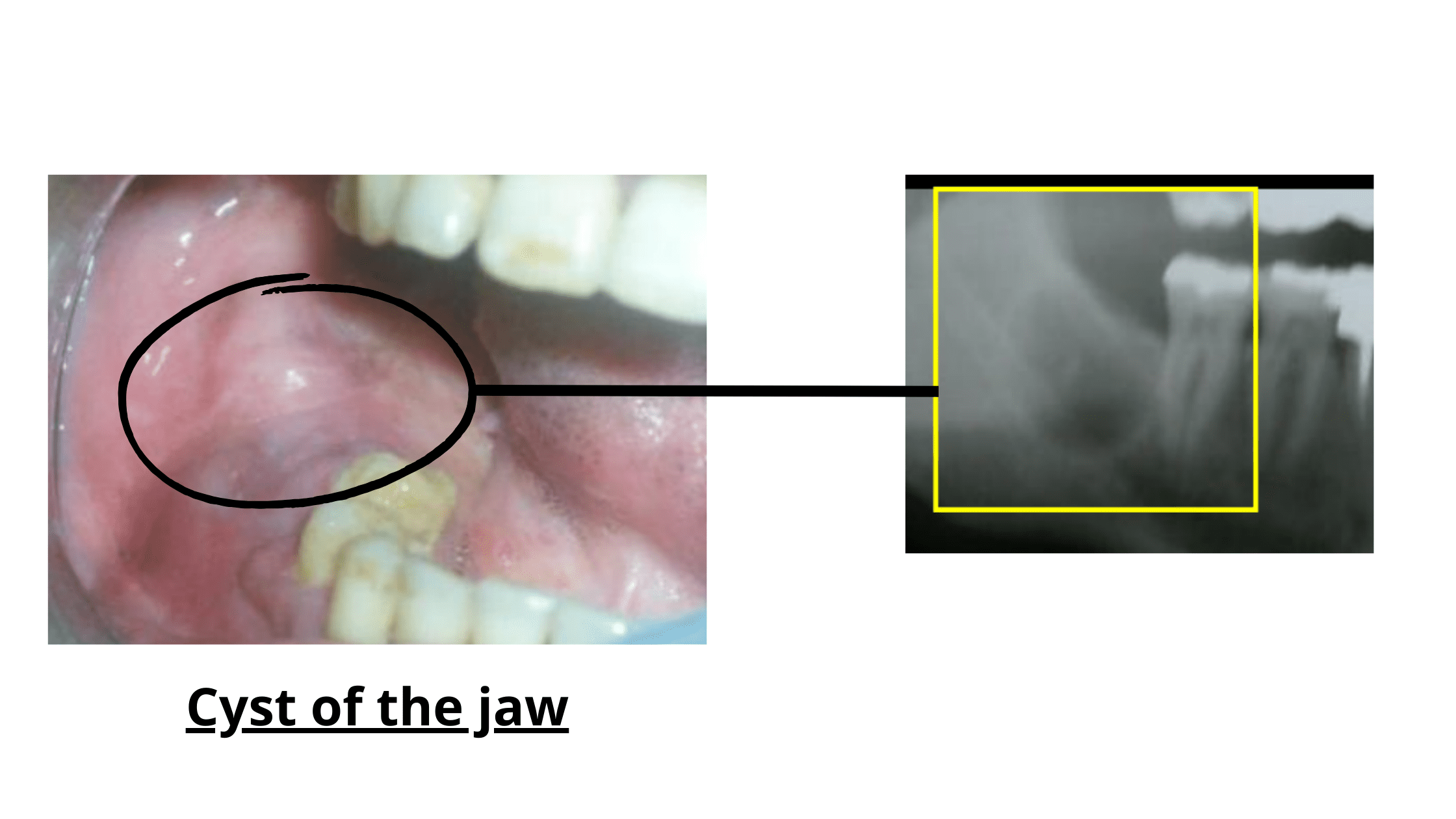
If a cyst was connected to your wisdom tooth and wasn't completely removed during extraction, it may still be there and continue to grow over time.
Most jaw cysts develop silently, without causing any symptoms. You may not notice anything until the cyst becomes large or infected, which can take years. When this happens, the gum may become red and swollen, and a pale fluid may drain from it.
As the cyst grows, it may also put pressure on your jaw or cause a dull, diffuse discomfort in the surrounding teeth.
7. Atypical odontalgia
Atypical odontalgia (AO), also known as phantom tooth pain, is a rare and mysterious dental condition with no clearly known cause. It affects between 0.03% and 1% of people, mostly women over the age of 40.AO is defined as ongoing pain in one or more teeth, or in areas where teeth were extracted, without any visible problem or identifiable reason.
In about 83% of cases, it starts after a dental procedure like a tooth extraction or root canal. The affected area often looks perfectly healthy, which can be confusing for both you and your dentist.
The pain is usually described as burning, aching, or throbbing. It doesn’t respond to regular painkillers, though in most cases, the discomfort stays mild and doesn’t interfere too much with your daily life.
The exact cause of AO is unclear, but many believe it's connected to nerve damage or dysfunction. Due to the confusion it causes, people with AO often undergo unnecessary dental treatment, which unfortunately can only make the pain worse.
Treatment focuses on relieving symptoms, particularly pain, with medications and therapies that slow down the processing of pain by the brain.
Takeaway
After having a wisdom tooth removed, it is normal to experience some swelling and pain. These should gradually subside within a few weeks.
However, if the pain persists longer than expected, or if it suddenly appears several years after the procedure, it may be a post-operative complication or an underlying dental or facial condition.
Any kind of mouth pain deserves to be checked by your dentist. Once the real cause is known, fixing the issue becomes much more straightforward.
- Advances in understanding nociception and neuropathic pain https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5808094/
- Residual cyst of the jaws: A clinico-pathologic study of this seemingly inconspicuous lesion https://pubmed.ncbi.nlm.nih.gov/33332452/
- Atypical odontalgia – pathophysiology and clinical management https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-2842.2007.01813.x