What causes blackness between my teeth? How can I get rid of it?
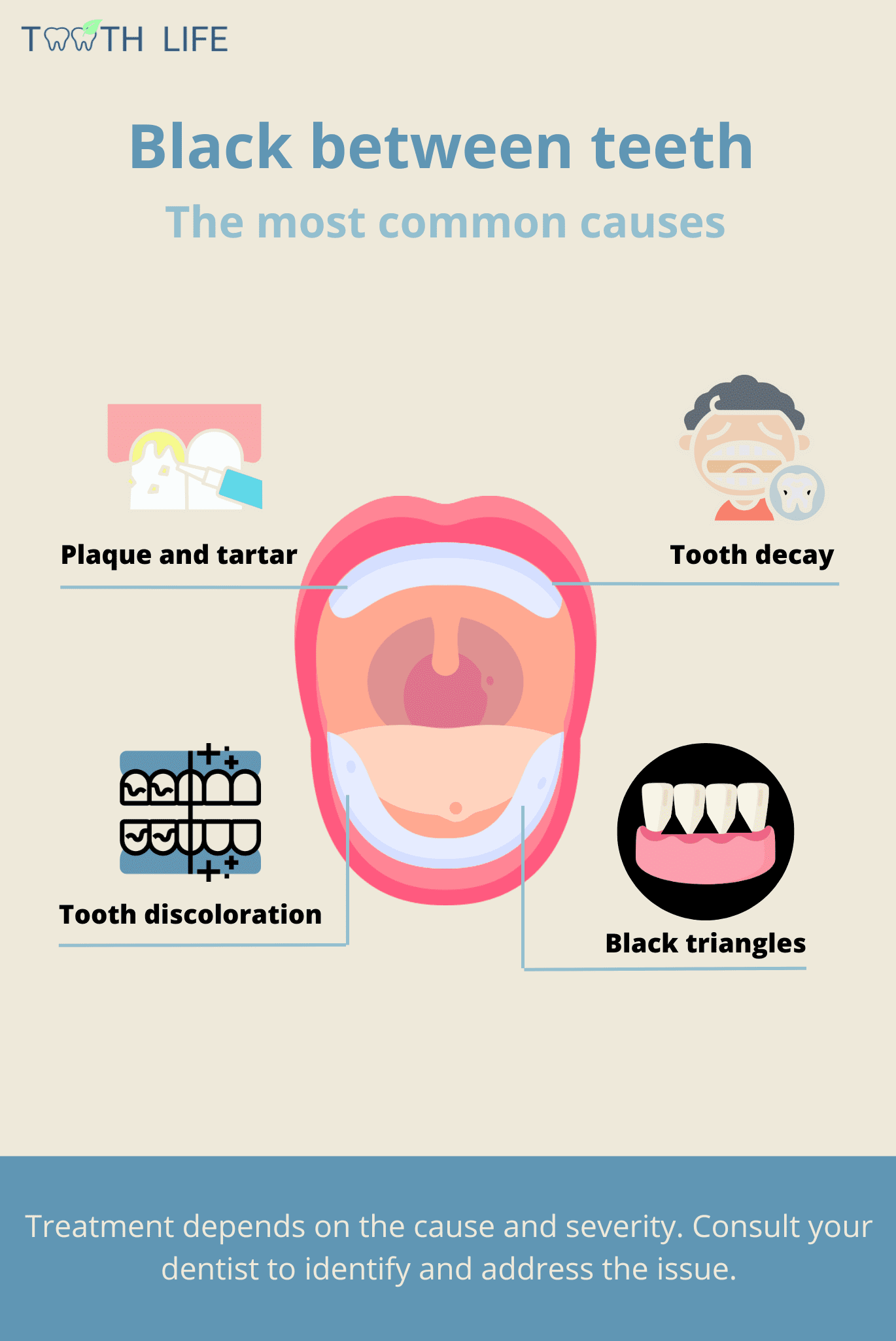 Noticing blackness, staining, or discoloration on your teeth—especially the front ones—can really affect the way your smile looks and your overall appearance.
Noticing blackness, staining, or discoloration on your teeth—especially the front ones—can really affect the way your smile looks and your overall appearance.
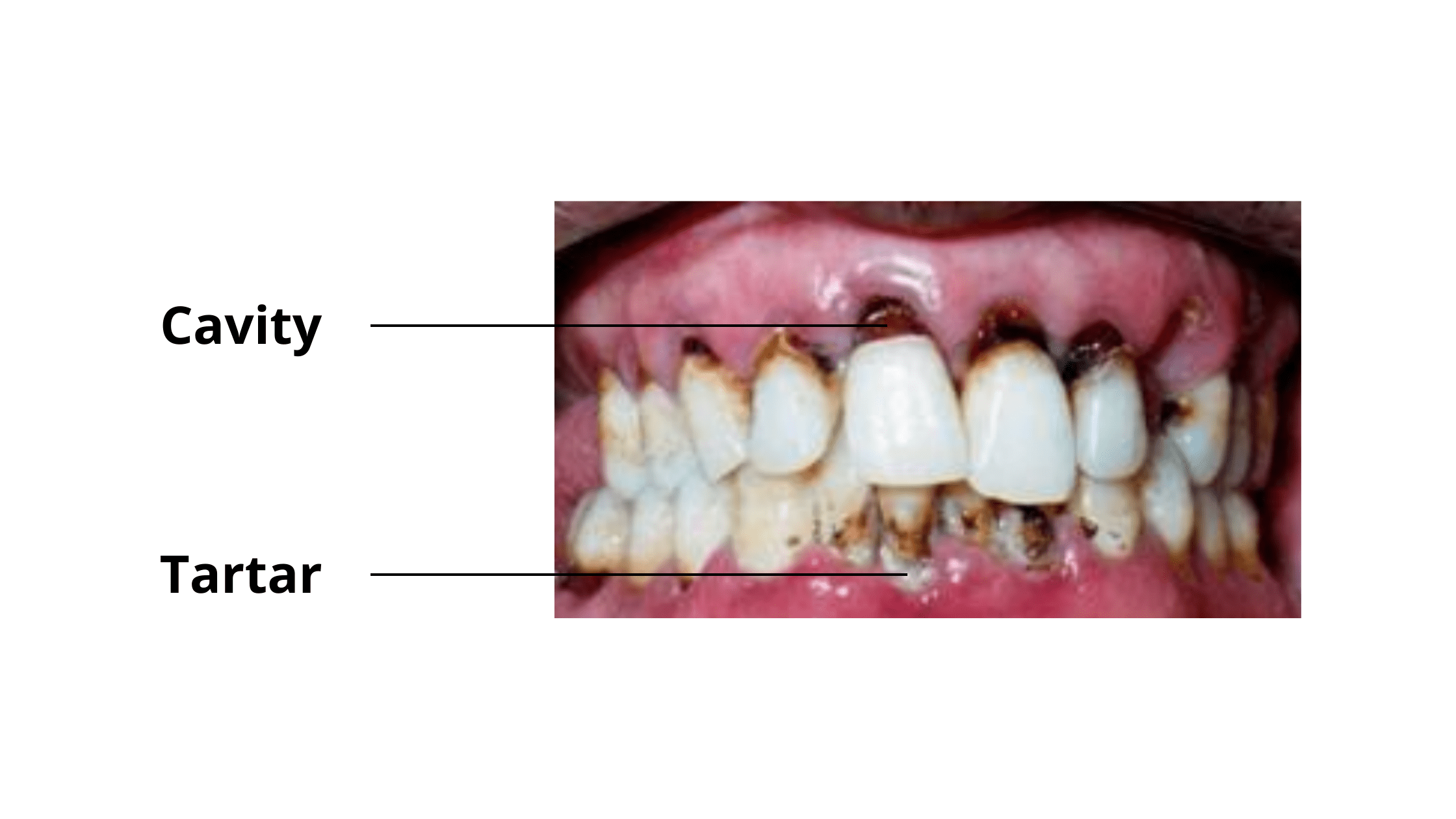
If you're dealing with black discoloration between your teeth, you're not alone. Several dental issues can cause this, such as black tartar, stains from certain foods, or even cavities.
As with most dental problems, the first step is identifying the root cause. Once you know what's behind it, finding a solution becomes much easier.
Keep reading to discover the common causes of blackness between teeth and practical tips to restore your smile to its best.
In this article:
1. Black Triangles
2. Tooth Discoloration or Dental Staining
3. Plaque & Tartar:
4. Tooth Decay:
Key takeaways:
Blackness between your teeth can result from several dental conditions, including:
- Black triangles: These are gaps or voids between the teeth that appear dark, hence the name. While they can be normal in certain cases, they may also indicate gum recession or other dental issues.
- Plaque and tartar buildup: When plaque and tartar accumulate on your teeth, they can absorb pigments from foods like coffee, tea, and chocolate, leading to dark, sticky deposits.
- Tooth discoloration or staining: Certain foods can cause pigments to penetrate the outer layer of your teeth, resulting in dark stains. These typically affect the enamel (the outermost layer), making them easier to remove.
- Cavities: Black discoloration may also signal tooth decay or cavities. If you feel a hole or a lesion in your tooth, it's likely a cavity.
Treatment Options
The treatment depends on the cause and severity of the issue:
- Tartar buildup? A professional dental cleaning will clear that up.
- Staining? You may need a whitening treatment to brighten your smile.
- Cavities? A dental filling by your dentist will be required to fix the problem.
1. Black Triangles
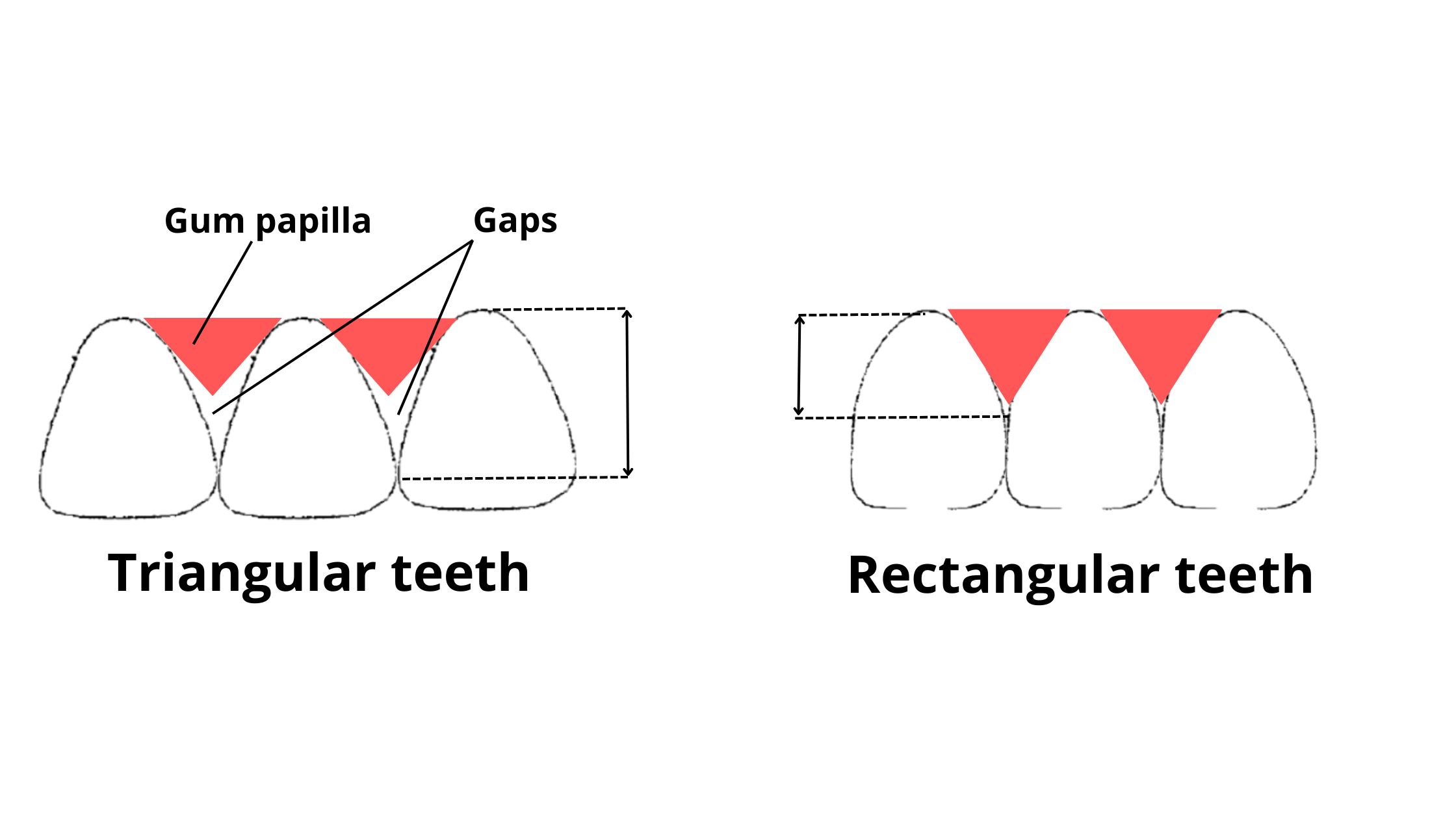
When your gums are healthy, they fit snugly around your teeth, creating small triangle-shaped areas between them called papilla or interdental gingiva.
However, if your gums start to recede, pulling away from the teeth, the papilla that usually fills the space between them can shrink or disappear. This leads to the formation of black gaps, known as "black triangles."
Black triangles can be normal if you’ve always had them, especially if you have round or triangular-shaped teeth. Some people are also genetically predisposed to having shorter or missing papilla.
But if you notice these black triangles suddenly appearing when you didn’t have them before, it could signal a dental issue that needs attention.
While black triangles don’t always require treatment, they can sometimes lead to problems like gum disease or cavities, especially if they trap more plaque and food particles.
Causes of Black Triangles
The most common causes of black triangles between teeth include: Gum Disease:
Plaque:
Plaque buildup is the main cause of gum disease. When oral hygiene is neglected, bacteria in plaque can penetrate the gum line, causing inflammation. As the inflammation progresses and affects the deeper tissues supporting the teeth, it can lead to bone loss, gum recession, and loose teeth. As the gums recede, black gaps may start to appear between your teeth.After a Deep Dental Cleaning:
Deep dental cleaning is the standard treatment for gum disease. While you might expect your gums to return to normal afterward, this isn’t always the case. As the gums heal and the inflammation goes down, some shrinkage can occur, leading to the loss of papillae and the appearance of black triangles.After Orthodontic Treatment:
Crowded teeth can affect the shape and position of the papillae. Once the teeth are realigned through orthodontic treatment, small or missing papillae may become noticeable in certain areas, creating black triangles.Chronic Trauma:
In addition to inflammation, other factors like chronic trauma can cause gums to recede. This often occurs when too much pressure is applied while brushing or when using a hard-bristled toothbrush.Treatment Options for Black Triangles
In some cases, no treatment is needed if the black triangles are stable and don’t cause cosmetic concerns (for example, if they aren’t noticeable when you talk or smile). However, if they bother you or tend to trap plaque and food, filling these gaps may be necessary.
Composite Bonding:
A tooth-colored material can be used to fill the black triangles. This is one of the simplest and most affordable methods, and it can provide long-lasting results if you maintain good oral hygiene. Your dentist will select a color that matches your natural teeth and bond the composite material to reshape the area between your teeth.Orthodontics:
If black triangles are caused by the shape of triangular teeth, one option is to reduce a thin layer of enamel between the teeth and bring them closer together through orthodontic treatment. This procedure is called interproximal reduction (IPR). After aligning the teeth with braces or clear aligners, the spaces will disappear within a few days.Veneers:
Veneers are thin, tooth-colored shells made of porcelain that cover the front surface of your teeth. They’re great for fixing discoloration, chips, and minor misalignment, and they can also fill in black triangles, giving you a durable and aesthetically pleasing result. The only downside compared to composite bonding is that veneers are more expensive and require some trimming and preparation of your teeth.Crowns:
Unlike veneers, dental crowns cover the entire tooth. The process involves reshaping the tooth to make room for the crown, which is designed to hide the dark spaces between your teeth. However, compared to fillings and veneers, crowns are more invasive because they require removing a larger portion of the tooth, making them a less gentle option.Gum Grafting:
If you're a good candidate, gum grafting can be an effective option for closing black triangles while also strengthening your gums. The surgical procedure usually involves taking a small piece of soft tissue from the roof of your mouth and placing it over the receded area.Although effective, rebuilding gum tissue between teeth can be challenging due to limited blood flow in that region. This can lead to imperfect or unpredictable long-term results. To learn more, talk to your dentist or periodontist about whether a gum graft might be the right solution for you.
2. Tooth Discoloration or Dental Staining
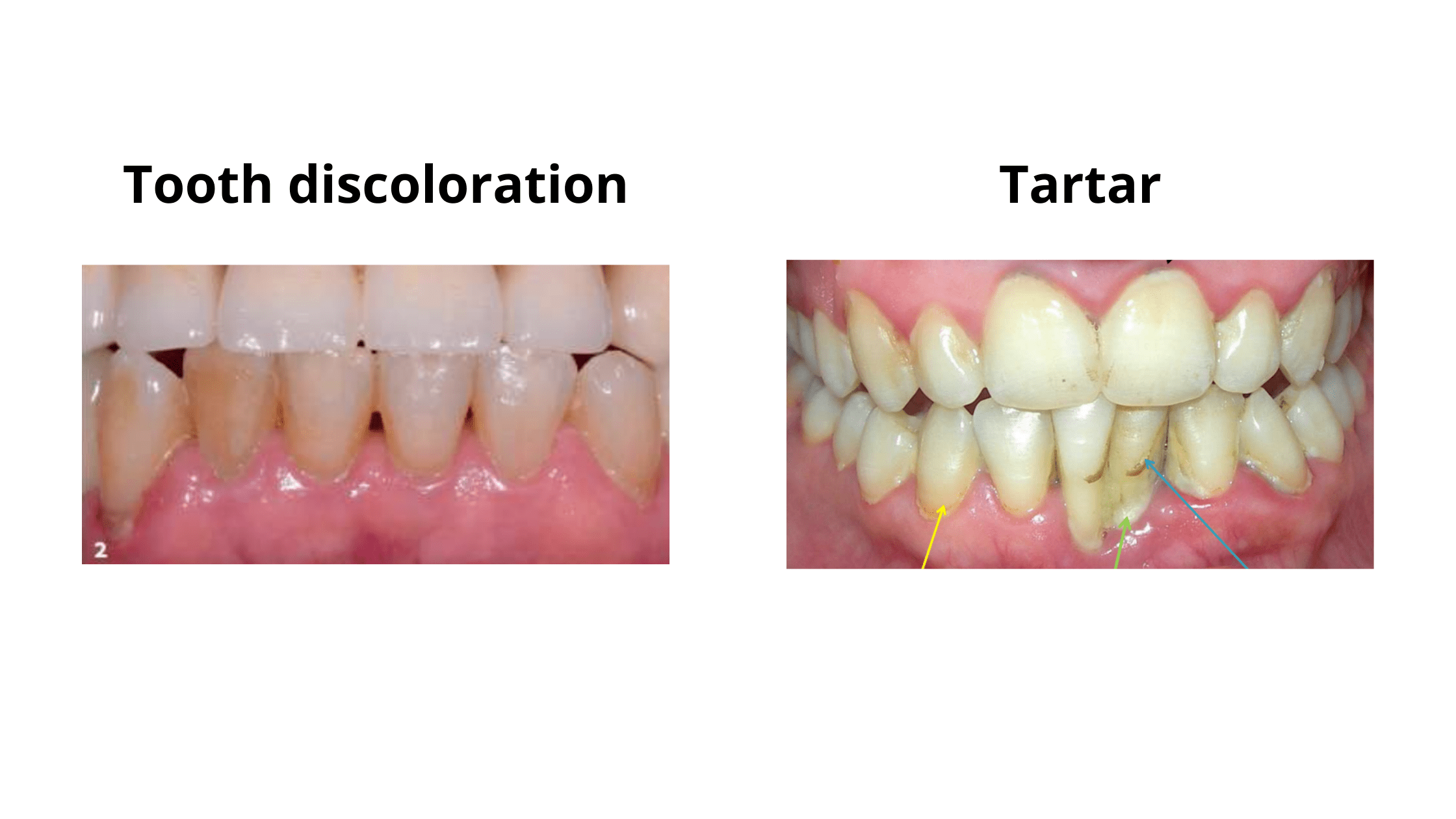
Blackness between teeth can sometimes indicate extrinsic staining, often caused by pigment compounds in certain foods (such as coffee, tea, and red wine) or tobacco.
Because our teeth are naturally porous, they can absorb different substances, including those that lead to staining. These pigment compounds seep into the outer tooth layer and mix with its minerals, causing yellow or brown spots that make teeth appear darker and duller.
When food is the culprit, this staining is called "extrinsic," as it's limited to the tooth's outer surface. The good news? It's easier to remove with proper oral hygiene or at-home whitening solutions.
It's important not to confuse staining with cavities. While discoloration only affects the tooth’s shade, cavities eat away at the tooth structure and can lead to more serious complications.
Treatment Options
The good news is that extrinsic dental stains are not permanent and can disappear with better oral hygiene and cutting back on stain-causing foods. You can actually remove these discolorations by simply brushing regularly with the right technique!
For faster results, at-home whitening solutions like whitening strips, kits, and toothpaste can be effective. These typically contain hydrogen peroxide, a powerful agent that breaks down the pigment compounds responsible for staining.
For immediate, long-lasting results, in-office whitening is the best option. During this procedure, your dentist will apply a highly concentrated whitening gel to your teeth, leaving it on for a few minutes. Just one session can lead to a dramatic improvement in your smile.
3. Plaque & Tartar:
Dental plaque is a thin, whitish film that builds up on your teeth when you skip brushing and flossing. Aside from water, it’s primarily made up of bacteria, which account for 70-80% of its dry weight!
Plaque forms constantly, even just minutes after a thorough brushing. That’s why it’s recommended to brush at least twice a day and floss daily.
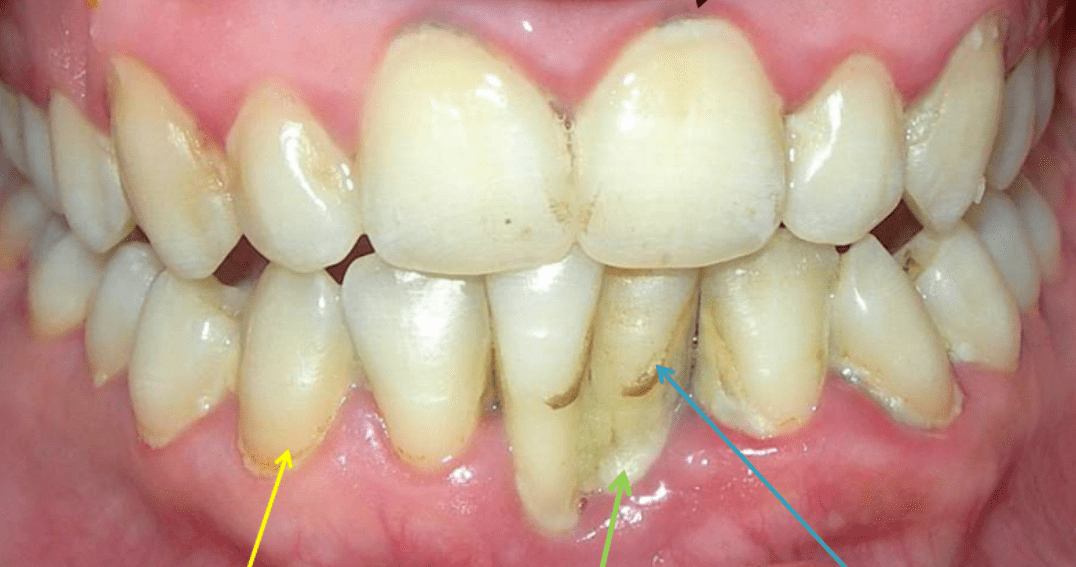
In small amounts, plaque isn’t easily noticeable. But as it accumulates, it can turn yellowish. Over time, it absorbs minerals from saliva and food, hardening into a darker, tougher substance known as tartar.
The spaces between your teeth and around the gum line are especially prone to plaque and tartar buildup, as their narrow gaps provide the perfect environment for bacteria to thrive.
Blackness Between Teeth: Could It Be Tartar?
Initially, tartar appears as a hard, porous, yellowish buildup on the teeth. When exposed to pigmented foods like tea or coffee, it can turn brown or even black.
Tartar can also form below the gum line, known as subgingival tartar. In this area, it often takes on a black color as it mixes with blood and gingival fluid. Since subgingival tartar is hidden beneath the gums, it’s not visible and can go unnoticed.
Complications of Plaque and Tartar
Plaque and tartar are the leading culprits behind gum disease and cavities. If they’re allowed to remain on your teeth for too long, they can cause significant damage and jeopardize your oral health. Some potential complications include:
- Bone Loss Around Teeth
- Gum Recession
- Tooth Loosening
- Infections and Abscesses
- Tooth Loss
Treatment
Preventing plaque and tartar buildup is the best way to avoid dental issues and complications.
To keep your teeth healthy, brush regularly with fluoride toothpaste and clean between your teeth every day. You can use dental floss, an interdental brush, or a water flosser—whichever tool you prefer, just make sure to use it daily.
While you can manage plaque buildup at home, tartar is more challenging to remove on your own. To get rid of tartar, you'll need a professional cleaning from your dentist.
If tartar has formed deep under the gum line, you may require an additional procedure called root planing. This involves cleaning below the gum line to smooth the root surfaces and promote gum health.
Your dentist might also prescribe an antiseptic mouthwash to eliminate any remaining bacteria in your gums.
4. Tooth Decay:
Tooth decay is one of the most common diseases globally. According to a CDC report, 1 in 4 adults aged 20 to 64 has at least one cavity.
There are different types of dental cavities based on their location in your teeth. Two among them:
- Interdental or Interproximal Decay: This type of decay occurs between the teeth and is quite common. It often happens if you skip flossing or cleaning between your teeth.
- Root Decay: Root decay begins at the gum line and can extend to the roots and areas between your teeth. It primarily affects older adults, especially those with gum recession. When gums recede, they expose the tooth roots. The roots are not as resilient as enamel. Consequently, root decay can progress quickly toward the nerves.
What Does Tooth Decay Look Like?
In its early stages, tooth decay may not cause any pain, so it can easily go unnoticed. At this point, it often appears as rough, whitish, or brownish spots on the surface of the tooth.
Decay is even harder to detect when it starts between your teeth, as these areas are out of sight. To check for interdental cavities, use dental floss. When you floss, the surfaces between your teeth should feel smooth, and the floss should come out without any tearing or damage. If the floss tears or gets damaged, it could indicate decay.
As decay progresses, it forms black holes or cavities that become more visible. You might also experience increased tooth sensitivity, especially to cold, heat, or pressure.
Treatment Options
Again, the best way to deal with tooth decay is to prevent it from happening in the first place. You can do this by maintaining good oral hygiene and visiting your dentist regularly for check-ups and professional cleanings.
If caught early, tooth decay is easy to treat. A simple remineralizing treatment might be all you need to restore the lost minerals in the tooth.
When decay has progressed but isn’t too severe, the solution usually involves removing the damaged tissue and filling the tooth.
For deeper decay that has reached the tooth’s nerve (pulp), a root canal may be necessary to remove the infection. Afterward, your dentist might suggest placing a crown to rebuild the tooth and protect it from further damage.
- Basics of oral health: Cavities https://www.cdc.gov/oralhealth/fast-facts/cavities/
- Dental plaque https://en.wikipedia.org/wiki/Dental_plaque
- Black staining: an overview for the general dental practitioner https://www.nature.com/articles/s41415-022-4345-0