Revealing cavities under a crown: What you need to know
 While crowns, fillings, and other dental restorations aim to protect your teeth for years to come, their lifespan is not limitless.
While crowns, fillings, and other dental restorations aim to protect your teeth for years to come, their lifespan is not limitless.
The risk of failure and complications increases with age. These can range from fractures, infections, or loosening. However, cavities are one of the most frequent and well-known complications associated with dental crowns.
In this article, we will discuss why crowned teeth can develop cavities, the different treatment options, and the best strategies to prevent this common issue.
In this article:
1. How can crowned teeth get cavities?
2. When it's your dentist's fault
3. What can cause cavities under crowns?
4. Symptoms of a cavity under a crown:
5. How is cavity under a crown treated?
6. Preventing future cavities:
How can crowned teeth get cavities?
Tooth decay is a common dental condition. According to a CDC report, nearly 90% of adults have had at least one cavity.It happens when harmful bacteria in your mouth feed on sugars and release acids. When acid attacks on your teeth are too frequent and long-lasting, they can gradually wear down your teeth, eventually leading to cavities.
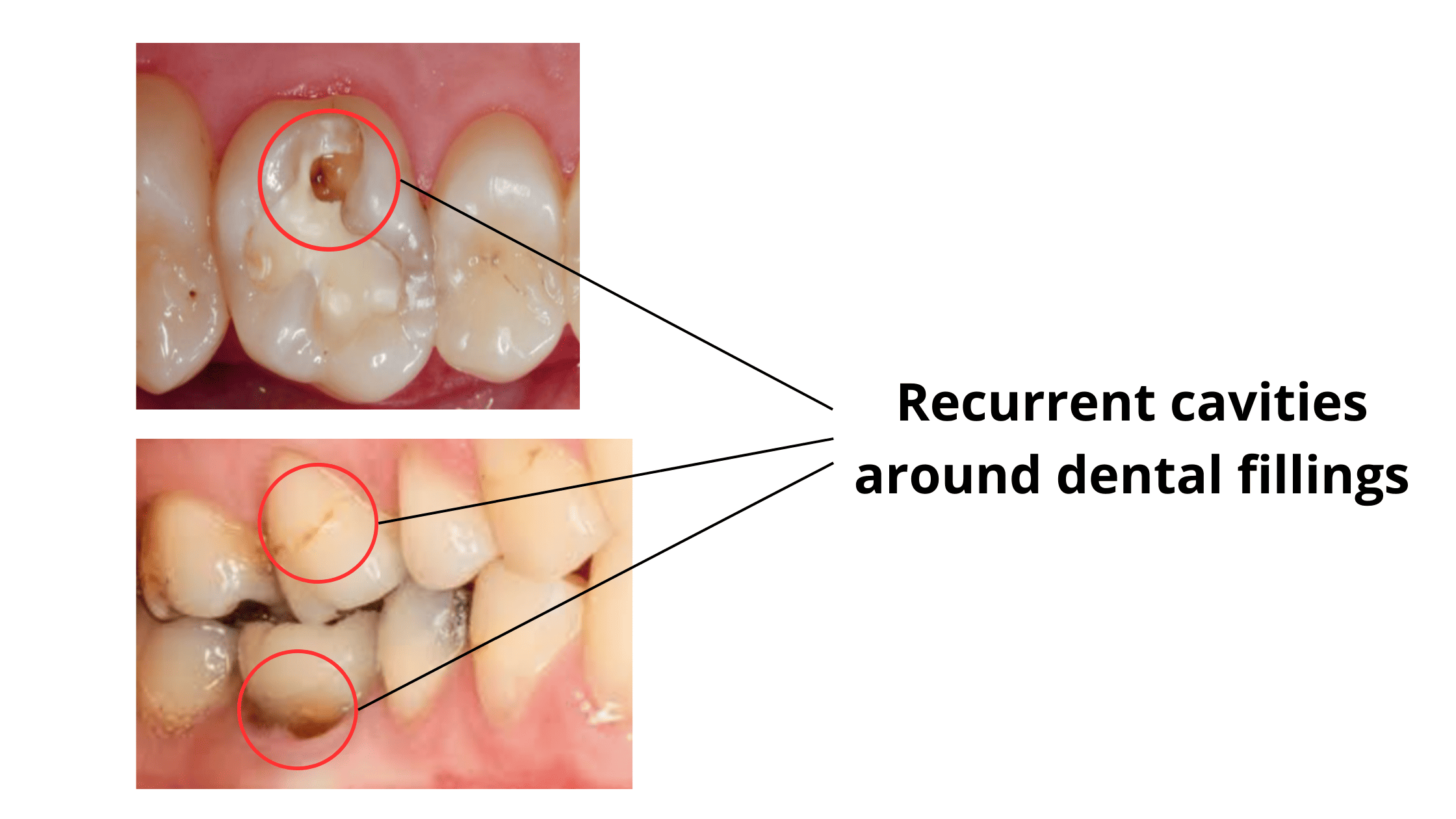
When decay develops under or around a dental crown, it’s called a recurrent or secondary cavity. This simply means the decay has returned, even though it was completely treated.
Crowns don’t make your tooth immune to decay. They can actually make it even more prone in some cases.
How can dental crowns increase the risk of cavities?
To place a crown, your dentist must trim down your natural tooth.
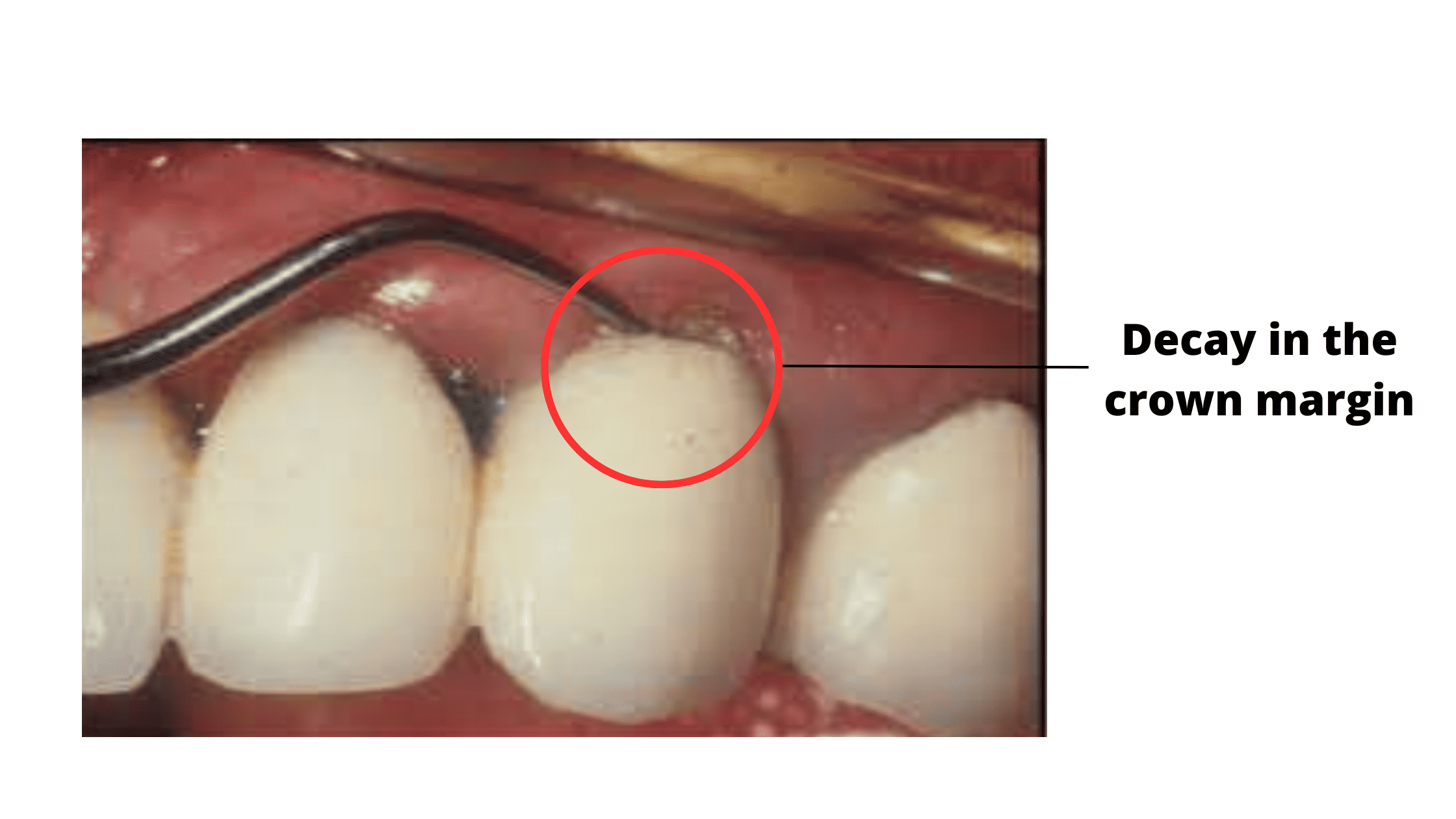
This creates a margin near the gum line, where the crown edge meets the tooth. The crown margins or edges are where cavities are most likely to form.
Why? Because it's a rougher area that naturally traps more plaque and food.
If plaque builds up around this area and isn’t removed with proper brushing and flossing, bacteria can slip into the tiny space between the tooth and crown.
The result? More acid attacks and a higher chance of decay forming under your crown.
When it's your dentist's fault
Secondary cavities are usually new lesions that develop slowly over time. Most of the time, it's not the dentist's fault.But what if your dentist accidentally left some decay behind before placing your crown? That’s what we call a residual cavity.
This is less likely to occur if the decay removal and crown placement procedures were done correctly, but unfortunately, it can still happen occasionally.
These aren't new lesions—they occur when untreated decay continues to grow and worsen. The damage can appear anywhere under the crown, not just near the gum line.
The tricky part is that these can hide under the crown, making them difficult to spot immediately. So you may not notice them until they've already done some serious damage.
The first culprit behind cavities under crowns
Plaque is the main culprit.It’s a white, sticky film full of bacteria that constantly builds up on our teeth.
And as mentioned earlier, crowns can actually promote more plaque buildup—especially around the margin where the crown meets your natural tooth.
That’s why maintaining good oral hygiene becomes even more important after receiving a crown or any dental restoration.
Other factors that can directly or indirectly increase your risk of developing cavities include:
- The age of the crown:
Crowns typically last between 15 to 20 years, with metal crowns being the most durable. However, over time, the crown's surface can become rough and worn, making it more prone to plaque buildup.
Bacteria can then create tiny gaps, allowing them to seep deep beneath the crown. If your crown shows signs of wear or damage, it might be time to consider replacing it. - Poorly shaped crown:
A poorly shaped crown that doesn't properly touch the neighboring teeth can create spaces where plaque can accumulate. This can result in cavities forming between the teeth. A badly fitted crown can also damage your gum tissue, leading to inflammation and receding gums. - Gaps at the crown margin:
The crown should fit snugly over the tooth without leaving any gaps. Even the smallest defects can cause leakage, allowing saliva, food, and bacteria to get under the crown and damage the tooth beneath. - Poor oral hygiene:
Your oral hygiene must be flawless to keep the area around the crown healthy and plaque-free. This will help your crown last as long as possible. - Receding gums:
When the gums recede, the tooth roots become exposed, leaving them vulnerable to plaque buildup and bacteria. Because roots are naturally more sensitive to acid attack, they can decay quicker than other parts of the tooth. (7)
Symptoms of a cavity under a crown:
Symptoms of cavities under a crown are not always obvious. Here's what to look out for:- Dark discoloration: A blackish or greyish color along the edge of the crown, close to the gum line, is one of the telltale signs of decay. This may be associated by a widening gap between the crown and tooth, making it easier for more plaque and food debris to get trapped.
- Soft substance: If you notice a soft stuff coming out from the crown margin when flossing, it could be a sign that your dental tissues are breaking down due to bacteria.
- Decay between teeth: Decay that develops between the teeth can be challenging to spot.
To check for it, try flossing the area gently. If the floss catches, frays, or tears instead of gliding smoothly between your teeth, it could be a sign of a cavity. - Sensitivity and pain: If your tooth is still alive and hasn’t had a root canal, decay can cause sensitivity, especially when eating or drinking something sweet, cold, or acidic.
- Root canal treated teeth: Even crowned teeth with root canal treatment are not immune to cavities. You might not feel any pain at first, which can make it harder to notice the damage.
If you notice any of these symptoms, don’t wait to see your dentist.
Delaying treatment will only make the problem worse.
If decay is caught early, the tooth can often be repaired without losing your crown.
At advanced stages, it becomes harder to save the crown because the underlying tooth is too damaged and weakened.
How is cavity under a crown treated?
The treatment depends on the severity and location of the cavity. Common options include:- Minor decay affecting the marginal area: If the damage is minor and affects only the margin of the crown near the gum line, your dentist will try to remove the decay while keeping your crown in place. The damaged area is then repaired with a tooth-colored filling material.
- Severe decay: When decay is extensive or hidden beneath the crown, saving the crown is often not possible, and it will need to be removed. After removing the decay, a new crown can be made to fit the reshaped tooth.
- Infection or failed root canal treatment: If the tooth has had a root canal that failed, the crown will need to be removed. A retreatment or second root canal will be done to clear the infection. Once the treatment is complete, a new crown will be placed to protect the tooth.
Preventing future cavities:
Here are some tips to help your crown last as long as possible- Maintain good oral hygiene: Brush your teeth at least twice a day with fluoride toothpaste and floss daily to remove plaque and prevent decay around the crown.
- Limit sugary and acidic foods and drinks: These feed the "BAD" bacteria in your mouth that cause cavities.
- Visit your dentist regularly: Routine check-ups and professional cleanings help catch any early signs of problems before they got too far.
- Use fluoride products: Fluoride strengthens your teeth and helps prevent cavities. Consider rinsing daily or weekly with a fluoride mouthwash, as directed by your dentist.
- Discuss preventive options with your dentist: If you’re prone to cavities, dental sealants, fluoride varnishes, or more frequent cleanings may provide extra protection.
- Recurrent Caries - an overview | ScienceDirect Topics
- Secondary caries in crowned teeth: correlation of clinical and radiographic findings - PubMed (nih.gov)
- Recurrent caries at crown margins: making a decision on treatment - PubMed (nih.gov)
- Success and failure of fixed bridgework - PubMed (nih.gov)
- 10: Periodontal–Restorative Interface | Pocket Dentistry
- Conventional_and_adhesive_luting_cements.pdf (ucm.es)
- Prosthetic crowns and other clinical risk indicators of caries among old-old Swedish adults: findings from the KEOHS Project. Kungsholmen Elders Oral Health Study | Request PDF (researchgate.net)
- LES-ECHECS-EN-PROTHESE-CONJOINTE-CAUSES.pdf (univ-tlemcen.dz)