Crown without root canal: is it possible and what to expect?
 Although root canals and dental crowns are two different procedures, they share the same goal. To protect and save the tooth for as long as possible.
Although root canals and dental crowns are two different procedures, they share the same goal. To protect and save the tooth for as long as possible.
Root canal treatment involves treating the inside of the tooth when the pulp is irreversibly damaged. A crown, on the other hand, restores the visible part of the tooth.
You may think that placing a crown would automatically require a root canal as the two often go together. However, this is not always the case.
We will discuss in this article why a crown does not always require a root canal, when it is necessary, and what to expect in the long run.
Table of content
Why would you need a crown in the first place?
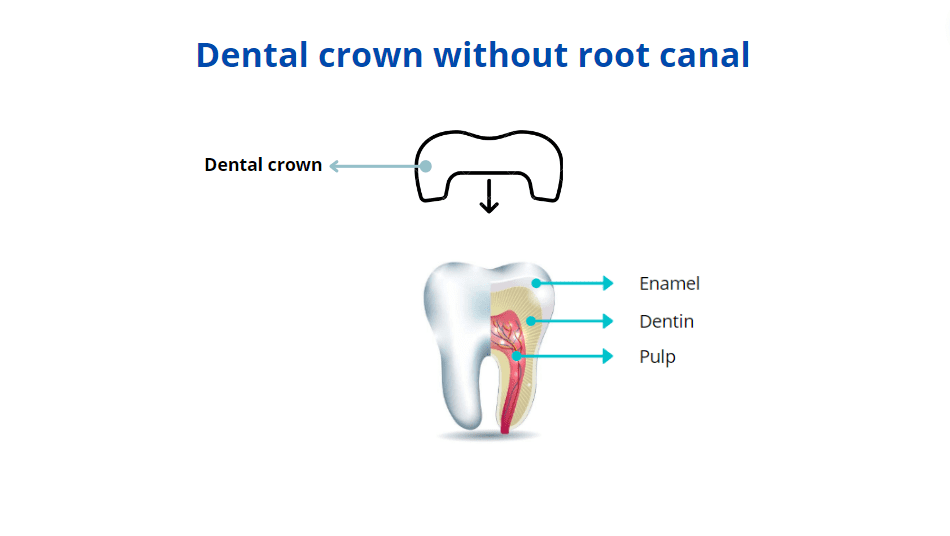
A dental crown is a permanent restoration that covers the visible part of the tooth. It is one of the most common procedures in dentistry.When your tooth is severely damaged by decay or trauma, it can no longer support a filling. In this case, a dental crown may be the only way to restore and save it.
It can also provide high aesthetic results when it comes to restoring front teeth. Although veneers are the best option in this regard, they have their limitations. Your dentist may recommend crowns over veneers if there are deep stains or significant damage.
Dental crowns can also correct minor crowding or malposition, so you don't have to wear braces.
Dental crowns can protect both vital teeth and those that have had root canal treatment.
For vital teeth, crowns shield the pulp from external stressors like bacteria, plaque, and food debris, helping the tooth last longer.
For non-vital teeth (those with root canal treatment), crowns strengthen the tooth and protect it from further damage. Since root canal-treated teeth are more fragile and prone to cracking, placing a crown on them is a common practice.
Why is root canal treatment not always needed before getting a dental crown?
The basic rule in dentistry is to save as much healthy tooth tissue as possible.For example, if you have stains on your teeth, you’d probably choose a simple whitening treatment. You probably won't go for more invasive and costly options like fillings or veneers that require drilling into healthy enamel.
The same idea applies when placing a crown. If your tooth’s nerve is healthy and alive, there’s no need for a root canal treatment, which can actually make the tooth weaker.
A root canal is usually not needed if:
- The decay is far from the nerve (pulp)
- The tooth is still strong and healthy
- There are no signs of infection
- Your tooth doesn’t hurt or feel sensitive
- The crown is being placed just for cosmetic reasons
Why should tooth nerves be saved whenever possible?
Saving the pulp (the tooth’s nerve and blood supply) means keeping the tooth’s natural defenses strong.A tooth with a healthy nerve is usually tougher and better at handling chewing forces. Teeth that have had root canal treatment tend to be more brittle and have a slightly higher chance of cracking or breaking.
That said, studies show that crowned teeth can last many years whether they have a root canal or not.
The real challenge comes if the tooth needs more treatment later. Fixing a tooth that already had a root canal is more complicated and riskier because the tooth has lost more of its natural structure.
If it gets infected again, it’s more likely that the tooth will need to be removed compared to a tooth with a healthy nerve.
Situations Where Root Canal Treatment Might Be Needed
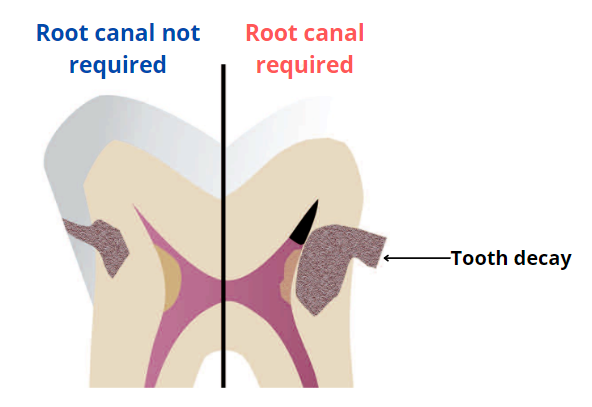
Sometimes, a root canal is necessary to prevent complications and help your crown last longer. These situations include:
- Irreversible pulp damage: When tooth decay reaches the pulp, it can cause permanent damage and risk infection. Symptoms often include a deep cavity and sharp, intense pain.
- Gum abscess: This is an advanced stage of tooth infection. A root canal is needed to disinfect the tooth and create a strong foundation for the crown to sit on.
- Thin dentin layer: If the tooth is severely damaged and doesn’t have enough structure to protect the pulp, infection is more likely. Root canal treatment helps prevent this.
- Severe gum disease: Advanced gum disease can expose the nerves, causing extreme sensitivity when eating or drinking. A root canal can relieve this pain.
Takeaway
While a root canal isn’t always required before placing a dental crown, sometimes it becomes necessary.This is especially true when the tooth is weak and at high risk of infection in the near future. If infection occurs, you may lose your crown much sooner than expected—crowns are designed to last for years, even decades.
- Assessment of the periapical and clinical status of crowned teeth over 25 years https://www.sciencedirect.com/science/article/abs/pii/S0300571296000085
- Fate of vital pulps beneath a metal-ceramic crown or a bridge retainer https://pubmed.ncbi.nlm.nih.gov/16011770/