Gum Graft Failure Symptoms: Signs You Shouldn't Ignore (pictures)
 Gum grafting is a highly successful procedure that helps cover areas of gum recession, restoring both strength and health to your gums. In the days and weeks following the surgery, you’ll gradually notice improvements in your gums’ appearance.
Gum grafting is a highly successful procedure that helps cover areas of gum recession, restoring both strength and health to your gums. In the days and weeks following the surgery, you’ll gradually notice improvements in your gums’ appearance.
Like any surgical procedure, however, gum grafting isn’t without risks. One possible complication is graft failure. The first few days after surgery are the most critical, as this is when the graft should survive and integrate with the surrounding tissue.
In this article, we’ll cover the most common causes of graft failure, the telltale symptoms to look for, and your options if it happens.
In this article...
The Most Common Causes of Gum Graft Failure:
The first few days following the gum graft are the most critical. Why? During this time, the graft must attach to its recipient site and form new blood vessels to survive.So, you must be careful not to destabilize the graft with your tongue, fingers, or any objects during the first week. Otherwise, you risk preventing it from properly attaching and taking hold.
When blood flow to the graft isn’t properly established, the tissue may fail to integrate and eventually die off. We call this necrosis.
The most common causes of graft failure are:
1. Technical mistake:
The technique used plays a major role in the success of any gum graft procedure. Even a small mistake during surgery can prevent the graft from integrating and healing properly.2. The graft did not take hold properly:
Once the graft is placed and sutured, it must not shift or change position, as this can disturb the blood clot—an essential part of the healing process.During the first few days, the graft depends on the underlying recipient site to receive most of the nutrients and moisture it needs. So be careful not to touch or dislodge the graft, especially during the first three days.
3. Smoking and diabetes:
Both smoking and uncontrolled diabetes (high blood sugar) can disrupt blood flow to the graft, decrease the immune response and increase the risk of complications.Smoking has also been shown to significantly increase the risk of pain and bleeding after surgery.
So, if you have diabetes, make sure your blood sugar level stays within the normal range, and avoid smoking—especially during the first two weeks.
4. You have injured the surgical site:
If you accidentally injure your graft, you can not only rip the dressing off and cause pain, but you might also dislodge the graft and trigger bleeding. This can stop the graft from getting the nutrients it needs, and it may fail to survive.Symptoms of Gum Graft Failure
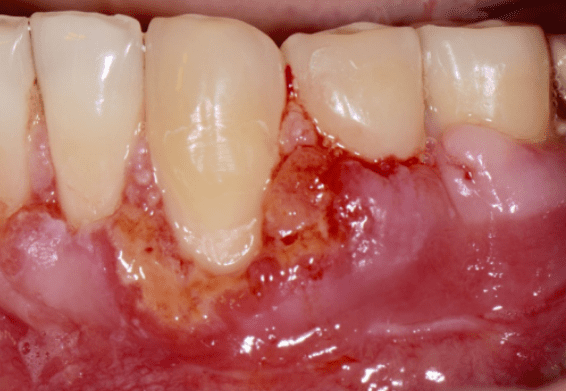
1. Failure by Necrosis
Graft necrosis means the tissue did not survive, and it’s one of the most common complications following gum graft surgery.

Symptoms of graft necrosis often include:
- Persistent pain
- A foul smell and taste
- A whitish area that doesn’t improve
- The graft is sloughing off.
- Healing that takes longer than expected
Not all whitish discoloration means something is wrong. It’s totally normal for the graft to appear white or gray during the first week.
This happens because the outer surface of the graft naturally sheds around the third day. Your body then begins replacing this dead, white layer with new, living tissue. As healing continues, the graft should gradually blend in with the natural color of your gums.
What should concern you is if symptoms last too long, such as persistent redness, swelling, pain, or poor healing that seems to take longer than expected. These may be signs that the graft is failing.
It’s always best to contact your dentist if in doubt.
How Is Gum Graft Necrosis Treated?
If graft necrosis occurs, your dentist will clean the area with an antiseptic solution to remove any dead tissue while saving the healthy parts of the graft. Painkillers and antibiotics may be prescribed as needed.Once the area has completely healed (typically in about 3 months), you can discuss with your dentist the option of a second graft.
2. Gum Graft Infection
Gum graft infection is rare, but it can happen if bacteria enter the surgical site. If not treated early, it can lead to graft failure.
People with weakened immune systems, such as those with diabetes, are at a higher risk of post-operative infection.
Watch for the following symptoms:
- Persistent pain that doesn't improve
- Swelling and redness around the graft site that get worse
- Clear-yellow fluid (pus) leaking from the surgical site
How Is Infection Managed?
The best way to manage infection is to prevent it from happening in the first place.- Follow your surgeon's post-op instructions carefully, including all scheduled follow-up visits to monitor healing.
- Make sure stitches are removed on time, as they can trap food and plaque, increasing the risk of infection.
- Rinse your mouth gently with warm salt water starting on the second day to help reduce bacteria and support healing.
If an infection does occur, your dentist will:
- Rinse the area with an antiseptic solution
- Remove any dead or infected tissue
- Prescribe antibiotics, if needed
3. You're Not Happy with the Graft Results
This isn’t a true failure, but if the graft didn't achieve the results you and your dentist were hoping for, it can still feel disappointing.
One of the main reasons for having a gum graft is to cover exposed roots and improve the appearance of your smile. This is especially true for the more visible front teeth.
Aside from root coverage, factors like color, contour, and texture of your gums also play a big role.
So, when a graft doesn't fully meet your aesthetic expectations, it may be considered a "partial failure."
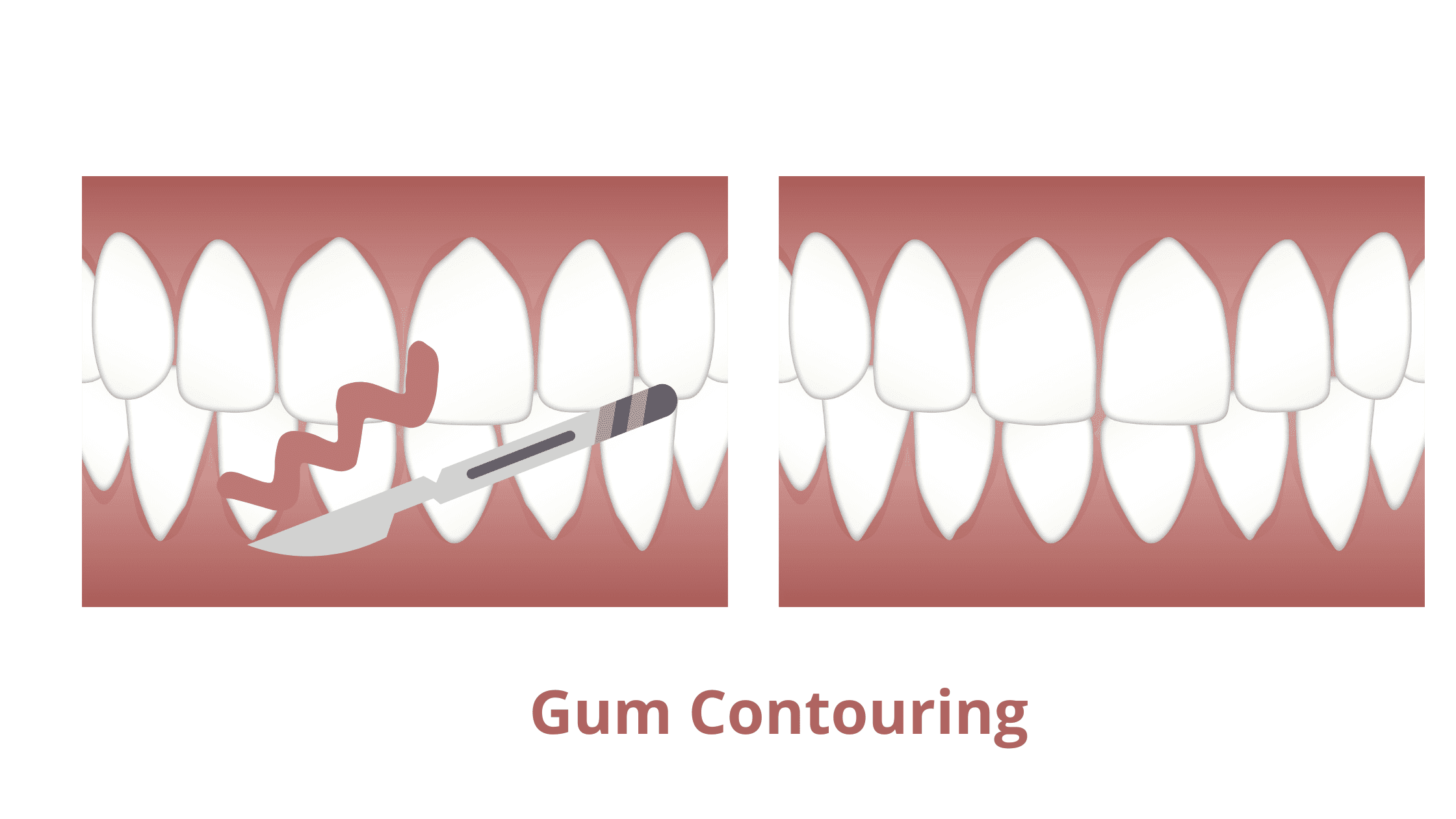
How Is Aesthetic Failure Managed?
If the root coverage is incomplete, your dentist may suggest a second grafting procedure, though this isn’t always possible and depends on your specific case.In cases where the gum line is uneven or there’s a surface irregularity, your dentist can correct it by reshaping the tissue using specialized instruments or a laser. This technique is called gingival recontouring or gingivoplasty.
Takeaway
While gum grafting is generally a highly successful procedure, recognizing the early signs of failure can save your results.It's always better to catch issues early, when the graft is only partially failing, than to wait until it's too late.
So if something doesn’t feel right, don’t wait. Contact your dentist as soon as possible.
- Color Atlas of Dental Medicine: Periodontology Book by Edith Rateitschak-Pluss and Herbert F. Wolf
- Postoperative complications following gingival augmentation procedures https://pubmed.ncbi.nlm.nih.gov/17209793/
- Skin graft vascularization involves precisely regulated regression and replacement of endothelial cells through both angiogenesis and vasculogenesis https://pubmed.ncbi.nlm.nih.gov/16525274/
- Interest in periodontology and preferences for treatment of localized gingival recessions https://pubmed.ncbi.nlm.nih.gov/15811055/
- Complications of free grafts of masticatory mucosa https://pubmed.ncbi.nlm.nih.gov/1079047/