Connective tissue graft: The gold standard for root coverage
In this article:
1. What is gum recession?
2. What is a connective tissue graf?
3. When would you need a connective tissue graft?
4. Connective tissue grafting techniques:
5. Pros and cons of connective tissue gum graft:
6. What to expect after the procedure:
7. The success rate of the connective tissue graft
8. Alternatives to connective tissue grafting
What is gum recession?
Gum recession is a condition where the gums pull away from the teeth, exposing more of the tooth or the root. Left untreated, it can lead to sensitivity, decay, and even tooth loss.Gum recession can affect anyone, but it is more common in adults over 40 years old. According to one study, more than 50 percent of the population has one or more sites with gingival recession of 1 mm or more. (1)
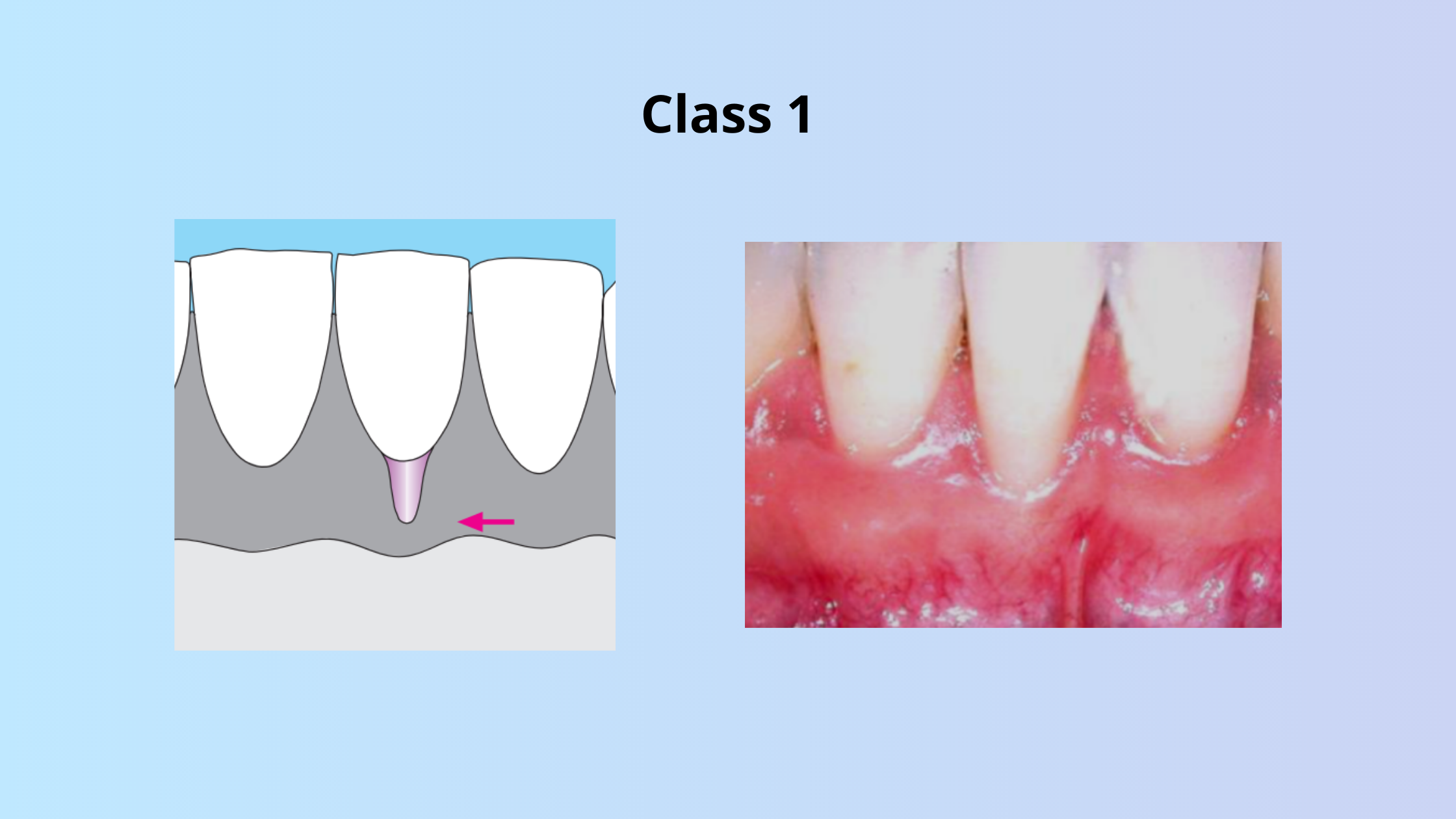
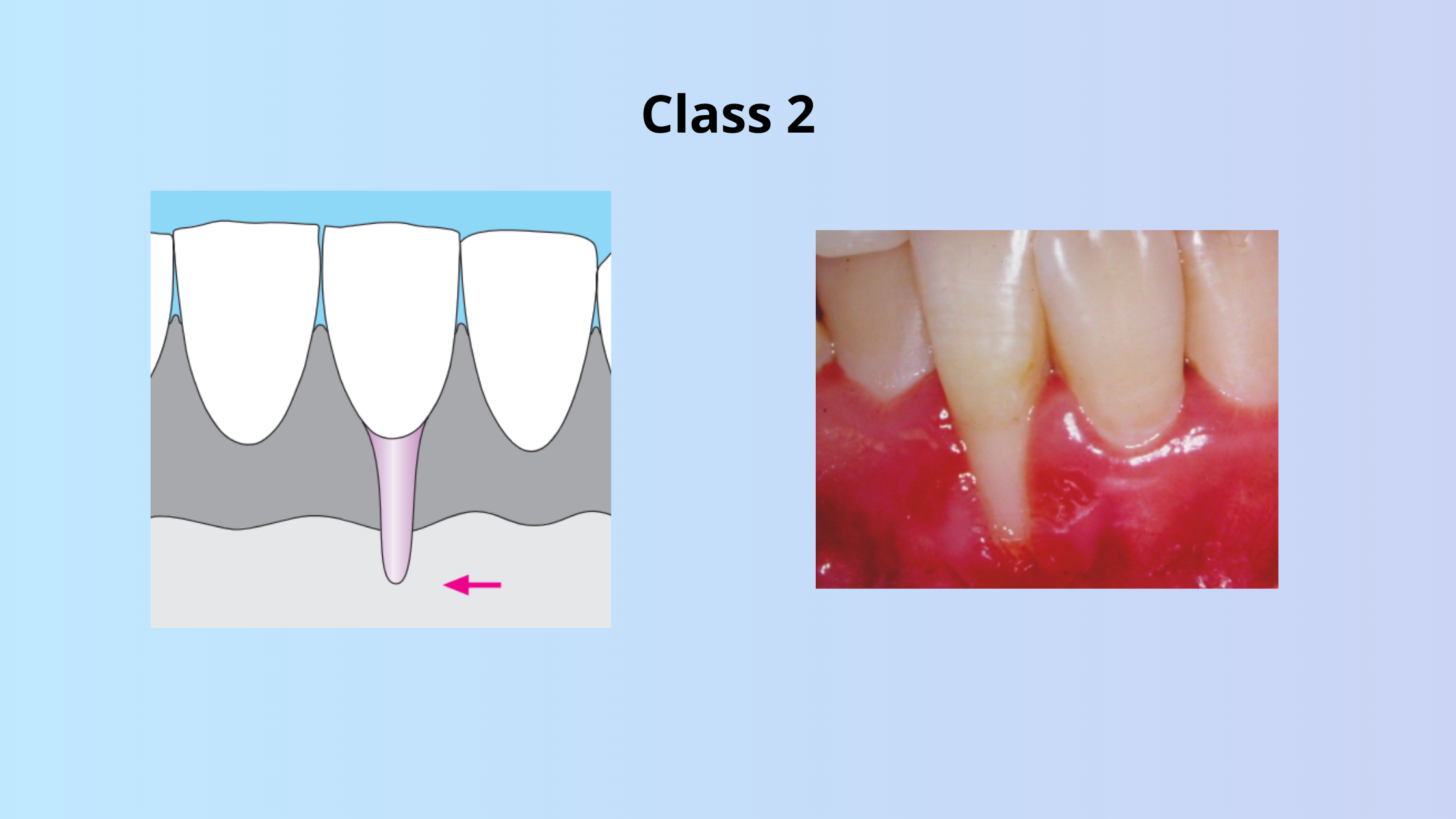
There are different types of gum recession according to Miller’s Classification:


What causes gums to recede?
The primary causes of gum recession are plaque and trauma.
Plaque is a sticky film of bacteria that forms on the teeth and can cause inflammation and infection of the gums. If not removed, it can initiate gum disease or periodontitis.
Trauma is any injury or damage to the gums, such as brushing too hard, using a toothpick, biting on something hard, or having a piercing.
Besides plaque and trauma, some factors increase the risk of gum recession even more. These include anatomical factors (thin gums), dental crowding, poor oral hygiene, medical condition, and aging.
Plaque is a sticky film of bacteria that forms on the teeth and can cause inflammation and infection of the gums. If not removed, it can initiate gum disease or periodontitis.
Trauma is any injury or damage to the gums, such as brushing too hard, using a toothpick, biting on something hard, or having a piercing.
Besides plaque and trauma, some factors increase the risk of gum recession even more. These include anatomical factors (thin gums), dental crowding, poor oral hygiene, medical condition, and aging.
What is a connective tissue graf?
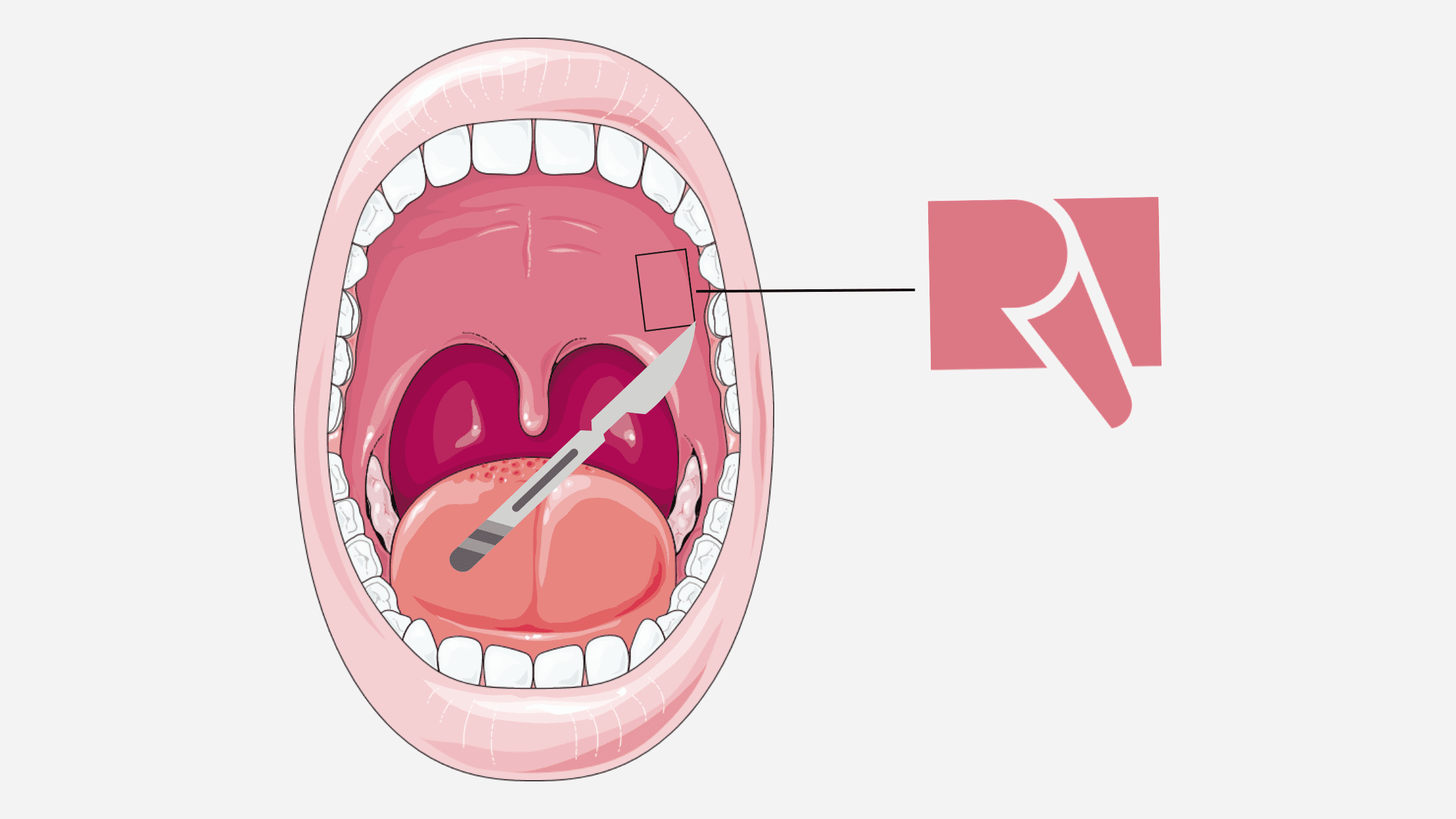
Connective tissue grafting is a technique that has long been considered the gold standard for covering recessions.It involves taking a small piece of tissue from the roof of your mouth and attaching it to the gum area where the root is exposed.
The term "autogenous" is used to describe this procedure because the graft used in connective tissue grafting is sourced from your own body. The word "auto" signifies "your own body," while "genous" refers to the origin of the graft.
This can help cover the root, protect it from damage, and improve the appearance of your smile.
When would you need a connective tissue graft?
Not all cases of gum recession actually require a gum graft. If your gum recession is stable and isn't causing any cosmetic or dental problems, you may not need surgery. In such cases, improving your oral hygiene and addressing the root causes of your recession can be sufficient.For example, if you've been brushing too hard or grinding your teeth, making changes in these habits and taking better care of your teeth may help prevent further recession.
However, if you have cosmetic concerns, dental sensitivity, root decay, or if your recession is progressing, a gum graft surgery could be a good option for you. Your dentist or periodontist will evaluate your specific situation and determine the most suitable technique for your needs.
Usually, connective tissue grafting is the ideal solution to cover recessions and restore the appearance of your gums, especially in the front part of your smile area.

Connective tissue grafting techniques:
The procedure of connective tissue grafting starts by preparing the area of recession (the recipient site).Your dentist will make a small cut in the gum to create space for the graft. Then, a tiny piece of skin or soft tissue, usually taken from the roof of the mouth (the donor site), will be placed into the prepared area and stitched in place using sutures.
These sutures help hold the graft securely and aid in the healing process.
There is not only one technique to perform a connective tissue graft. Here are the most commonly used:
1. Connective tissue graft associated with coronally advanced flap:
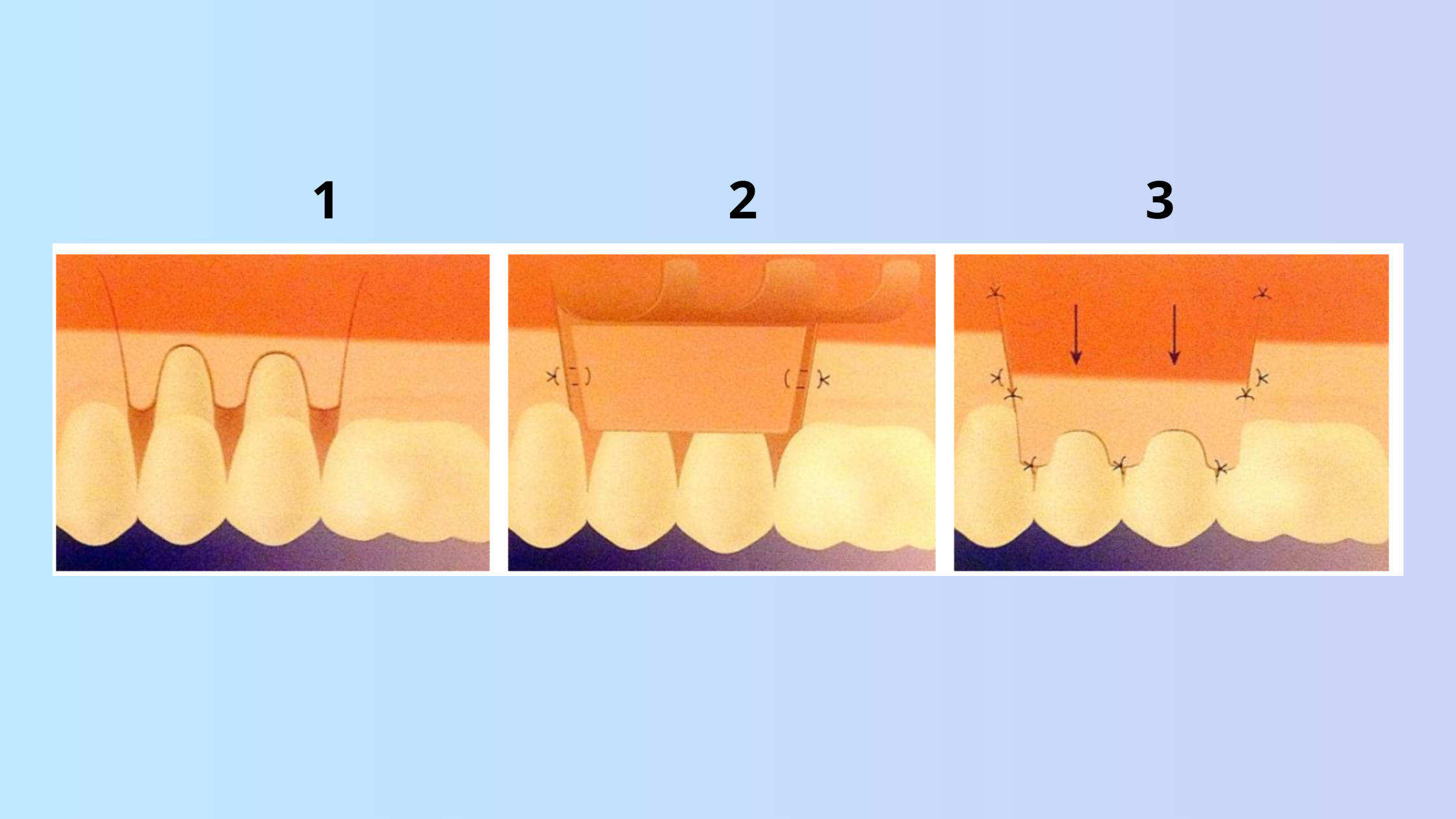
This is the most common technique used to treat root exposure. First, your dentist will harvest a small piece of connective tissue and place it over the exposed root. Then, they will carefully lift the gum tissue around the affected tooth and stitch it over the graft, completely covering the recession. This technique can be used to treat one or more teeth in the same area.
2. Connective tissue graft with laterally repositioned flap:
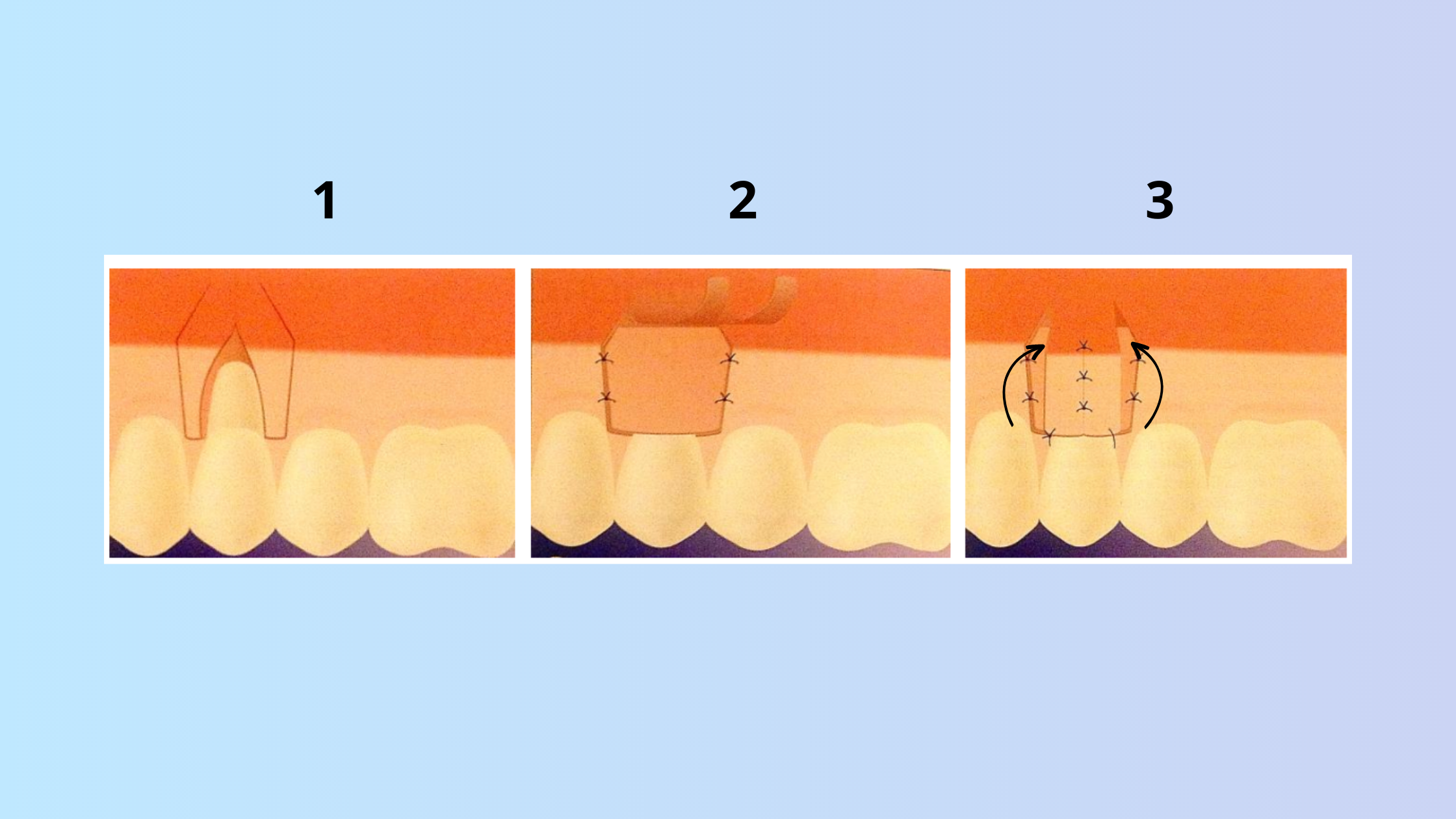
This technique is similar to the previous one, but instead of pulling up the gum tissue around the tooth, your dentist will move it sideways from an adjacent tooth. This technique can be used when there is enough gum tissue on one side of the tooth, but not on the other.
3. Envelope technique:
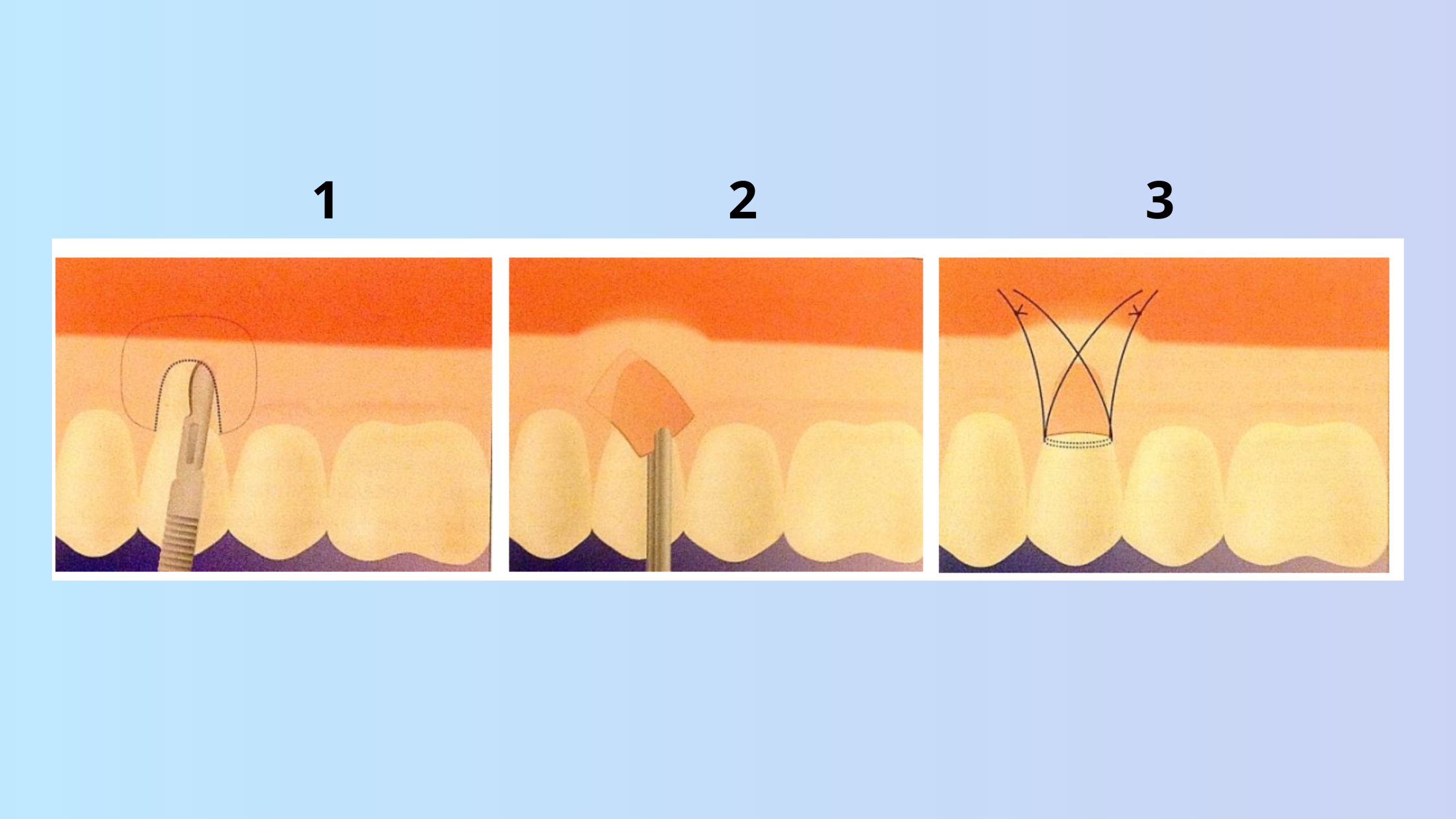
This technique is less invasive than the previous ones, as it involves making a single horizontal incision (without the need for a vertical incision to open the flap).
In this technique, your dentist will make a small incision in the gum tissue to create a pocket or envelope. Then, they will insert the connective tissue graft into the pocket and stitch it to the surrounding gum tissue.
4. Tunnel technique:
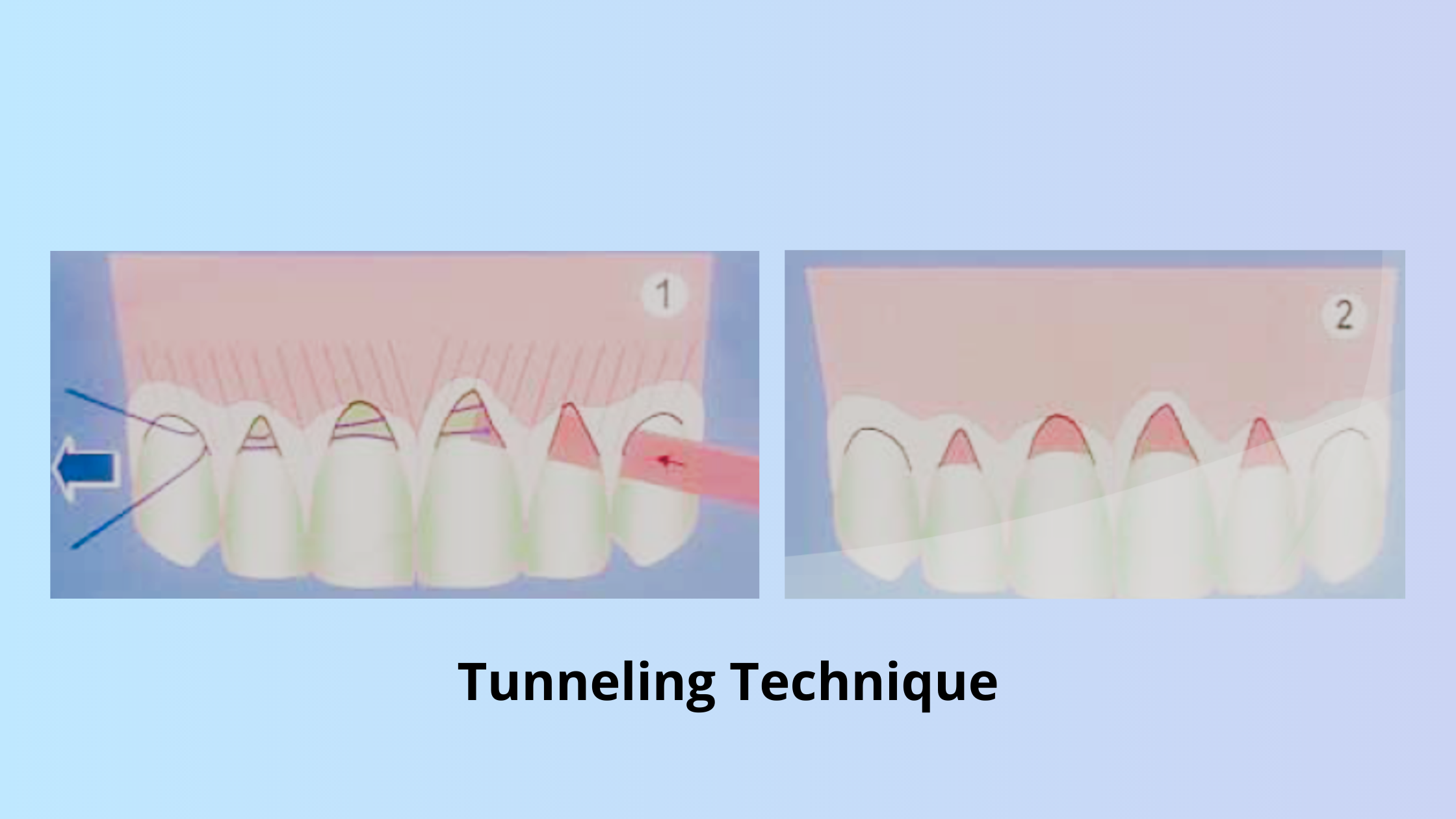
This technique is also minimally invasive, as it does not require any incisions or flaps. Your dentist will create a tunnel under the gum tissue along the affected teeth and insert the connective tissue graft through the tunnel. Then, they will use special instruments to position the graft over the exposed roots and secure it with stitches.
This technique can be used to treat several teeth in different areas of the mouth, as long as there is enough space under the gum tissue for the tunnel.
Pros and cons of connective tissue gum graft:
Pros:
- It can cover exposed roots and reduce tooth sensitivity.
- It can prevent further gum recession.
- It can improve the appearance of your smile and make your teeth look more even.
- It can reduce the risk of tooth decay and infection on the root surface.
- Connective tissue grafts have a higher survival rate compared to free gingival grafts.
Cons:
- It may cause some discomfort and bleeding in the donor and recipient sites.
- It may require additional sessions to achieve the desired result.
- It may have some complications, such as infection, inflammation, or graft failure.
- It is a very technique-sensitive procedure that requires a great deal of experience from the practitioner.
What to expect after the procedure:
As with any surgery, it is normal to experience some postoperative effects after the procedure. These are temporary and gradually subside over time. Here are some things you should know about what to expect after the procedure:- You may experience some bleeding, swelling, and pain in the donor and graft site. These are normal and temporary signs of healing. While it may take a little longer for the tenderness in the roof of your mouth to subside, you can expect a noticeable improvement after the first week.
- You can apply a cold compress to the affected area to reduce swelling and discomfort. You can also take over-the-counter pain relievers as directed by your dentist.
- You should avoid eating hard, crunchy, or sticky foods for at least a week after the procedure. These foods can irritate or dislodge the graft. You should also avoid smoking, drinking alcohol, or using a straw, as these can interfere with the healing process.
- Instead, opt for soft foods that are easy to chew and swallow, such as yogurt, soup, eggs, mashed potatoes, etc.
- You should maintain good oral hygiene after the procedure, but be gentle around the graft site. You should not brush or floss the graft area until it has healed completely.
- You can rinse your mouth with warm salt water or an antibacterial mouthwash after 24 to 48 hours to keep the area clean and prevent infection. You should also avoid touching or pulling on the graft with your tongue or fingers.
- You should follow up with your dentist regularly to monitor the healing of the graft. Your dentist will check if the graft has attached properly and if there are any signs of complications.
- The graft will gradually blend in with your natural gum tissue and cover the exposed root. The complete healing of the graft may take several weeks to months.
The success rate of the connective tissue graft
One of the benefits of the connective tissue graft is that it has a high survival rate. This means that the tissue that is taken from the roof of your mouth and placed over the exposed root of your tooth is likely to stay healthy and alive.This is because it receives blood supply from two sides. On the one hand, by the recipient bed and, on the other, by the gum flap that covers it.
When combined with a coronally advanced flap, the connective tissue graft can achieve high rates of total coverage of exposed roots. This means that the procedure has a significant potential to provide favorable cosmetic and functional outcomes.

Alternatives to connective tissue grafting
One of the downsides of connective tissue grafting is that it requires two surgical sites: the donor and recipient sites. This means more discomfort and a longer healing time for you.However, the good news is that there are alternatives to connective tissue grafting that eliminate the need for tissue from your palate. Some of these options include:
- Allograft: This is a type of graft that uses donated human tissue instead of your own. The tissue is processed and sterilized to eliminate any risk of disease transmission.
- Xenografts: In this approach, graft material is derived from animal sources. Xenografts provide a natural foundation for tissue growth and can be a suitable alternative for those who prefer not to use their own tissue.
- Platelet-rich plasma and growth factors: These are substances derived from your blood that can stimulate the healing and growth of your gum tissue. They are applied to the receding gum area along with a membrane that serves as a support for the new tissue.
These alternatives to connective tissue grafting may offer some advantages, such as less pain, faster recovery, and better aesthetic results. However, they may not be suitable for everyone or every case of gum recession.
Your dentist or periodontist can help you decide on the best option based on your oral health, the depth of your recession, and your budget.
- Does gingival recession require surgical treatment? https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4907322/
- The etiology and prevalence of gingival recession https://pubmed.ncbi.nlm.nih.gov/12636127/
- La Chirurgie plastique parodontale en 2015 : la greffe conjonctive est-elle toujours le gold standard ?
- TAUX DE RECOUVREMENT DES RÉCESSIONS GINGIVALES EN FONCTION DU TRAITEMENT APPLIQUÉ http://docnum.univ-lorraine.fr/public/BUPHA_TD_2014_MAGAR_CELINE.pdf
- Use of autologous platelet rich plasma to treat gingival recession in esthetic periodontal surgery https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3768186/
- A connective tissue graft envelope technique for the treatment of single gingival recessions: a 1-year study https://pubmed.ncbi.nlm.nih.gov/20072736/
- Coronally advanced flap + connective tissue graft techniques for the treatment of deep gingival recession in the lower incisors. A controlled randomized clinical trial https://pubmed.ncbi.nlm.nih.gov/24802283/