What does it mean to have sensitivity in one tooth?
 Does your tooth hurt when you eat something cold or sweet?
Does your tooth hurt when you eat something cold or sweet?
If so, you might be dealing with tooth sensitivity, also known as dentin hypersensitivity.
It often feels like a short, sharp pain — especially when you eat or drink something cold, hot, sweet, or acidic. The discomfort usually goes away once the trigger is removed.
When sensitivity affects just one tooth, it’s often a sign of a local problem, such as wear, tooth decay, gum recession, or a crack or fracture.
Spotting the real cause is the first step toward the right treatment.
Don’t worry, we’ll break it all down so you can better understand what’s actually going on with your tooth.
In this article:
1. Understanding the tooth sensitivity process
2. Potential Causes of One-Tooth Sensitivity
3. How to Stop Sensitivity in One Tooth (In 2 Steps)
4. When to See Your Dentist
5. Takeaway
Understanding the tooth sensitivity process
Before delving deeper into dental sensitivity, we must first take a look at the internal structure of a tooth.
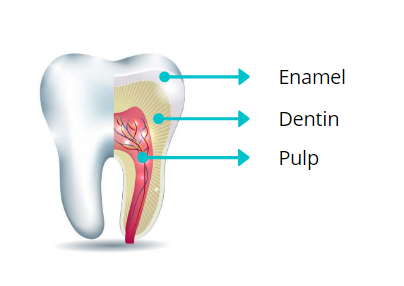 Each tooth is covered with hard protective layers — enamel on the outside and dentin underneath.
Each tooth is covered with hard protective layers — enamel on the outside and dentin underneath.
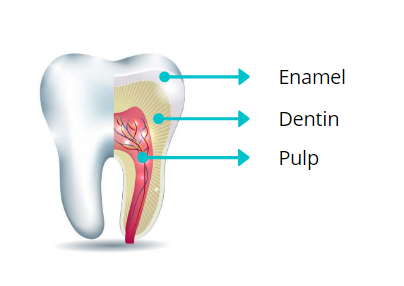 Each tooth is covered with hard protective layers — enamel on the outside and dentin underneath.
Each tooth is covered with hard protective layers — enamel on the outside and dentin underneath.
Enamel is the strongest layer that acts as a shield. It is very dense in minerals and contains no nerves. This means it perfectly isolates the tooth nerves and prevents sensitivity.
Dentin is also a hard mineralized layer, but it’s more fragile. It contains thousands of tiny channels called dentinal tubules. Each square millimeter of dentin has between 20,000 and 65,000 tubules (as shown below). These tubules run through the dentin and connect directly to the tooth’s nerves.
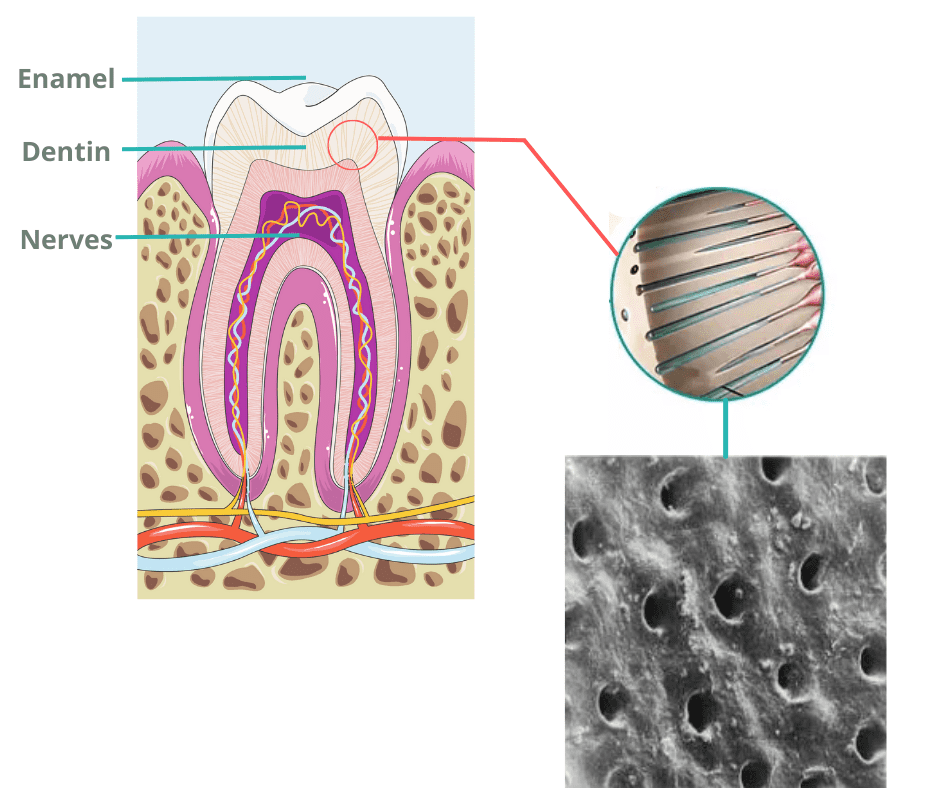
For these reasons, dentin isn’t designed to protect the nerves from the harsh conditions in the mouth.
So when the enamel wears away and exposes the dentin, the inevitable result is tooth sensitivity — especially to cold, hot, sweet, or acidic foods and drinks.
That’s because these triggers can easily travel through the dentinal tubules and reach the nerves, causing sharp pain or discomfort.
What Causes Dentin Exposure?
Several factors can lead to exposed dentin, including:- Receding gums
- Tooth wear (attrition, erosion, or abrasion)
- Cracks or trauma
- Most commonly, untreated tooth decay or cavities
Why should tooth sensitivity never be ignored?
Increased sensitivity is your body’s way of telling you that something is wrong with your tooth.Healthy teeth with sound enamel should never cause pain when biting, chewing, or eating hot or cold foods.
If they do, it often means something is actively damaging your teeth — and the longer you wait, the worse the damage can become.
Potential Causes of One-Tooth Sensitivity
Anything that exposes the dentin and underlying nerves to the outside harsh oral environment can lead to tooth sensitivity.Here are the most common causes:
1. Tooth Decay
If your tooth suddenly becomes sensitive, decay is one of the most likely reasons.
Tooth decay is so common. Nearly 90% of adults aged 20–64 have experienced it at some point. It’s also the main cause of dental pain.
At first, tooth decay sneaks in and progresses slowly. It gradually breaks down the outer protective layers of your tooth — starting with enamel and reaching the dentin.
When decay is still limited to the enamel, you may not feel anything at all. It often goes unnoticed in its early stages.
But once it reaches the dentin and creates a hole or cavity, you’ll likely start to notice sensitivity issues.
If your tooth hurts but you don’t see a cavity, it might be hidden in a hard-to-see spot, like between your teeth.
Only your dentist can help you detect it with a dental exam and X-rays.
2. Gum Recession on a Single Tooth
Gum recession is another common cause of sensitivity in one tooth — especially in older adults. As we age, the risk of our gums pulling away from the teeth increases. And when gums recede, sensitivity often follows.
Why?
When the gums pull away, they expose the tooth’s root surface. Unlike the crown of the tooth, roots don’t have enamel.
They’re covered only by dentin. And, as we’ve seen, dentin contains thousands of microscopic tubules that connect directly to the nerves.
Once exposed, these areas become more sensitive and vulnerable to outside triggers.
Exposed roots are also more susceptible to other issues like root decay and wear, which can make the sensitivity even worse.
3. Tooth Wear
Tooth wear happens when certain factors gradually strip minerals from the teeth, weakening and thinning the enamel and dentin over time.
One of the most common causes is bruxism — the habit of grinding or clenching your teeth, often during sleep.
Another major factor is high acidity in the mouth, which can dissolve tooth minerals. This acidity can come from overconsumption of sugary or acidic drinks, frequent acid reflux, or repeated vomiting.
Aggressive brushing or using an abrasive toothpaste can also wear out your enamel and dentin over time.
Tooth wear typically affects multiple teeth rather than just one. But in some cases, one tooth might wear down rapidly and more noticeably than the others.
4. Dental Crowding
Dental crowding can also be a potential reason — especially if one tooth sits higher than the rest of your teeth.
When this happens, the chewing pressure isn't evenly distributed across all teeth. Instead, it concentrates on that single, protruding tooth.
This can irritate the tooth’s nerve and strain the supporting tissues, including the surrounding bone and ligaments. The sign of this is sensitivity and pain, especially when biting down.
5. Fracture
A cracked or chipped tooth can also cause sudden sensitivity.
The tricky part about these injuries is that they can be too tiny at first and hard to see.
Over time, as they widen and deepen, they can create an opening for bacteria and saliva to reach the inner layers of the tooth and nerves.
These types of injuries should be treated as soon as possible. They don’t heal on their own and can worsen quickly, leading to serious complications like infection, abscess, or even tooth loss.
6. A Leaking Dental Filling or Crown
If a filling or crown doesn’t fit firmly, it can leave small gaps between the restoration and the tooth. These "BAD" gaps can be an open gateway for bacteria, food particles, and saliva to enter.
This can damage the underlying dentin and nerves, leading to sensitivity. You might also notice signs like bad breath, a foul taste in your mouth, gum irritation near the tooth, or visible wear on the restoration.
These gaps not only trigger sensitivity but can also become hiding spots for bacteria, increasing the risk of cavities and gum infection.
7. Recent Professional Cleaning
It’s common to feel some tooth sensitivity after a deep dental cleaning — especially if you had a lot of tartar buildup.
That’s because the buildup that was covering and protecting parts of your teeth is no longer there. So, it's normal for your teeth to feel more sensitive for a short time.
The good news is that this type of sensitivity is temporary and usually goes away within a week.
However, if the pain lasts longer than expected or gets worse, it’s best to have it checked by your dentist. It could be a sign of another underlying issue.
How to Stop Sensitivity in One Tooth (In 2 Steps)
The first step in treating tooth sensitivity is knowing what's really behind it.That’s because sensitivity usually improves once the underlying cause is fixed.
There are some things you can do on your own at home, but others require a dentist’s help.
For example, conditions like cavities, cracks, or tooth wear are irreversible — they won’t heal on their own and need professional treatment.
That’s why it’s always a good idea to see your dentist to rule out these conditions first.
Next come desensitizing treatments designed to make teeth less sensitive to pain.
1. Removing the Root Cause:
Depending on the specific cause, this can include:
- Correcting brushing technique: If you’ve been brushing too hard or using a stiff toothbrush, switch to a gentler technique and a softer brush. This alone can prevent further damage and reduce sensitivity.
- Limiting acidic and sweet foods and drinks: These can strip minerals from your teeth and make sensitivity worse.
- Fixing fillings or treating tooth decay: If your filling or crown is leaking, repairing it is the only way to stop the sensitivity. Similarly, cavities need professional treatment as soon as possible — they won’t heal on their own, and waiting can only make things worse.
- Treating tooth damage: If your tooth is cracked, broken, or worn down, it should be restored to protect the nerves and prevent further complications.
2. Making the Tooth Insensitive:
Once the root causes have been delt with, the next step is to reduce sensitivity with some home treatments.
1. Desensitizing Toothpastes
Toothpastes designed for sensitive teeth work in two main ways:
- Numbing the tooth:
The most common active ingredient is Potassium Nitrate, which helps numb the nerve endings inside the tooth that send pain signals.
Examples include Sensodyne Pronamel and Colgate Sensitive Prevent & Repair. - Sealing the exposed dentinal tubules:
Other toothpastes work by filling and sealing the tiny exposed tubules in the dentin, preventing triggers from reaching the nerves.
Some ingredients to look for include Novamin, Stannous Fluoride, and Hydroxyapatite.
When used regularly, these toothpastes form a protective layer over the exposed dentin and reduce sensitivity.
Great options include Crest Pro-Health Toothpaste, Sensodyne Repair and Protect, and Parodontax Gum Breath & Sensitivity.
2. Remineralizing Products:
Some products help remineralize your teeth — meaning they restore minerals your teeth have lost.
These products are meant to supplement your daily brushing routine, not replace it.
Remineralizing products are available in different forms, such as mouthwashes, gels, and creams. Always read and follow the instructions on the label carefully.
Here are some good options:
These products are meant to supplement your daily brushing routine, not replace it.
Remineralizing products are available in different forms, such as mouthwashes, gels, and creams. Always read and follow the instructions on the label carefully.
Here are some good options:
- CariFree Gel – Fluoride-free and based on nano-hydroxyapatite
- ROCS Remineralizing Gel – Contains calcium, phosphorus, xylitol, and other minerals
- MI Paste – A dental cream containing Recaldent and fluoride
Tip
For quick and effective relief, apply a small amount of the product (toothpaste or gel) to your teeth and leave it on for at least 3 minutes. Then, spit out the excess, but do not rinse or eat for 30 minutes afterward.When to See Your Dentist
As we've said, it’s best to see your dentist early to rule out any serious dental conditions.Don’t delay making an appointment—especially if your sensitivity is severe, persists, or doesn’t improve with home treatments.
Professional options may include:
- Stronger Desensitizing Agents: Dentists can apply products with higher concentrations of desensitizing ingredients than those found in over-the-counter options. These provide faster and more effective relief.
- Sealing the Exposed Dentin: If a large area of dentin is exposed, your dentist may use a bonding agent or sealant to cover sensitive spots and protect the tooth.
- Topical Fluoride Applications: High-concentration fluoride gels or varnishes can be applied to remineralize teeth, making them stronger and more resistant to acid attacks.
- Spotting and Treating Tooth Decay: If tooth decay is suspected, your dentist may take an X-ray to get a better look at the tooth. Once the cavity is treated, the sensitivity should go away.
- Gum Treatment: If receding gums are the culprit, ask your dentist about gum grafting. This procedure covers exposed roots, reducing sensitivity and preventing further issues like root decay and wear.
Takeaway
Tooth sensitivity — whether in one tooth or several — should never be ignored.Healthy teeth shouldn’t hurt when you eat or drink. When sensitivity appears, it’s often a warning sign of an underlying dental issue that’s actively damaging your tooth.
Don’t wait to see your dentist!
The sooner the problem is diagnosed, the simpler and more effective the treatment will be.