5 Symptoms of Gingivitis You Might Not Know
 Gingivitis, or gum inflammation, is the earliest stage of gum disease. The good news? If you catch it early, you can easily reverse it and restore your gum health with simple home care.
Gingivitis, or gum inflammation, is the earliest stage of gum disease. The good news? If you catch it early, you can easily reverse it and restore your gum health with simple home care.
But if left untreated, gingivitis can progress into periodontitis—an advanced and irreversible stage where the bone and tissues supporting your teeth start to break down. Unfortunately, once that happens, the damage can’t be undone.
In this post, we’ll go over 5 symptoms of gingivitis so you can recognize the signs early and prevent it from turning into something more serious.
In this article:
1. Inflammation Signs – Red, Swollen, and Bleeding Gums
2. Teeth and Gum Sensitivity
3. Changes in Gum Texture and Consistency
4. Plaque and Tartar Buildup
5. Bad Breath (Halitosis)
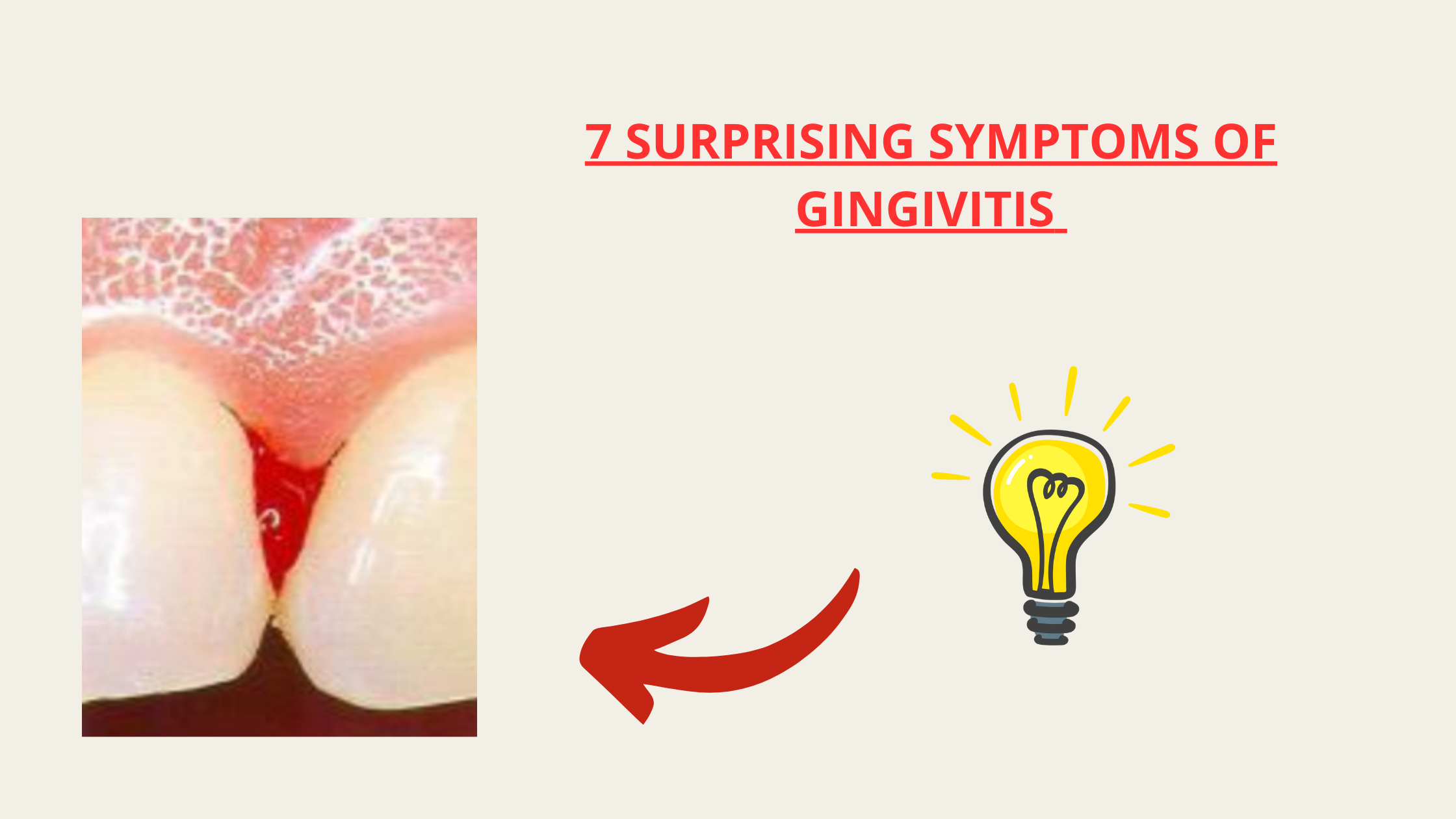
1. Inflammation Signs – Red, Swollen, and Bleeding Gums
These are the first signs you will likely notice. Inflammation is your body’s natural defense against the bacteria in plaque buildup.At first, the inflammation might be so mild that you don’t even notice it. But as it worsens, your gums will start to turn red instead of their normal pale pink. The first areas affected are usually along the gum line and between the teeth. In the more diffuse forms, the redness can affect all of your gums.

Swelling is another sign of gingivitis. It may be subtle at first or, in severe cases, cause the gums to puff up so much that they cover more than half of your teeth.

Furthermore, healthy gums don’t bleed when you brush or floss. If you see blood when cleaning your teeth, it’s a clear sign of gingivitis or gum inflammation.
Tips
Even if your gums feel sore or bleed, don’t stop your oral hygiene routine. With consistency, the inflammation will gradually subside, and your gums will heal.
- Brush at least twice a day for two full minutes. Use gentle circular motions, brushing from the gum line toward the tooth.
- Floss once a day, preferably before bed, to remove plaque and food particles from between your teeth.
- Chew sugar-free gum between meals to stimulate saliva production, which naturally helps clean your teeth.
- See your dentist if your symptoms don’t improve despite your efforts at home.
2. Teeth and Gum Sensitivity
Gingivitis doesn’t always cause pain or sensitivity. It often develops silently without noticeable symptoms. However, if the inflammation is too severe, sore and tender gums are common signs.You may feel discomfort, especially when brushing, flossing, or eating hard or crunchy foods.
Tips to Soothe Sensitivity
- Pick a soft-bristled toothbrush and brush gently.
- Avoid harsh horizontal strokes when brushing, as they can be damaging. Instead, use gentle circular motions.
- Go easy with floss at first and avoid toothpicks. As your gums become healthier, the soreness will gradually disappear.
- Apply a soothing oral gel like Orajel, which contains numbing ingredients to relieve discomfort. Simply apply it directly to the painful areas.
3. Changes in Gum Texture and Consistency
Healthy gums are firm, have a natural “orange-peel” texture, and fit snugly around your teeth.But with gingivitis, things start to change. Your gums may lose their texture, becoming shiny and smooth instead. They might also feel looser and less attached to your teeth due to swelling (edema).
To check these changes, gently press your gum with your index finger.
- If it springs back to its original position, your gums are firm and healthy.
- If it stays pressed in or seems out of place, it's a sign that your gums are looser and less attached.
An uneven gum line is another sign to look for. Instead of a smooth, regular shape, gingivitis may cause some areas to appear higher or lower than others.
Solution
As long as you're still in the gingivitis stage, these changes aren’t permanent. With consistent oral hygiene, your gums can return to their natural, healthy state.
4. Plaque and Tartar Buildup
Plaque is the main culprit behind gum disease. If your gums are inflamed, there’s a high chance plaque buildup is the reason.Plaque is a soft, whitish film full of bacteria that constantly forms on your teeth. If it’s not removed regularly, harmful bacteria multiply and can travel below the gum line, leading to inflammation and damage.
Take a toothpick and gently run it along the gum line. If you see whitish material sticking to it, that’s bacterial plaque.
While plaque-induced gingivitis is the most common type, other less common forms can be triggered by allergies, viral infections, or autoimmune diseases.
Tips to Control Plaque and Tartar
- Proper, regular tooth brushing and flossing are the basis of plaque control. No mouthwash or product can replace them.
- Tartar (hardened plaque) can’t be removed at home. It requires a professional dental cleaning (scaling), where your dentist uses special tools to eliminate it.
- You can supplement flossing and brushing with mouthwash to reduce harmful bacteria left behind.
5. Bad Breath (Halitosis)
Bad breath isn’t always constant, but many people with gum disease experience it.I’m not talking about morning breath or the temporary smell after fasting—this is about chronic bad breath that lingers or comes back even after thorough brushing and flossing.
If this sounds familiar, it’s important to identify the real cause. It could be untreated cavities, infections, or gum disease.
If gum disease is the culprit, treating it can completely refresh your breath.
Solutions to address bad breath
- Find and address the root cause. A dental checkup can help rule out cavities or infections.
- Clean your tongue daily. This is where most odor-producing bacteria live, so using a tongue scraper or brushing it will help.
- Stay hydrated and chew sugar-free gum. This helps prevent dry mouth, which is a leading cause of bad breath.
- Use a mouthwash designed to fight bad breath. Choose one that contains zinc (such as zinc chloride or zinc lactate), as these ingredients have been shown to cancel out odor-causing compounds.