Mouth Sores in Leukemia: What They Look Like and Why They Happen
 Leukemia is a type of blood cancer that causes the bone marrow to start producing large numbers of immature and abnormal white blood cells. This overproduction often comes at the expense of other essential blood cells.
Leukemia is a type of blood cancer that causes the bone marrow to start producing large numbers of immature and abnormal white blood cells. This overproduction often comes at the expense of other essential blood cells.
As a result, the bloodstream becomes flooded with abnormal white cells, while the levels of red blood cells, platelets, and healthy immune cells drop.
Oral symptoms are very common in leukemia. In fact, up to 80% of people with leukemia develop signs in the mouth, including painful sores, unexplained bleeding, or swollen gums. These oral signs can even be the first signs of the disease.
Nonetheless, mouth symptoms are usually accompanied by general signs, like swollen lymph nodes in the neck, fever, fatigue, malaise, and pallor.
Below, we break down how leukemia can cause mouth sores, what these lesions look like, as well as other oral warning signs.
In this article...
1. Leukemic mouth sores: why do they happen and what do they look like?
2. Other mouth symptoms of leukemia
3. How are leukemic mouth sores managed?
Leukemic mouth sores: why do they happen and what do they look like?
While leukemia starts in the bone marrow, if left untreated, cancer cells will eventually spread and affect other parts of the body, including the lymph nodes, spleen, kidneys, and the mouth.Why and how is the mouth affected? One reason is the direct infiltration of abnormal cancer cells, especially in the gums. This appears as severe and diffuse gum swelling, known as gingival hyperplasia. The gums can enlarge to the point of covering all the teeth.
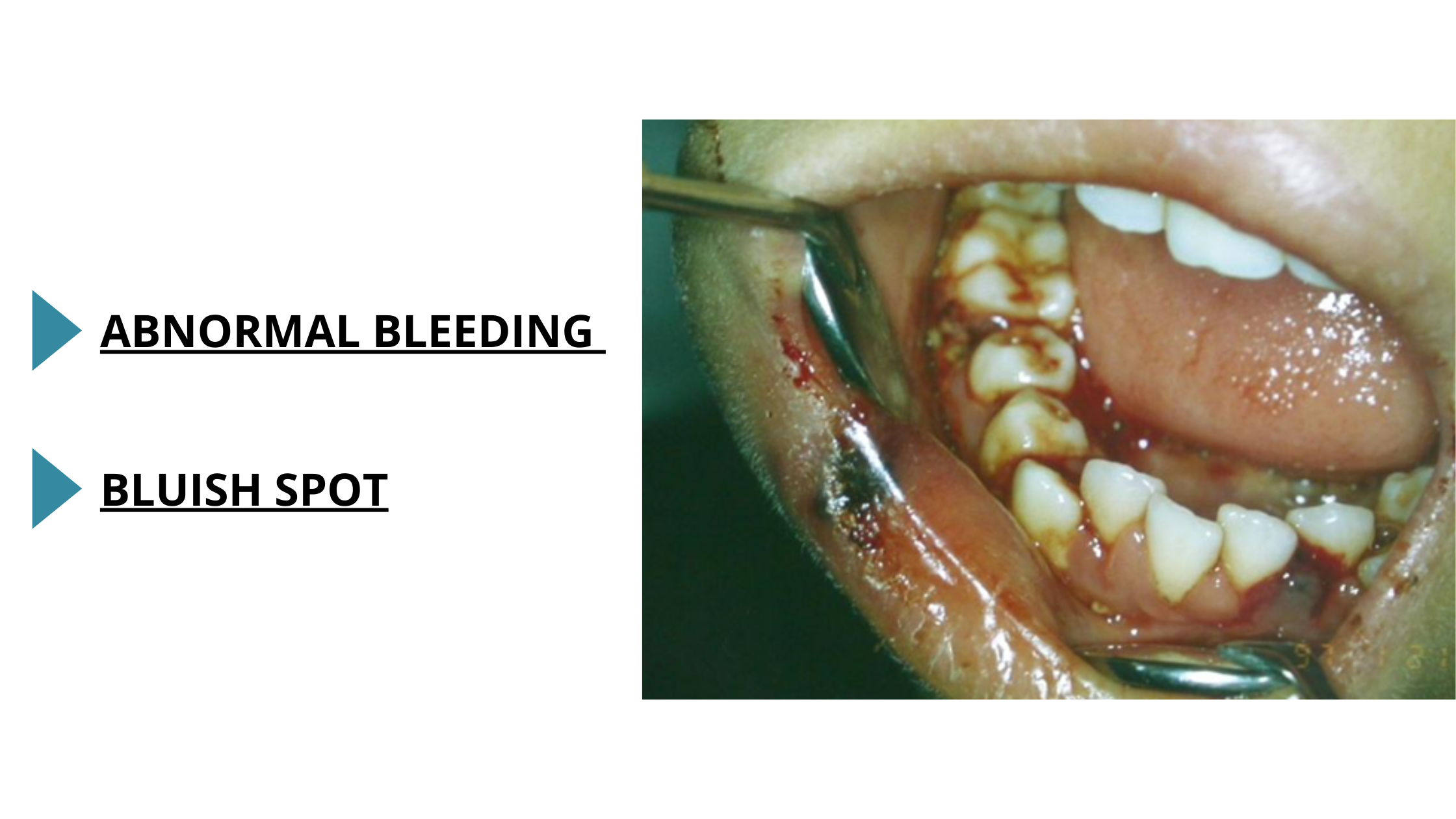
In fact, swollen and bleeding gums are the most common oral manifestations of leukemia. They should be seen as a red flag, especially when associated with other general signs such as fever, swollen lymph nodes, pallor, and fatigue.

The second way leukemia can affect the mouth is by weakening the immune system.
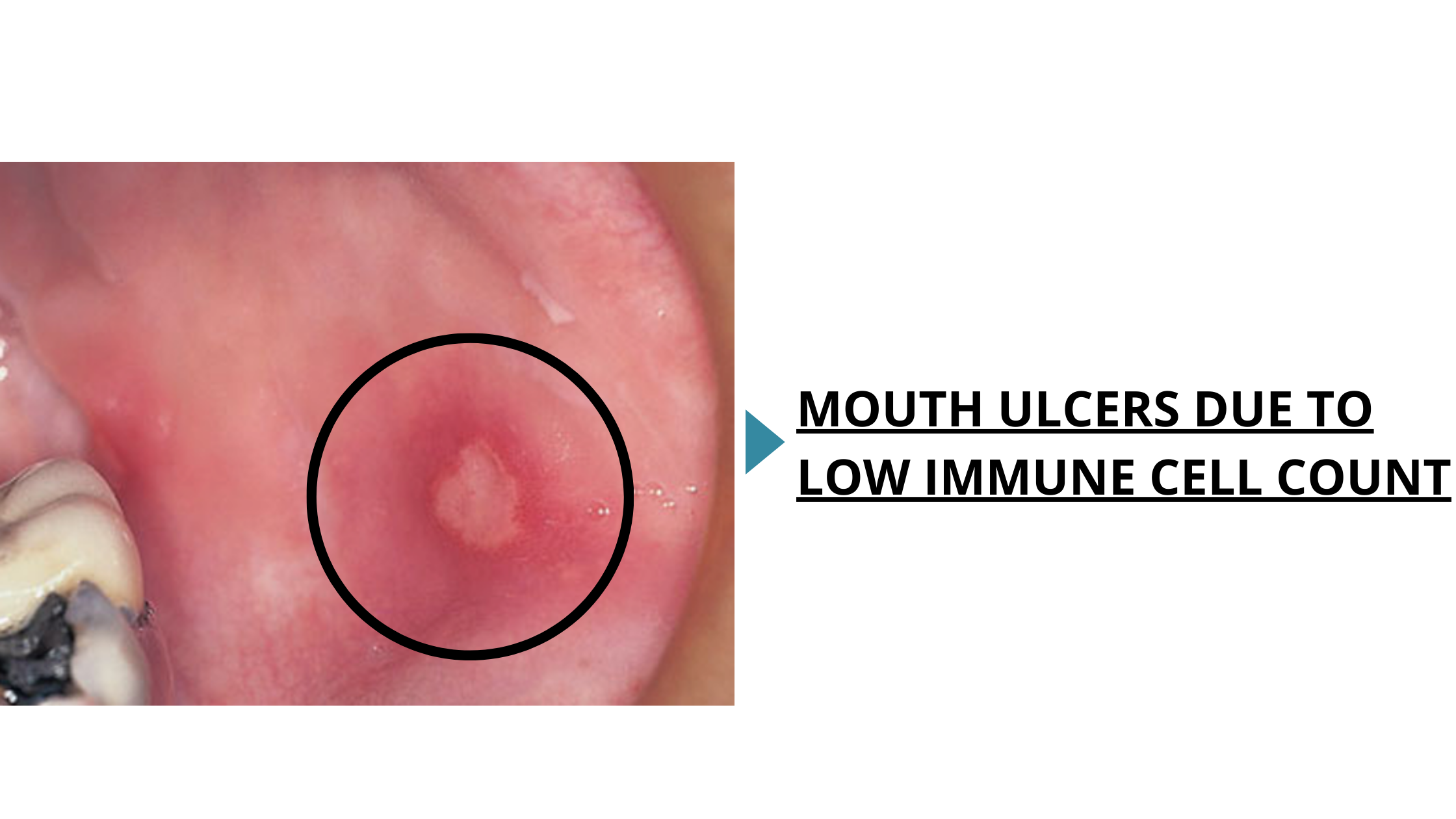
A lower count of healthy immune cells, combined with an increased number of abnormal white blood cells, makes it harder for the body to fight bacteria, yeasts, and viruses that it used to handle easily. This often leads to:
- Widespread mouth inflammation: The oral lining becomes thinner, red, and tender.
- Open sores or ulcers: Severe mouth ulcerations that recur frequently are common. They may appear as single or multiple sores, with a grayish necrotic center and red borders.
- Oral thrush (candidiasis): Caused by an overgrowth of the yeast Candida albicans. Symptoms include creamy white patches on the tongue or other oral surfaces, along with burning, soreness, and redness.
- Severe gum disease (necrotizing ulcerative gingivitis): A weakened immune system allows aggressive bacteria to grow and invade the gums. This can lead to painful grayish-white ulcers and severe destruction of the tissues that support the teeth.
Other mouth symptoms of leukemia
Aside from affecting immune cells, leukemia also affects the body’s ability to produce other major blood cells.Often, red blood cell levels are too low, leading to anemia. In the mouth, this causes the gums and oral lining to appear pale, while the tongue may become red, swollen, and sore.
Platelets, which are essential for blood clotting and stopping bleeding, also drop too low. This can result in unexplained and repeated mouth bleeding, easy bruising, and the appearance of small red, purple, or bluish spots inside the mouth due to internal bleeding.
Other oral symptoms may be related to leukemia itself or to its treatment, typically chemotherapy. These include dry mouth, widespread mouth inflammation and soreness, difficulty opening the mouth fully, and pain in the jaw and jaw joints.
How are leukemic mouth sores managed?
Mouth sores related to leukemia are generally managed in a similar way to common canker sores. This mainly involves:- Proper oral hygiene: Using a soft-bristle toothbrush.
- Topical numbing agents: Containing xylocaine or benzocaine to relieve pain.
- Topical corticosteroids: For more severe or persistent ulcers.
- Mouth rinses: With chlorhexidine 0.12%, baking soda, or salt water to keep the mouth clean and control inflammation.
- Diet: A soft diet and avoiding foods that may worsen pain or sores, such as hot, spicy, acidic, or crunchy foods.
Antimicrobials are needed only when there is an underlying infection. For example:
- Antibiotics for bacterial infections.
- Antivirals for viral infections, such as cold sores.
- Antifungals used to treat yeast infections, such as oral thrush.